Sick sinus syndrome
(SSSU) is a group of cardiac rhythm and conduction disorders characterized by a decrease in the frequency of electrical signals emanating from the sinus node.
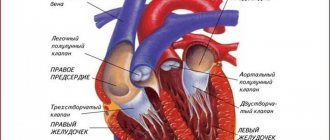
The sinus (sinoatrial) node is a source of electrical excitation and the first-order pacemaker of the heart. It is localized in the wall of the right atrium and produces impulses with a frequency of 60-80 per minute. The SA node is subject to the influence of the ANS (autonomic nervous system) and hormonal systems, this is manifested by changes in rhythm adequate to the needs of the body during physical, psycho-emotional activity, sleep or wakefulness.
With sick sinus syndrome, the SA node loses its leading position in generating the heart rhythm.
SSSU classification
- According to the etiology,
SG dysfunction is divided into primary and secondary, arising against the background of another pathology. - According to the course:
acute, accompanied by hemodynamic disturbances and severe symptoms; paroxysmal (attack-like) and chronic form. Among the chronic ones, a latent form is distinguished, in which there are no symptoms or ECG signs, and the diagnosis is established only after EPI (electrophysiological study); compensated brady- and tachybrady-form with variants of decompensation; permanent brady-form of atrial fibrillation against the background of sick sinus syndrome. - Based on the presence of clinical manifestations,
SU dysfunction can be asymptomatic or symptomatic. Manifestations of the latter may include AHF (acute heart failure), hypotension, angina pectoris, syncope (fainting), transient ischemic attack as a consequence of impaired cerebral blood supply.
Causes of autonomic dystonia syndrome
Autonomic dystonia syndrome is classified as a consequence of various pathologies of the central and peripheral nervous system. VDS is not an independent disease and rarely occurs overnight. The causes of vegetative dystonia syndrome are as follows:
- Problems at home, at school, which lead to systematic constant stress;
- Brain damage due to problems during pregnancy;
- Hormonal changes in adolescence (adolescence);
- Heredity, expressed by poor tolerance to work, high meteotropicity, and so on;
- Diseases of the endocrine system (diabetes mellitus, etc.);
- Bronchial asthma, stomach ulcer, hypertension and other somatic pathologies;
- Passive lifestyle;
- Systematic diseases of the nervous system;
- Carious teeth, sinusitis, otitis media and other permanent foci of infection;
- Mental and physical overload;
- Persistent autoimmune diseases.
Forms of the disease SSSU
- Sinus bradycardia
- rhythm with a frequency of up to 60 contractions per minute. It is considered the norm for physically trained individuals, athletes, as well as young people with a predominance of vagal influences on the heart. In addition, during sleep there is a physiological decrease in heart rate by 30%. In other cases, bradycardia accompanies various diseases.Moderate bradycardia may not impair blood circulation, but a rhythm with a frequency of less than 40 beats per minute leads to insufficient blood supply and ischemia (oxygen deficiency) of organs and tissues, thereby disrupting their function.
Regardless of the cause, the basis of bradycardia is a violation of the sinus node’s ability to generate electrical impulses with a minute frequency of more than 60 or their incorrect propagation through the conduction system.
- Sinoatrial block.
With this type of sinus dysfunction, inhibition occurs until the transmission of the electrical wave from the pacemaker to the atria completely stops. In this case, there is an increase in the pause between atrial contractions, their temporary asystole and, as a consequence, the absence of timely contraction of the ventricles, which affects hemodynamics.
The mechanism for the development of blockade can be associated both with blocking the movement of the impulse from the source and with the lack of formation of excitation in the node itself.
- SU stop.
Sinus arrest threatens sudden cardiac arrest. However, more often the role of a source of impulses is taken on by a second order pacemaker (AV node), generating signals with a frequency of 40-60 per minute or a third order (His bundle, Purkinje fibers) with AV block, frequency = 15-40 per minute.
Prevention of the syndrome
Based on the above, it is much easier to prevent a disease than to treat it.
The best prevention of the development of SSSS will be strengthening the heart muscle, as well as limiting those substances that affect the functioning of the heart:
- quitting tobacco and alcohol;
- limiting strong tea and coffee;
- a balanced diet that includes foods that have a beneficial effect on heart activity - honey, zucchini, nuts;
- regular exercise and physical activity. This includes walks in the fresh air, exercise and swimming;
- avoiding stressful situations or taking sedatives - infusion of valerian, motherwort;
- refusal to take uncontrolled medications. As mentioned above, they can affect heart rate;
- compliance with safety regulations. For example, ticks can carry Lyme disease, which also affects the sinus node. So, you need to be very careful when you are in the forests and parks in the summer.
For all its frivolity, SSSS is a very serious disease. You should not neglect your well-being and it is better to consult a doctor if the symptoms described above appear more than once or twice a year.
Symptoms of SSSU
Clinically significant dysfunction of the sinus node occurs when less than 1/10 of the working pacemaker cells remain.
