In cardiology, there is a concept of deviations that do not cause harm to human health, and therefore are considered by doctors as a variant of the norm. One such phenomenon is supraventricular crest syndrome. When faced with a diagnosis for the first time, patients show anxiety and look for ways to overcome the problem. Doctors agree that the phenomenon does not pose a threat to life and health, and therefore does not require treatment or correction. The syndrome occurs more often in children and is caused by individual characteristics of the heart structure.
Causes of the syndrome
Speaking about the etiology of the phenomenon, experts come to the conclusion that it is impossible to identify a number of reasons leading to its development. First of all, it should be noted that pectinate syndrome is not a disease. It is determined by the physiological characteristics of the structure of the human heart.
The main organ of the circulatory system consists of four chambers. Entering the heart, blood enters the right atrium, and then into the right ventricle. Passing through the valve and entering the lungs, where gas exchange occurs, the blood flow returns to the left atrium, then to the left ventricle and from there it goes to the main artery - the aorta.
The right ventricle, in which the so-called scallop is located, is the beginning of the pulmonary circulation. It is one of the four chambers of the heart. It is separated from the left atrium by the interventricular grooves, and from the atrium of the same name it is separated by the coronary groove.
The shape of this cardiac chamber is an irregular pyramid, consisting of three sides, with a flat rear and convex anterior and internal walls, one of which forms a septum with the left ventricle.
Being a hollow formation, this chamber consists of two sections, one of which (the anterior, so-called arterial cone) is narrow, and the second (posterior) is wider.
There is a valve between the atrium and the ventricle that prevents the backflow of blood.
In the right ventricle, as well as in the left, there are special structures that belong to the conduction system of the heart and are responsible for coordinating the work of its different parts. These formations include fibers, knots and bundles - it is the latter that form the so-called comb. Deviations in its work, which, however, are a variant of the norm, cause a phenomenon called supraventricular crest syndrome.
Sometimes the described condition is mistakenly called pancreatic scallop syndrome; it is diagnosed quite often in children and much less often in adult patients.
Pathogenesis
A child’s cardiogram has its own physiological and pathological characteristics. It is worth saying that changes in it depend on the age of the patient, when, as for an adult, there is a single norm. Among the “children’s” features we can list the shortening of the PQ and QT intervals, the GRS complex also narrows, and sometimes arrhythmia can be observed, while maintaining a positive P wave.
Pathophysiologists explain these phenomena by the fact that a child’s heart beats faster than an adult’s. Action potentials shift and layer on top of each other. Or the excitation does not have time to cover all cardiomyocytes before contraction - this is how artifacts appear on the ECG.
Supraventricular crest syndrome is one such physiological phenomenon. Its presence does not indicate any pathology, so doctors do not focus attention on it and over time the child outgrows it.
Characteristic signs
Scalloping syndrome has no pronounced external symptoms; internally it also does not cause any pain or discomfort. It is detected during a cardiogram.
In adults
The syndrome in adult patients (persons over eighteen years of age) is diagnosed extremely rarely. This is due to the fact that over the years, the cardiac structures become fully formed and function stably. Nevertheless, scallop syndrome is still recorded on the ECG in adults in rare cases. Apart from the fact that the phenomenon is recorded on thermal paper during the research process, it does not manifest itself in anything else.
In children
In a child or teenager, deviations of this kind are recorded quite often and cause unnecessary fears among parents. As in the case of adult patients, such conditions do not cause pain or persistent discomfort at rest. Some patients may experience the following symptoms:
- cardiopalmus;
- fast fatiguability;
- chest pain after significant physical activity.
If the syndrome is present, the child's ECG shows some deviations from the norm, which are its only confirmation.
Diagnostics
The only way to see supraventricular crest syndrome at the moment is an ECG. This method is available in any hospital or clinic. An electrocardiogram is a graphical record of a sequential change in electrical potentials appearing in cardiomyocytes.
In young children, the nervous system is not yet fully “calibrated”, so it is possible to register various abnormalities on the ECG. For example, this may be a change in the configuration and amplitude of the teeth in the chest leads. But in order to confirm the presence of pathology, it is not enough to have the result of one study.
Children whose pediatrician suspects the presence of disturbances in the functioning of the heart are registered with a dispensary for this disease and are required to undergo examination by a cardiologist once a year or every six months. This allows you to observe the dynamics of the development of the process, as well as timely notice the deterioration of the condition.
Diagnosis and treatment
To make a decision on possible treatment methods for a particular disease, a specialist sends the patient for a comprehensive examination.
Diagnostics
Only one method of instrumental examination can provide a reliable picture when diagnosing the described condition - an electrocardiogram. The study is usually carried out in case of complaints about a concomitant disease or for preventive purposes. Thus, abnormalities in the functioning of the supraventricular structures are discovered by chance. During inspection and simple listening, violations of this kind are not recorded.
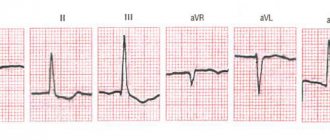
Since the syndrome is predominantly found in children, it makes sense to take a closer look at what ECG signs are used to conclude its presence.
- Shorter line length of PQ, QT intervals.
- Reduced width of the ventricular complex.
- Deviation of the electrical axis of the heart to the right.
- The difference between heartbeats is more than ten percent.
- Predominance of the right ventricle over the left.
- Change in the amplitude of the teeth (overestimation).
- Negative T waves in the V1-V3 pattern.
- Physiological alternation of the ventricular complex.
- Splitting of the QRS complex in lead V4.
- Deformation of the ventricular complex (on the recording it looks like jaggedness of the ascending limb of the S wave or as a narrow one, with a small amplitude r' in the V3R - V5R and V1 scheme).
The above features are a variant of the norm for children. Some of them are caused by the physiologically small (for a given age optimal) thickness of the chest wall, others by the location of the organ in the chest. When it comes to an adult patient with some of the above signs that appear on the cardiogram, there are individual characteristics of the functioning of the heart.
Since sometimes the syndrome can cause discomfort after heavy physical exertion, it makes sense to talk about differential diagnosis. So, often unpleasant sensations caused by a malfunction of the pancreas, stomach, and so on can be mistaken for heart pain.
Treatment
Since the condition in question is not a disease and does not pose a threat to human health and life, it does not require treatment or correction.
Suspicious patients, especially when it comes to the parents of a child who has ECG symptoms of supraventricular crest syndrome, often insist on treatment and medical care. In such cases, vitamin-mineral complexes and some other drugs may be prescribed to prevent diseases and strengthen the cardiovascular system.
Adult patients may be at risk of developing cardiovascular diseases in the following cases:
- hereditary predisposition;
- presence of bad habits (smoking, alcohol abuse);
- increased blood cholesterol levels;
- high blood pressure;
- sedentary lifestyle;
- excess weight.
In such cases, it is worth taking care of prevention, for which it is recommended to consult a cardiologist. You can take the following medications:
- In their pure form, vitamins are A, B1, B6, E, C, P, F, Q10.
- In their pure form, minerals are potassium, magnesium, calcium, phosphorus, selenium.
- "Ascorutin".
- "Asparkam."
- Other vitamin and mineral complexes, balanced in composition and prescribed if there are reasons for the development of diseases.
- Prevention includes lifestyle modification, proper nutrition, moderate physical activity and the absence of bad habits.
ECG of a child. Peculiarities
25.09.2011 34285
Features of a children's cardiogram.
Atrial complex (P wave). In children, as in adults, the P wave is small (0.5-2.5 mm), with maximum amplitude in standard leads I and II. In most leads it is positive (I, II, aVF, V2-V6), in lead aVR it is always negative, in leads III, aVL, V1 it can be smoothed, biphasic or negative. In children, a slightly negative P wave in lead V2 is also allowed.
The greatest features of the P wave are observed in newborns, which is explained by increased electrical activity of the atria due to the conditions of intrauterine circulation and its postnatal restructuring. In newborns, the P wave in standard leads, compared to the size of the R wave, is relatively high (but in amplitude no more than 2.5 mm), pointed, and sometimes may have a small notch at the apex as a result of non-simultaneous coverage of the right and left atria by excitation (but not more than 0 .02-0.03 s). As the child grows, the amplitude of the P wave decreases slightly. With age, the ratio of the size of the P and R waves in standard leads also changes. In newborns it is 1:3, 1:4. as the amplitude of the R wave increases and the amplitude of the P wave decreases, this ratio by 1-2 years decreases to 1:6, and after 2 years it becomes the same as in adults - 1:8; 1:10.
The smaller the child, the shorter the duration of the P wave. It increases on average from 0.05 s in newborns to 0.09 s in older children and adults.