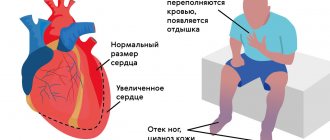
The clinical picture of SSSU is formed by 2 main groups of symptoms: cardiac
(heart) and
cerebral
(brain).
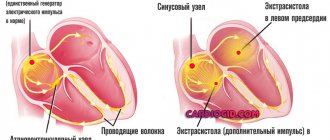
Patients complain of a feeling of a slow, irregular pulse, a sinking heart, in the case of severe bradycardia, pain in the projection of the heart, a pressing, squeezing nature behind the sternum due to a decrease in blood flow through the coronary arteries. Arrhythmia may occur (paroxysmal tachycardia, supraventricular and ventricular extrasystole, fibrillation, atrial flutter - this is felt by interruptions in the heart, palpitations, “tumbling” of the heart. In an unfavorable course, ventricular fibrillation develops, which is often the cause of sudden cardiac death.
Brain (cerebral) symptoms
in the initial stages of SSSS is presented by nonspecific symptoms: general weakness, fatigue, irritability, emotional instability, decreased memory and attention.
As sick sinus syndrome develops, drowsiness, presyncope, and short-term loss of consciousness (Morgagni-Adams-Stokes attacks) appear, associated with a sharp deterioration in blood supply to the brain. As a rule, such fainting passes on its own.
Dizziness, tinnitus, weakness also progress, the emotional sphere suffers, performance and memory are significantly reduced, and sleep is disturbed.
Naturally, with SSSS, the blood supply not only to the heart and brain deteriorates - other organs also suffer. Kidney function is impaired, the patient notices a decrease in the amount of urine; digestive function is impaired; the tone and strength of skeletal muscles decreases.
Diagnosis and treatment of sick sinus syndrome
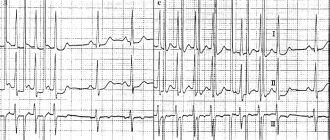
1. Persistent severe sinus bradycardia. 2. The minimum heart rate during the day, determined by daily ECG monitoring, is <40 beats/min, and its increase during physical activity does not exceed 90 beats/min. 3. Bradysystolic form of atrial fibrillation. 4. Migration of the atrial pacemaker. 5. Stopping the sinus node and replacing it with other ectopic rhythms. 6. Sinoauricular block. 7. Pauses >2.5 s, resulting from sinus node arrest, SA blockade, or rare escape rhythms. 8. Tachy-Brady syndrome, alternating periods of tachycardia and bradycardia. 9. Rarely - attacks of ventricular tachycardia and/or ventricular fibrillation. 10. Slow and unstable restoration of sinus node function after extrasystoles, paroxysms of tachycardia and fibrillation, as well as at the moment of cessation of stimulation during electrophysiological examination of the heart (post-tachycardial pause, which normally does not exceed 1.5 s, can reach 4–5 s with SSSU). 11. Inadequate reduction of rhythm when using even small doses of β-blockers. Presence of bradycardia during the administration of atropine and exercise testing. Historical background SA blockade was first described by J. Mackenzie in 1902 during an influenza epidemic. In 1909, E. Laslet observed a Morgagni–Adams–Stokes (MAC) attack in a 40-year-old woman in whom pauses in heart contractions reached 2–5 s; the atria stopped along with the ventricles, which, as the author emphasized, distinguished this phenomenon from complete atrioventricular (AV) block. D. Short (1954) drew attention to the alternation of sinus bradycardia with atrial fibrillation (AF) in some patients. He called this "bradycardia-tachycardia alternating syndrome" (Short's syndrome). The study of sinus dysfunctions was facilitated by the clinical studies of V. Lown (1967), who noted an unstable restoration of the automatism of the SA node in a number of patients who underwent the procedure of electrical defibrillation. V. Lown defined this condition as sick sinus syndrome (SSS). A year later, M. Ferrer (1968) extended this term to the group of bradyarrhythmias caused by weakening of the functions of the SA node and accompanied by corresponding clinical symptoms. Anatomy of the sinus node The sinus node (sinoauricular node, Keys-Flac node, first-order pacemaker) is a bundle of specific cardiomuscular tissue, the length of which reaches 10-20 mm and width - 3-5 mm. It is located subepicardially in the wall of the right atrium between the mouths of the vena cava. There are two types of sinus node cells - pacemaker (P-cells) and conductor (T-cells). P-cells (pacemaker) generate electrical impulses, and T-cells primarily perform a conductor function. The sinus node is the normal pacemaker of the heart - a first-order pacemaker, it generates 60-90 impulses per minute, and the heart rhythm recorded on the ECG is called sinus. The blood supply to the sinus node is carried out by the SA artery; in 60% of cases this artery arises from the right coronary artery, and in 40% from the left. The sinus node is innervated by the sympathetic and parasympathetic nervous systems. Prevalence of SSS The prevalence of sinus node dysfunction in the general population is unknown. According to the available incomplete information, in cardiac patients it is approximately 3:5000. Signs of sinus node disease are observed in 6.3–24% of patients, and therefore these patients underwent pacemaker implantation. It is believed that sinus node dysfunction is equally common in men and women. With age, the incidence of SSSS increases. Etiology of SSSS Cases of primary SSSS include dysfunction caused by organic lesions of the SA zone during: a) cardiac pathology - ischemic heart disease, hypertension, cardiomyopathy, heart