Features of the PQ interval in children . The duration of the PQ interval depends on heart rate (the higher the heart rate, the shorter the PQ interval) and age. As children grow, there is a noticeable increase in the duration of the PQ interval: on average from 0.10 s (not more than 0.13 s) in newborns to 0.14 s (not more than 0.18 s) in adolescents and 0.16 s (not more than 0.20 s) in adults.
Features of the QRS complex in children . In children, the time of ventricular excitation coverage (QRS interval) increases with age: on average from 0.045 s in newborns to 0.07-0.08 s in older children and adults (Appendix Table 3).
Wave Q. In children, as in adults, it is recorded inconsistently, more often in II, III, aVF, left chest leads (V4-V6), less often in I and aVL leads. In lead aVR, a deep and wide Q wave of the Qr type or QS complex is detected. In the right chest leads, Q waves, as a rule, are not recorded. In young children, the Q wave in standard leads I and II is often absent or weakly expressed, and in children of the first 3 months - also in V5, V6. Thus, the frequency of registration of the Q wave in various leads increases with the age of the child.
The amplitude of the Q waves in most leads is small (1-3 mm) and their size changes little with the age of the child, except for two leads - standard III and aVR.
In standard lead III in all age groups, the Q wave is also small on average (2 mm), but can be deep and reach up to 5 mm in newborns and infants; in early and preschool age - up to 7-9 mm and only in schoolchildren it begins to decrease, reaching a maximum of 5 mm. Sometimes, in healthy adults, a deep Q wave is recorded in standard lead III (up to 4-7 mm). In all age groups of children, the size of the Q wave in this lead can exceed the size of the R wave.
In lead aVR, the Q wave has a maximum depth, which increases with the age of the child: from 1.5-2 mm in newborns to 5 mm on average (with a maximum of 7-8 mm) in infants and at an early age, up to 7 mm on average (with a maximum of 11 mm) in preschool children and up to 8 mm on average (with a maximum of 14 mm) in schoolchildren. The duration of the Q wave should not exceed 0.02-0.03 s.
R wave. In children, as in adults, R waves are usually recorded in all leads, only in aVR they can be small or absent (sometimes in lead V1). There are significant fluctuations in the amplitude of the R waves in various leads from 1-2 mm to 15 mm, but the maximum value of the R waves in standard leads is up to 20 mm, and in the chest leads - up to 25 mm. The amplitude of the R waves in different leads depends on the position of the electrical axis of the heart (it is important to evaluate the ratio of the sizes of the R and S waves in different leads), and therefore changes in children of different age groups. The smallest magnitude of R waves is observed in newborns, especially in the strengthened unipolar and chest leads. However, even in newborns, the amplitude of the R wave in standard lead III is quite large, since the electrical axis of the heart is deviated to the right. After the 1st month, the amplitude of the RIII wave decreases, the magnitude of the R waves in the remaining leads gradually increases, especially noticeably in the II and I standard and in the left (V4-V6) chest leads, reaching a maximum at school age.
With a normal position of the electrical axis of the heart, high R waves with a maximum of RII are recorded in all limb leads (except aVR). In the chest leads, the amplitude of the R waves increases from left to right from V1 (r wave) to V4 with a maximum of RV4, then decreases slightly, but the R waves in the left chest leads are higher than in the right ones. Normally, in lead V1, the R wave may be absent and then a QS-type complex is recorded. In children, the QS type complex is also rarely allowed in leads V2, V3.
In newborns, electrical alternans is allowed - fluctuations in the height of the R waves in the same lead. Variants of the age norm also include respiratory alternation of ECG waves.
In children, thickening, notching, and splitting are often found on the R (sometimes S) waves. Their presence is unimportant if they are detected only in one lead, in the transition zone or on low-voltage waves. The degree of their significance increases if they are located close to the top of the waves, which have a sufficiently large amplitude, and are detected in several leads. In such cases, they speak of a violation of the propagation of excitation throughout the myocardium of a particular ventricle.
In children, deformation of the QRS complex in the form of the letters “M” or “W” in the III standard and V1 leads is often found in all age groups, starting from the neonatal period. In this case, the duration of the QRS complex does not exceed the age norm. Splitting of the QRS complex in healthy children in V1 is referred to as “slow excitation syndrome of the right supraventricular crest” or “incomplete block of the right bundle branch.” The origin of this phenomenon is associated with the excitation of the hypertrophied right “supraventricular scallop” located in the region of the pulmonary cone of the right ventricle, which is the last to be excited. The position of the heart in the chest and the electrical activity of the right and left ventricles changing with age are also important.