defects, myocarditis, surgery and heart transplantation; b) idiopathic degenerative and infiltrative diseases; c) hypothyroidism, dystrophy of the musculoskeletal system, senile amyloidosis, sarcoidosis, scleroderma heart, malignant tumors of the heart, in the stage of tertiary syphilis, etc. Ischemia caused by stenosis of the artery supplying the sinus node and the SA zone, inflammation and infiltration, hemorrhage, dystrophy , local necrosis, interstitial fibrosis and sclerosis cause the development of functional cells of the sinoatrial node of connective tissue in place. Secondary SSSS is caused by external (exogenous) factors affecting the sinus node. Exogenous factors include hyperkalemia, hypercalcemia, treatment with drugs that reduce the automaticity of the sinus node (β-blockers, sotalol, amiodarone, verapamil, diltiazem, procainamide, cardiac glycosides, dopegit, reserpine, etc.). Particularly among external factors is autonomic dysfunction of the sinus node (ADSU). VDSU is often observed in connection with hyperactivation of the vagus nerve (reflex or long-term), causing a decrease in sinus rhythm and prolongation of refractory sinus node. The tone of the vagus nerve can increase during various physiological processes: during sleep, during urination, defecation, coughing, swallowing, nausea and vomiting, and during the Valsalva maneuver. Pathological activation of the vagus nerve can be associated with diseases of the pharynx, genitourinary and digestive tracts, which have abundant innervation, as well as with hypothermia, hyperkalemia, sepsis, and increased intracranial pressure. VDSU is more often observed in adolescents and young adults due to significant neuroticism. Persistent sinus bradycardic rhythm can also be observed in trained athletes due to the pronounced predominance of vagal tone, however, such bradycardia is not a sign of SSSS, because The increase in heart rate occurs adequately to the load. At the same time, athletes can develop true SSSS in combination with other rhythm disturbances caused by myocardial dystrophy. Classification of SSSU There is no unified classification of SSSU. Depending on the nature of the lesion, true (organic), regulatory (vagal), medicinal (toxic) and idiopathic SSS are distinguished. According to the characteristics of the clinical manifestation, the following forms of SSSS and their course variants are distinguished: 1. Latent form - absence of clinical and ECG manifestations; sinus node dysfunction is determined by electrophysiological study. There are no work restrictions; implantation of an electrical pacemaker (pacemaker) is not indicated. 2. Compensated form: there are no clinical changes, there are changes on the ECG: a) bradysystolic variant - mild clinical manifestations, complaints of dizziness and weakness. There may be a professional disability; pacemaker implantation is not indicated; b) brady/tachysystolic variant - paroxysmal tachyarrhythmias are added to the symptoms of the bradysystolic variant. Implantation of a pacemaker is indicated in cases of decompensation of the cardiovascular system under the influence of antiarrhythmic therapy. 3. Decompensated form: there are clinical and ECG manifestations of the disease. a) bradysystolic variant - persistently pronounced sinus bradycardia is determined, it is manifested by a violation of cerebral blood flow (dizziness, fainting, transient paresis), heart failure caused by bradyarrhythmia. Significant disability; indications for implantation are asystole and sinus node function recovery time (SNFRU) of more than 3 s; b) brady/tachysystolic variant (Short’s syndrome) – paroxysmal tachyarrhythmias (supraventricular tachycardia, atrial fibrillation and flutter) are added to the symptoms of the bradysystolic variant of the decompensated form. Patients are completely disabled; the indications for pacemaker implantation are the same as for the bradysystolic variant. 4. Permanent bradysystolic form of atrial fibrillation (against the background of previously diagnosed SSSU): a) tachysystolic variant - disability; there are no indications for pacemaker implantation; b) bradysystolic variant – limitation of working capacity; Indications for pacemaker implantation include cerebral symptoms and heart failure. The development of the bradysystolic form of atrial fibrillation can be preceded by any form of sinus node dysfunction (Table 1). Depending on the registration of signs of SSSS during Holter ECG monitoring, latent (signs of SSSS are not detected), intermittent (signs of SSSS are detected with a decrease in sympathetic tone and an increase in parasympathetic tone, for example, at night) and manifesting course (signs of SSSS are detected with each daily ECG) are distinguished. -monitoring). SSSU can occur acutely and chronically, with relapses. The acute course of SSSS is often observed during myocardial infarction. The recurrent course of SSSS can be stable or slowly progressive. The etiological factors distinguish between the primary and secondary forms of SSSS: the primary is caused by organic lesions of the sinus-atrial zone, the secondary – by a violation of its autonomic regulation. Clinical manifestations of SSSU The clinical manifestation of SSSU can be different. In the early stages, the course of the disease may be asymptomatic even if there are pauses of more than 4 s. As the disease progresses, patients report symptoms associated with bradycardia. The most common complaints include a feeling of dizziness and severe weakness, even fainting (MAS syndrome), chest pain caused by myocardial hypoperfusion, and shortness of breath caused by limited chronotropic reserve. In some cases, chronic heart failure develops. Fainting of a cardiac nature (MAS syndrome) is characterized by the absence of an aura and convulsions (except in cases of prolonged asystole). Patients with mild symptoms may complain of feeling tired, irritability, emotional lability and forgetfulness. Elderly patients may experience a decrease in memory and intelligence. As the disease progresses and circulatory impairment continues, cerebral symptoms become more pronounced. Possible coldness and paleness of the skin with a sharp drop in blood pressure, cold sweat. Fainting can be provoked by coughing, sudden turning of the head, or wearing a tight collar. Fainting ends on its own, but if it is prolonged, it may require resuscitation measures. The progression of bradycardia may be accompanied by symptoms of dyscirculatory encephalopathy (the appearance or intensification of dizziness, momentary memory loss, paresis, “swallowing” of words, irritability, insomnia, memory loss). The appearance of slipping rhythms can be felt as palpitations and interruptions in the functioning of the heart. Due to hypoperfusion of internal organs, oliguria, acute ulcers of the gastrointestinal tract may develop, and symptoms of intermittent claudication and muscle weakness may intensify. ECG diagnosis of sinus sinus syndrome In case of SA node dysfunction, electrocardiographic signs of sinus dysfunction can be recorded long before the onset of clinical symptoms. 1. Sinus bradycardia – slowing of sinus rhythm with heart rate less than 60 per minute. due to reduced automatism of the sinus node. In SSSS, sinus bradycardia is persistent, long-lasting, refractory to physical activity and the administration of atropine (Fig. 1). 2. Bradysystolic form of atrial fibrillation (AF, atrial fibrillation, atrial fibrillation, absolute arrhythmia, atrial fibrillation, vorhofflimmern, arrhythmia perpetua, delirium cordis, arrhythmia completa) - chaotic, fast and irregular fibrillation of individual fibers of the atrial muscle not coordinated with each other as a result of ectopic atrial impulses with a frequency of 350 to 750 per minute, causing complete disorder of ventricular contractions. In the bradysystolic form of AF, the number of ventricular contractions is less than 60 per minute. (Fig. 2). 3. Migration of the pacemaker through the atria (wandering rhythm, sliding rhythm, migrating rhythm, migration of the cardiac pacemaker, wandering pacemaker). There are several variants of the wandering (wandering) rhythm: a) wandering rhythm in the sinus node. The P wave is of sinus origin (positive in leads II, III, AVF), but its shape changes with different heart contractions. The PR interval remains relatively constant. Severe sinus arrhythmia is always present; b) wandering rhythm in the atria. The P wave is positive in leads II, III, AVF, its shape and size change with different heart contractions. Along with this, the duration of the PR interval changes; c) wandering rhythm between the sinus and AV nodes. This is the most common variant of the wandering rhythm. With it, the heart contracts under the influence of impulses that periodically change their location, gradually moving from the sinus node, along the atrial muscles to the AV junction, and again return to the sinus node. ECG criteria for migration of the pacemaker through the atria are three or more different P waves in a series of cardiac cycles, a change in the duration of the PR interval. The QRS complex does not change (Fig. 3 and 4). 4. Passive ectopic rhythms. Reduced activity of the sinus node or complete blockade of sinus impulses due to functional or organic damage to the sinus node causes the activation of automatic centers of the second order (cells of atrial pacemakers, AV junction), III order (His system) and IV order (Purkinje fibers, ventricular musculature ). Automatic centers of the second order produce unchanged ventricular complexes (supraventricular type), while centers of the third and fourth order generate dilated and deformed ventricular complexes (ventricular, idioventricular type). The following rhythm disturbances have a substitutive nature: atrial, nodal, migration of the pacemaker through the atria, ventricular (idioventricular rhythm), jumping contractions. 4.1. Atrial rhythm (slow atrial rhythm) is a very slow ectopic rhythm with foci of impulse generation in the atria (Table 2): a) right atrial ectopic rhythm - the rhythm of an ectopic focus located in the right atrium. The ECG shows a negative P' wave in leads V1–V6, II, III, aVF. The P-Q interval is of normal duration, the QRST complex is not changed; b) coronary sinus rhythm (coronary sinus rhythm) - impulses to excite the heart come from cells located in the lower part of the right atrium and the coronary sinus vein. The impulse propagates through the atria retrogradely from bottom to top. This leads to the registration of negative P' waves in leads II, III, aVF. The P'aVR wave is positive. In leads V1–V6, the P' wave is positive or biphasic. The PQ interval is shortened and is typically less than 0.12 s. The QRST complex is unchanged. The coronary sinus rhythm may differ from the right atrial ectopic rhythm only by shortening the PQ interval; c) left atrial ectopic rhythm - impulses to excite the