The internal deviation interval (time of activation of the right and left ventricles) in children changes as follows. The activation time of the left ventricle (V6) increases from 0.025 s in newborns to 0.045 s in schoolchildren, reflecting an accelerated increase in the mass of the left ventricle. The activation time of the right ventricle (V1) practically does not change with the age of the child, amounting to 0.02-0.03 s.
In young children, there is a change in the localization of the transition zone (thoracic lead, in which the R and S waves of equal amplitude are recorded) due to a change in the position of the heart in the chest (rotations around the axes) and a change in the electrical activity of the right and left ventricles. In newborns, the transition zone is located in lead V5, which characterizes the dominance of the electrical activity of the right ventricle. At the age of 1 month, the transition zone shifts to leads V3, V4, and after 1 year it is localized in the same place as in older children and adults - in V3 with vibrations V2-V4. Together with an increase in the amplitude of the R waves and deepening of the S waves in the corresponding leads, and an increase in the activation time of the left ventricle, this reflects an increase in the electrical activity of the left ventricle.
S wave . In children, as in adults, the amplitude of the S waves in different leads varies widely: from none in a few leads to a maximum of 15-16 mm, depending on the position of the electrical axis of the heart. The amplitude of the S waves changes with the age of the child. Newborn children have the smallest depth of S waves in all leads (from 0 mm to 3 mm), except standard I, where the S wave is quite deep (on average 7 mm, maximum up to 13 mm). This reflects the deviation of the electrical axis of the heart to the right.
In children older than 1 month, the depth of the S wave in the first standard lead decreases and subsequently in all limb leads (except aVR) S waves of small amplitude (from 0 mm to 4 mm) are recorded, the same as in adults. In healthy children, in leads I, II, III, aVL and aVF, the R waves are usually larger than the S waves.
As the child grows, there is a deepening of the S waves in precordial leads V1-V4 and in lead aVR, reaching their maximum value at high school age. In the left chest leads V5-V6, on the contrary, the amplitude of the S waves decreases, often they are not recorded at all. In the chest leads, the depth of the S waves decreases from left to right from V1 to V4, having the greatest depth in leads V1 and V2.
Sometimes in healthy children with an asthenic physique, with a so-called “hanging heart,” an S-type ECG is recorded. In this case, the S waves in all standard (SI, SII, SIII) and chest leads are equal to or exceed the R waves with reduced amplitude. It is believed that this is due to the rotation of the heart around the transverse axis with the apex posteriorly and around the longitudinal axis with the right ventricle forward. In this case, it is almost impossible to determine the angle ?, so it is not determined. If the S waves are shallow and there is no shift of the transition zone to the left, then we can assume that this is a normal variant. More often, the S-type ECG is determined by pathology.
Variants of the age norm include “comb syndrome”, already mentioned above, i.e. delayed excitation of the right supraventricular crest - widening and jaggedness on the ascending limb of the S wave in lead V1, sometimes V2.
Features of the ST segment in children . Just like in adults, in children the ST segment should be isoelectric, but in a normal ECG the ST segment does not completely coincide with the isoelectric line. The strictly horizontal direction of the ST segment in all leads except III can be considered a pathology. Shifts of the ST segment up and down are allowed up to 1 mm in the limb leads and up to 1.5-2 mm in the chest leads, especially in the right ones. These shifts do not mean pathology if there are no other changes on the ECG. In newborns, the ST segment is often not expressed and the S wave, when reaching the isoline, immediately turns into a gently rising T wave.
Features of the T wave in children . In older children, as in adults, the T waves are positive in most leads (standard I, II, aVF, V4-V6). In standard III and aVL leads, T waves can be smoothed, biphasic or negative; in the right chest leads (V1-V3) are often negative or smoothed; in lead aVR – always negative.
The greatest differences in T waves are observed in newborns. In their standard leads, the T waves are low-amplitude (from 0.5 mm to 1.5-2 mm) or smoothed. In a number of leads, where T waves in children of other age groups and adults are normally positive, in newborns they are negative and vice versa. Thus, in newborns there may be negative T waves in standard I, II, in strengthened unipolar and in the left chest leads; may be positive in standard III and right chest leads. By 2-4 weeks of life, inversion of the T waves occurs, i.e. in the I, II standard, aVF and left chest leads (except V4) they become positive, in the right chest and V4 - negative, in the III standard and aVL - they can be smoothed, biphasic or negative.