heart come from the left atrium. In this case, a negative P' wave is recorded on the ECG in leads II, III, aVF, V3–V6. The appearance of negative P' waves in I, aVL is also possible; the P' wave in aVR is positive. A characteristic sign of left atrial rhythm is the P' wave in lead V1 with an initial rounded dome-shaped part, followed by a pointed peak - “shield and sword” (“dome and spire”, “bow and arrow”). The P' wave precedes the QRS complex with a normal PR interval of 0.12–0.2 s. Atrial rhythm frequency is 60–100 per minute, rarely below 60 (45–59) per minute. or above 100 (101–120) per minute. The rhythm is correct, the QRS complex is not changed (Fig. 5); d) lower atrial ectopic rhythm - the rhythm of an ectopic focus located in the lower parts of the right or left atrium. This leads to the registration of negative P' waves in leads II, III, aVF and a positive P' wave in aVR. The PQ interval is shortened (Fig. 6). 4.2. Nodal rhythm (AV rhythm, replacing AV nodal rhythm) is a heart rhythm under the influence of impulses from the AV junction with a frequency of 40–60 per minute. There are two main types of AV rhythm: a) junctional rhythm with simultaneous excitation of the atria and ventricles (junctional rhythm without P wave, junctional rhythm with AV dissociation without P wave): the ECG shows an unchanged or slightly deformed QRST complex, P wave absent (Fig. 7); b) junctional rhythm with different simultaneous excitation of the ventricles and then the atria (nodal rhythm with a retrograde P wave, isolated form of the AV rhythm): an unchanged QRST complex is recorded on the ECG, followed by a negative P wave (Fig. 8). 4.3. Idioventricular (ventricular) rhythm (intrinsic ventricular rhythm, ventricular automatism, intraventricular rhythm) - ventricular contraction impulses arise in the ventricles themselves. ECG criteria: widened and deformed QRS complex (more than 0.12 s), rhythm with heart rate less than 40 (20–30) per minute. The terminal idioventricular rhythm is very slow and unstable. The rhythm is often correct, but may be incorrect if there are several ectopic foci in the ventricles or one foci with varying degrees of impulse formation or exit block. If an atrial rhythm is present (sinus rhythm, atrial fibrillation/flutter, ectopic atrial rhythm), it is independent of the ventricular rhythm (AV dissociation) (Fig. 9). 5. Sinoauricular block (block of exit from the SA node, dissociatio sino-atriale, SA-block) - a violation of the formation and/or conduction of impulses from the sinus node to the atria. SA blockade occurs in 0.16–2.4% of people, mainly in people over 50–60 years of age, more often in women than in men. 5.1. Sinoauricular blockade of the 1st degree is manifested by a slowed formation of pulses in the sinus node or slowed by their atrium. The usual ECG is uninformative, diagnosed by electrical stimulation of the atrial or recording the potentials of the sinus node and on the basis of a change in the time in the synoauricular node. 5.2. Sinoauricular blockade of the II degree is manifested by the partial conduct of pulses from the sinus node, which leads to the loss of contractions of atrial and ventricles. There are two types of synoauricular blockade of the II degree: Sinoauricular blockade of the II degree of type I (with periodicals of Samoilov -Venkebach): a) progressive shortening of PP intervals (periodicals of Samoilov -Venkebach), followed by a long pause of PP; b) the highest distance PP - during a pause at the time of the loss of heart contraction; c) this distance is not equal to two normal PP intervals and less than their duration; d) the first after the pause of the PP interval is longer than the last PP interval before the pause (Fig. 10). Sinoauricular blockade of the II type II type: a) asystole - the absence of electrical activity of the heart (there are no Tooth R and QRST complex), there is a reduction in atrial and ventricles; b) the pause (asystole) is red to one normal interval RR (PP) or equal to two normal periods RR (PP) of the main rhythm (Fig. 11). The far -reaching synoaricular blockade of the II type II. By analogy with the Av -blockade, the protracted sa -blockade 4: 1, 5: 1, etc. It should be called the far -reaching sa -blockade of the II degree of type II. In some cases of a pause (isoelectric line), it is interrupted by slipping complexes (rhythms) from atrial centers of automatism or, more often, from the field of AB -connection. Sometimes delayed sinus impulses are found (coincide) with a slipping impulses. On the ECG, rare teeth P are located in the immediate vicinity of the QRS slippers. These teeth P are not drawn to the ventricles. The emerging AV -dissection can be complete and incomplete with the captures of the ventricles. One of the options for incomplete AB -dissection, when each sliding complex should be captured by the ventricles with a sinus impulse, was called Escape - Capture - Bigemini (Bigeminium "Settering - Capture"). 5.3. Sinoauricular blockade of the III degree (complete synoauricular blockade) is characterized by the lack of excitement of atrial and ventricles from the sinus node. Asystole occurs and continues until the automatic center II, III or IV order begins to operate (Fig. 12). 6. Stop sinus node (sinus node refusal, sinus arrest, sinus pause, sinus - indio) - periodic loss with a sinus node of the ability to produce pulses. This leads to the loss of the excitement and reduction of atrial and ventricles. A long pause is observed on the ECG, during which the p, QRST teeth are not recorded and isolinies are recorded. The pause when stopping the sinus node is not multiple of one interval RR (PP) (Fig. 13). 