In subsequent years, negative T waves persist in lead V4 until 5-11 years, in lead V3 - up to 10-15 years, in lead V2 - up to 12-16 years, although in leads V1 and V2 negative T waves are allowed in some cases and in healthy adults.
After the 1st month of life, the amplitude of the T waves gradually increases, ranging from 1 to 5 mm in standard leads and from 1 to 8 mm in chest leads in young children. In schoolchildren, the size of T waves reaches the level of adults and ranges from 1 to 7 mm in standard leads and from 1 to 12-15 mm in chest leads. The T wave is largest in lead V4, sometimes in V3, and in leads V5, V6 its amplitude decreases.
Features of the QRST complex in children (electric systole). Analysis of electrical systole makes it possible to assess the functional state of the myocardium. Young children, especially in the 1st year of life, are characterized by electrical instability of the myocardium, which is aggravated by any pathological process in the child’s body, which is reflected on the ECG. The following features of electrical systole in children can be identified, reflecting the electrophysiological properties of the myocardium changing with age.
§ Increase in the duration of the QT interval as the child grows from 0.24-0.27 s in newborns to 0.33-0.4 s in older children and adults (Table 4 of the appendix). The indicator reflects the time during which the ventricles are in an electrically active state.
§ With age, the relationship between the duration of the electrical systole and the duration of the cardiac cycle changes, which is reflected by the systolic index (SP). In newborn children, the duration of electrical systole occupies more than half (SP = 55-60%) of the duration of the cardiac cycle, and in older children and adults - 1/3 or slightly more (37-44%), i.e. SP decreases with age.
§ With age, the ratio of the duration of the electrical systole phases changes: the excitation phase (from the beginning of the Q wave to the beginning of the T wave) and the recovery phase, i.e. rapid repolarization (T wave duration). In newborns, more time is spent on recovery processes in the myocardium than on the excitation phase. In young children, these phases take approximately the same time. In 2/3 of preschoolers and most schoolchildren, just like in adults, more time is spent on the arousal phase.
§ Changes in electrical systole in children occur quite often, especially at an early age, reflecting the electrical instability of the myocardium, which is aggravated by any pathological process in the child’s body.
To summarize, we can highlight the following features of children's ECGs:.
1. The heart rate is more frequent, its lability and large individual fluctuations are noted. As the child ages, the heart rate decreases and the heart rate stabilizes.
2. Sinus arrhythmia is often recorded.
3. A decrease in the voltage of the QRS complex waves in the first days of life with a subsequent increase in their amplitude.
4. Deviation of the electrical axis of the heart to the right in newborns with a gradual transition to a vertical position at an early age, and subsequently to a normogram, but a high frequency of vertical position remains even in adolescents and young adults.
5. Shorter duration of intervals, waves, ECG complexes as a result of faster conduction of excitation, with their gradual increase with age.
6. The presence of high, pointed P waves in newborns and young children, followed by a decrease in their amplitude.
7. The frequency of registration of the Q wave in various leads increases with age. The Q wave is most pronounced in aVF and, especially, in standard lead III, where it can be deep, especially in early and preschool age, and exceed ? R wave size.
8. Deformation of the initial ventricular QRS complex in the form of the letters W or M in standard III and V1 leads is often recorded in all age periods - delayed excitation syndrome of the right supraventricular crest.
9. With age, the amplitude of the R and S waves and their ratio in different leads changes, which reflects a change in the position of the heart in the chest and the influence of other factors.
10. Low amplitude of T waves in newborns with its subsequent increase. The presence of negative T waves in the right thoracic (V1-V3) and V4 leads before school age.
11. With age, the activation time of the left ventricle increases (the duration of the interval of internal deviation in V6) and the transition zone shifts from V5 in newborns to V3 (V2-V4) after 1 year of life.
12. With age, the duration of the electrical systole increases, but its duration decreases in relation to the duration of the cardiac cycle (decrease in SP), and the ratio between the phases of the electrical systole also changes towards increasing the duration of the excitation phase.
Some ECG changes (syndromes) in practically healthy children can be attributed to variants of the age norm (transient changes). These include:
- moderately severe sinus tachy- or bradycardia;
- respiratory (electrical) alternation of ECG waves associated with significant excursions of the diaphragm;
- average right atrial rhythm;
- migration of the pacemaker between the sinus node and mid-atrial centers of automaticity in adolescents;
- “crest” syndrome - delayed excitation of the right supraventricular scallop - deformation of the QRS complex in leads III and V1 or jaggedness of the S wave in leads V1 and/or V2.