7. The atrial stop (atrial asystole, Atrial Standstill, Partial Asistol) is the lack of atrial arousal, which is observed during one or (more often) more heart cycles. Atrial asystole can be combined with ventricular asystolia, in such cases a complete asystole of the heart occurs. However, during the atrial asystole, rhythm II, III, IV drive drivers usually begin to function, which cause ventricular excitement (Fig. 14). There are three main options for stopping the atrial: a) the atrial stop along with the refusal (stop) of the SASL: there are no teeth P, as well as the electrograms of the sazla; A slow replacement rhythm from AB -connection or from Idioventricular centers is recorded. With a similar phenomenon, you can meet with severe quinidine and digitalist intoxication (Fig. 14); b) the absence of electrical and mechanical activity (stop) atrial while maintaining automatism of the sazal, which continues to control the excitement of the AV node and ventricles. Such a picture is observed with severe hyperkalemia (> 9–10 mm/l), when the correct rhythm with bruised QRS complexes without teeth R appears, this phenomenon is called the Sinnitricular Conduct; c) the preservation of the automatism of the SAS and the electrical activity of the atrial (teeth P) in the absence of their contractions. The syndrome of electromechanical dissociation (discretion) in the atria can sometimes be observed in patients with advanced atriums after their electric defibrillation. Constant stop, or paralysis, atrial is a rare occurrence. In the literature there are reports of atrial paralysis for heart amyloidosis, common atrial fibrosis, fibroelastosis, fat infiltration, vacuoral degeneration, neuromuscular dystrophy, and in the terminal period of heart diseases. 8. Bradycardia/tachycardia syndrome (tachi/brady syndrome). At the same time, the variant is alternating a rare sinus or replacement of the supraventricular rhythm with tachystole attacks (Fig. 15). The clinical assessment of the function of the sinus node of the SSCU should be considered as a probable diagnosis in patients with symptoms described above. The most complex electrophysiological studies should be carried out only if the diagnosis of sinus node dysfunction causes certain doubts. Valsalva maneuver. The simplest vagus samples with holding breathing on a deep breath (including the Valsalva test), carried out in isolation or in combination with straining, sometimes allow you to identify sinus pauses exceeding 2.5–3.0 s, which must be differentiated with pauses caused by impaired AB - Safe. The identification of such pauses indicates the increased sensitivity of the sinus node to vagus influences, which can be found both at the VDS and the SSSU. If such pauses are accompanied by clinical symptoms, an in -depth examination of the patient is required to determine the treatment tactics. Massage of the carotid sinus. The carotid sinus is a small formation of the autonomic nervous system, located at the beginning of the internal carotid artery over the branch of the general carotid artery. Carotide sinus receptors are associated with a wandering nerve. The reflex of the carotide sinus in physiological conditions causes bradycardia and hypotension due to irritation of the vagus nerve and vascular regulatory center in the medulla oblongata. With a supersensitive (hypersensitive) carotid sinus, pressing on it can cause sinus pauses exceeding 2.5–3.0 s, accompanied by a short -term disorder of consciousness. Such patients before massage of carotide zones show an assessment of the state of blood flow according to carotid and vertebral arteries, because Conducting arteries massage with pronounced atherosclerotic changes can lead to sad consequences (sharp bradycardia up to loss of consciousness and asystole!). It is important to emphasize that the syndrome of the carotide sinus can, on the one hand, develop against the background of the normal function of the sinus node, and on the other, does not exclude the presence of SSSU. Tilt -test. Tilt -test (passive orthostatic test) is considered today as a “gold standard” in the examination of patients with syncopal states of unknown etiology. Exercise testing (bicycle ergometry, thread -test). Starry testing allows you to evaluate the ability of the sinus node to increase the rhythm in accordance with the internal physiological chronotropic stimulus. Holter monitoring. Outpatient monitoring using the Holter apparatus, if it is carried out during normal daily activity, is apparently a more valuable physiological method for evaluating the function of the sinus node than stress testing. The alternating appearance of bradyarrhythms and tachyarrhythms in patients with SSU is often not found on a regular electrocardiogram at rest. Studying the function of the sinus node by the CPEC. An indicator of the automatic activity of the sinus node is the duration of the sinus pause from the moment the stimulation stops (the last artifact of the electrical stimulus) to the beginning of the first independent tooth R. This period of time is called the restoration of the function of the sinus node (VVFSU). Normally, the duration of this period does not exceed 1,500–1600 ms. In addition to the VVFSU, another indicator is calculated - the corrective time of restoration of the sinus node function (KVVFSU), which takes into account the duration of the VVFSU indicator in relation to the initial frequency of the sinus rhythm. Treatment of SSSU at the beginning of therapy for SSU cancel all drugs that can contribute to conductivity disruption. In the presence of tachi -brugida tachy tachi syndrome, it can be more flexible: with a combination of moderate sinus bradycardia, which is not yet an indication for the installation of a constant pacemaker, and frequent brady -dependent paroxysms of atrial fibrillation in some cases, an allapinin is possible in a small dose (1/2 tab. . 