Possible complications and prognosis
Since the phenomenon under consideration is not a pathology, it has no possible complications. One of the predictions for the development of the syndrome is incomplete blockade of the right bundle branch, but the described condition rarely develops into this form. If a blockade occurs, the process of conducting an electrical impulse is disrupted. As a rule, such a deviation is also considered as a variant of the norm, does not manifest itself and is recorded only during a cardiogram. If there are no concomitant diseases, this condition does not require treatment.
The prognosis for diagnosed supraventricular crest syndrome in the absence of other heart diseases is favorable.
( 1 ratings, average: 5.00 out of 5)
Causes
Scientists have not yet figured out why supraventricular crest syndrome occurs. This anatomical formation is a bundle of muscle fibers that pass through the middle of the right ventricle.
On the electroencephalogram, the syndrome looks like a split QRS wave in the fourth lead. It occurs only in thirty percent of cases of examination of clinically healthy preschool children.
For the appearance of this pathology, the position of the heart and the electrical potentials of the right and left ventricles play a role.
Treatment
Supraventricular crest syndrome does not require treatment as long as it does not cause discomfort to the child. The phenomenon goes away on its own when the patient grows up, and doctor’s intervention can only worsen the situation. But if parents insist on therapy, we can advise taking the following medications:
- Essential fatty acids, such as omega-3. They help reduce the amount of lipids in the blood; in addition, these substances strengthen the walls of blood vessels and improve heart function.
- "Antiox" is a multivitamin preparation containing vitamins A, E, C, as well as microelements. You should not abuse such complexes, because an allergic reaction develops to them.
But it is best not to stuff your child with medications, but to ensure that his diet receives all the necessary substances that are contained in the following products: dietary meat (poultry, veal), fatty fish, olive oil, nuts, fresh vegetables and fruits (preferably seasonal, not greenhouse). If there is sufficient physical activity with this diet, the phenomenon will go away on its own.
Possible complications
Scallop syndrome, although not a pathology, can lead to serious consequences, especially if a person is at risk, for example:
- Is overweight.
- Engaged in work activities that require strong physical exertion.
- Suffers from hypertension and cholesterol disease.
- Hereditarily predisposed to heart pathologies.
- Abuses alcohol.
In this case, an incomplete block of the His bundle may occur, which is characterized by a disruption in the process of conducting an electrical impulse. However, this condition is not accompanied by any serious changes in the myocardium and has virtually no effect on a person’s quality of life.
But if the patient neglects the doctor’s recommendations, leads a passive lifestyle, eats poorly, smokes and abuses alcohol, then pectineus syndrome can provoke a complete transverse block of the His bundle and the development of other cardiac pathologies (for example, a heart attack).
It is important to understand that scallop syndrome is a normal phenomenon that occurs in 60% of children and 10% of adults. And if you lead a healthy lifestyle, then its presence will not affect your overall health. With such a diagnosis, a child may well play sports and play with his peers on the street. The main thing is to constantly monitor his diet so that the body regularly receives all the necessary nutrients. And if you do everything correctly, then after the heart is fully formed (this happens closer to the age of 18), the electrocardiogram readings will return to normal.
Etiology
The supraventricular crest is a bundle of muscle fibers of the heart, which is located in the right ventricle, between its posterior and anterior sections, and takes an active part in the so-called blood circulation. The right branch of the His bundle passes through it, and if its function is disrupted, they speak of the development of pancreatic crest syndrome.
Muscle fibers have the property of contracting. And since in children the heart beats much faster, an ECG reveals such changes. They are within normal limits and do not require third-party intervention, but only if the child has not previously had cardiac pathologies. If they were, then when diagnosing the syndrome, doctors also prescribe an ultrasound and after that it is determined whether the baby requires special treatment or not.
If, during the electrocardiogram, no noise was detected in the child and no complaints are received from him, then there is no need for therapy at all. As soon as the child’s body gets stronger and his heart begins to work like an adult’s, the signs of the syndrome on the ECG will disappear.
In people over 18 years of age, disturbances in the functioning of the supragastric scallop can provoke various pathologies:
- Heart disease.
- Ischemic disease.
- Angina pectoris.
- Arrhythmia, etc.
But it must also be said that in an adult, the presence of this syndrome does not have a negative effect on the functioning of the heart. Therefore, when making such a diagnosis, you simply need to periodically undergo an ECG. Treatment should be carried out only if an electrocardiogram reveals more serious disturbances in the functionality of the organ.