3-4 p./Day) followed by mandatory control during Holter monitoring. However, over time, the progression of conductivity disorders may require the abolition of drugs with the subsequent installation of the pacemaker. When the bradycardia is preserved, the simultaneous use of Belloid of 1 tab is permissible. 4 rubles/day Or theopeca 0.3 g of 1/4 tab. 2-3 p./Day. It is necessary to exclude hyperkalemia or hypothyroidism, in which the patient can be mistaken at the installation of constant ex. In case of suspicion of SSCU, you should refrain from the purpose of the suppleting sinus node of the drugs to Holter monitoring and special tests. The purpose of β -blockers, calcium antagonists (verapamil, diltiazem), sotalol, amyudarone, cardiac glycosides are inappropriate. In cases of acute development of SSCU, etiotropic treatment is carried out primarily. In case of suspicion of its inflammatory genesis, the introduction of a prednisolone of 90–120 mg iv or 20-30 mg/day is shown. inside. In acute myocardial infarction, anti -hepartic drugs (nitrates), designs (acetylsalicylic acid, clopidogrel), anticoagulants (heparin, low molecular weight heparins), cytoprotectors (trimetazidin) are prescribed. Emergency therapy of the SSSU itself is carried out depending on its severity. In cases of asystole, bouts of MAS, resuscitation measures are needed. Pronounced sinus bradycardia, worsening hemodynamics and/or provoking tachyarrhythmias, requires atropine 0.5–1.0 ml of a 0.1% solution of the p/k up to 4–6 rubles/day, infusions of dobutamine or eufillin under the control of the cardiomonitor . For a preventive purpose, a temporary endocardial stimulator can be established. Absolute indications for the implantation of the pacemaker: 1. HAC attacks (at least once). 2. Pronounced bradycardia (less than 40 in min.) And/or pauses of more than 3 s. 3. VVFSU of more than 3500 ms, KVVFSU - more than 2300 ms. 4. The presence of dizziness caused by bradycardia, presincopal conditions, coronary failure, congestive heart failure, high systolic arterial hypertension - regardless of heart rate. 5. SSSU with rhythm disorders requiring the prescription of antiarrhythmic drugs, which is impossible in impaired conductivity. Currently, it is precisely patients with SSUs that make up the vast majority of patients with permanent pacemakers. It should be noted that this method, improving the quality of life, sometimes significantly, usually does not allow to increase its duration, which is determined by the nature and severity of the concomitant organic heart disease, mainly myocardial dysfunction. When choosing a method of electrocardiastying, one should strive to ensure not only the adequate frequency of ventricular rhythm, but also preserving atrial systole.
Literature 1. Cardiac arrhythmias./Ed. W. J. Mandela. – M.: Medicine, 1996. p. 512. 2. Bokarev I.N., Popova L.V., Fomchenkova O.I. Arrhythmia syndrome. – M.: Practical Medicine, 2007. – P. 208. 3. Heart disease: A guide for doctors / Ed. R.G. Oganova, I.G. Fomina. – M.: Litterra, 2006. – P. 1328. 4. Janashia P.Kh., Shevchenko N.M., Shlyk S.V. Heart rhythm disturbances. – M.: Publishing House “Overlay”, 2006. – P. 320. 5. Isakov I.I., Kushakovsky M.S., Zhuravleva N.B. Clinical electrocardiography. – L.: Medicine, 1984. 6. Cardiology: national guide. / Ed. Yu.N. Belenkova, R.G. Oganova. – M.: GEOTAR-Media, 2010. – 1232 p. 7. Cardiology in questions and answers / Ed. Yu.R. Kovaleva. – St. Petersburg: Foliant Publishing House LLC, 2002. – P. 456. 8. Kushakovsky M.S. Cardiac arrhythmias. – St. Petersburg: Hippocrates, 1992. 9. Kushakovsky M.S., Zhuravleva N.B. Arrhythmias and heart block (atlas of electrocardiograms). – L.: Medicine, 1981. 10. Murashko V.V., Strutynsky A.V. Electrocardiography: Textbook. Manual / 3rd ed., revised. and additional / M.: Medpress LLC; Elista.: APP “Dzhangar”, 1998.– P. 313. 11. Nedostup A.V., Blagova O.V. How to treat arrhythmias. Diagnosis and therapy of rhythm and conduction disorders in clinical practice. – 3rd ed. – M.: MEDpress-inform, 2008. – P. 288. 12. Orlov V.N. Guide to electrocardiography. M.: Medical Information Agency LLC, 1999. – 528 p. 13. Tomov L., Tomov I. Heart rhythm disturbances. – Sofia: Medicine and Physical Education, 1976. 14. Zimmerman F. Clinical electrocardiography. – M.: Binom, 1997. 15. Chernov A.Z., Kechker M.I. Electrocardiographic atlas. – M.: Medicine, 1979. 16. Yakovlev V.B., Makarenko A.S., Kapitonov K.I. Diagnosis and treatment of heart rhythm disorders. – M.: Binom. Knowledge Laboratory, 2003. – P.168. 17. Yalymov A.A., Shekhyan G.G., Shchikota A.M. Guide to electrocardiography / Edited by Honored Scientist of the Russian Federation, prof. V.S. Zadionchenko – Saarbrucken, Germany. Publisher: LAP LAMBERT Academic Publishing GmbH&Co. KG, 2011. – P. 323.
Reasons for SSSU
Primary dysfunction:
- Replacement of cells with connective tissue - cardiosclerosis (post-infarction, post-myocardial, cardiomyopathic).
- Congenital underdevelopment of the sinus node.
- Senile amyloidosis.
- Idiopathic damage, including Lenegra's disease.
Secondary dysfunction:
- Increased vagal tone (vagus nerve): carotid sinus syndrome, sleep apnea, vasovagal syncope, increased intracranial pressure, myocardial infarction of the lower topic, subarachnoid hemorrhage, Bezold-Jarisch reflex, diseases of the larynx and esophagus, cardioversion.
- Effects of drugs: beta-blockers, non-dihydropyridine calcium channel blockers, cardiac glycosides, antiarrhythmics, cholinomimetics, morphine, sodium thiopental, lithium preparations.
- Inflammation of the heart muscle (myocarditis).
- Ischemia of the sinus node.
- Acute injury to the sinus due to right atrium infarction
- Traumatic damage to the cells of the sinus node and conduction system (surgery, injury).
- Electrolyte disturbances.
- Blood gas disturbances (hypoxemia, hypercapnia).
- Dysfunction of hormonal systems (most often hypothyroidism).
Diagnosis of SSSU
- An ECG
showing bradycardia of sinus origin with a frequency of up to 40 beats per minute during the day and less than 30 beats per minute at night may indicate sinus dysfunction. SA blockade, pauses of more than 3 seconds, tachy-bradycardia syndrome, migration of the pacemaker through the atria allow us to suspect a weakening of the pacemaker. - A more informative diagnostic method is Holter ECG monitoring
. It allows you to analyze the heart rhythm for a whole day or more, track the connection of disturbances with exercise, taking medications, and identify provoking factors. - In difficult situations, when dysfunction of the SU is not permanent, EFI
. An electrode is inserted into the patient's esophagus, with which the atria are stimulated to a frequency of 140-150 beats per minute, thereby suppressing the activity of the natural pacemaker and observing the time it takes to restore the function of the sinus node after cessation of stimulation.
EchoCG is used to detect organic myocardial pathology
(ultrasound of the heart), less often cardiac tomography.
Treatment of SSSU
Treatment tactics for sick sinus syndrome depend on the degree of sinus node dysfunction, the cause of the disease, clinical manifestations, and the severity of hemodynamic disorders. The secondary nature of the pathology implies treatment of the underlying disease.
For mild and moderate forms of SSSS, medications are used. If medications do not have an effect, or a complex, combined with other rhythm disturbances, or acute, severe form of sinus node dysfunction develops, disrupting regional and systemic circulation, installation of a pacemaker is indicated.
Prices
Since the pathologies are very different, their treatment methods also differ significantly from each other. Vascular surgery in Israel carries out a variety of operations by type, level of complexity, etc. which effectively help eliminate the problem and save a person’s life.
In Israel, the following operations can be performed depending on the type of disease.
For atherosclerosis of the coronary arteries and coronary heart disease, coronary angioplasty combined with stenting, as well as coronary artery bypass grafting, are performed. In case of atherosclerosis of the carotid arteries, they are stenated.
Aortic aneurysm is treated using standard prosthetics, graft stenting, aortic root reconstruction, aneurysm clipping, etc.
Endovasal surgery (obturation with special coils) helps to cure aneurysms and malformations of the cerebral arteries.
For varicose veins, effective methods are laser coagulation, foam sclerotherapy, stripping, etc.
Hemangiomas are treated by excision, sclerotherapy, cryosurgery, or laser surgery.
Prices for vascular surgery procedures in Israel are not very high, which is why treatment in clinics in this country is so popular. The cost will vary significantly depending on the treatment method, equipment and drugs used, doctor, clinic and many other factors. You can send a request to find out data for your specific case. The high level of professionalism of doctors and the use of advanced technologies guarantee a quick recovery.
The main goal is the patient’s speedy recovery and restoration of his ability to work. Treatment conditions are created in such a way that the patient feels completely comfortable - this has a good effect on the treatment process.
Approximate prices for the Department of Cardiology and Cardiac Surgery
| Disease | Approximate price, $ |
| Prices for mitral valve replacement in Israel | 49 200 — 55 720 |
| Prices for treatment of atrial fibrillation | 22 720 — 36 310 |
| Prices for treatment of hypertrophic cardiomyopathy | 39 420 |
| Prices for treatment of thoracic aortic aneurysm | 101 279 — 112 279 |
| Prices for coronary artery bypass surgery | 48 610 |
| Prices for diagnosing hypertension | 5 630 |
| Prices for treatment of abdominal aortic aneurysm | 71 960 — 74 960 |
| Prices for treatment of coronary heart disease | 9 260 — 23 110 |