The human heart works like a pump. Due to the properties of the myocardium (excitability, ability to contract, conductivity, automaticity), it is able to pump blood into the arteries, which enters it from the veins. It moves without stopping due to the fact that a pressure difference is formed at the ends of the vascular system (arterial and venous) (0 mmHg in the main veins and 140 mmHg in the aorta).
The work of the heart consists of cardiac cycles - continuously alternating periods of contraction and relaxation, which are called systole and diastole, respectively.
Phase structure
The cycle begins with atrial systole, which lasts 0.1 seconds. Their diastole lasts 0.7 seconds. Ventricular contraction lasts 0.3 seconds, their relaxation lasts 0.5 seconds. The general relaxation of the chambers of the heart is called a general pause, and in this case it takes 0.4 seconds. Thus, there are three phases of the cardiac cycle:
- atrial systole – 0.1 sec.;
- ventricular systole – 0.3 sec.;
- cardiac diastole (general pause) – 0.4 sec.
The general pause preceding the start of a new cycle is very important for filling the heart with blood.
Before the onset of systole, the myocardium is in a relaxed state, and the chambers of the heart are filled with blood that comes from the veins.
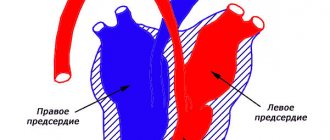
The pressure in all chambers is approximately the same, since the atrioventricular valves are open. Excitation occurs in the sinoatrial node, which leads to contraction of the atria; due to the pressure difference at the time of systole, the volume of the ventricles increases by 15%. When atrial systole ends, the pressure in them decreases.
Atrial systole (contraction)
Before the onset of systole, blood moves to the atria and they are successively filled with it. Part of it remains in these chambers, the rest is sent to the ventricles and enters them through the atrioventricular openings, which are not closed by valves.
At this moment, atrial systole begins. The walls of the chambers tense, their tone increases, the pressure in them increases by 5-8 mm Hg. pillar The lumen of the veins that carry blood is blocked by annular bundles of myocardium. The walls of the ventricles at this time are relaxed, their cavities are expanded, and blood from the atria quickly rushes there through the atrioventricular openings without difficulty. The duration of the phase is 0.1 seconds. Systole overlaps the end of the ventricular diastole phase. The muscle layer of the atria is quite thin, since they do not require much force to fill the neighboring chambers with blood.
Ventricular systole (contraction)
This is the next, second phase of the cardiac cycle and it begins with tension of the heart muscles. The voltage phase lasts 0.08 seconds and in turn is divided into two more phases:
- Asynchronous voltage – duration 0.05 sec. Excitation of the walls of the ventricles begins, their tone increases.
- Isometric contraction – duration 0.03 sec. The pressure in the chambers increases and reaches significant values.
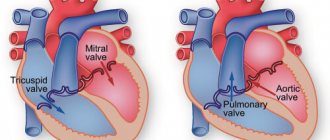
The free leaflets of the atrioventricular valves floating in the ventricles begin to be pushed into the atria, but they cannot get there due to the tension of the papillary muscles, which stretch the tendon threads that hold the valves and prevent them from entering the atria. At the moment when the valves close and communication between the heart chambers stops, the tension phase ends.
As soon as the voltage reaches its maximum, a period of ventricular contraction begins, lasting 0.25 seconds. The systole of these chambers occurs precisely at this time. About 0.13 sec. The rapid expulsion phase lasts - the release of blood into the lumen of the aorta and pulmonary trunk, during which the valves adhere to the walls. This is possible due to an increase in pressure (up to 200 mmHg in the left and up to 60 in the right). The rest of the time falls on the slow ejection phase: blood is ejected under less pressure and at a lower speed, the atria are relaxed, and blood begins to flow into them from the veins. Ventricular systole is superimposed on atrial diastole.
General pause time
Ventricular diastole begins, and their walls begin to relax. This lasts for 0.45 seconds. The period of relaxation of these chambers is superimposed on the still ongoing atrial diastole, therefore these phases are combined and called a general pause. What happens during this time? The ventricle contracted, expelled blood from its cavity and relaxed. A rarefied space with pressure close to zero formed in it. The blood strives to get back, but the semilunar valves of the pulmonary artery and aorta, closing, prevent it from doing this. Then it is sent through the vessels. The phase that begins with relaxation of the ventricles and ends with the closure of the lumen of the vessels by the semilunar valves is called protodiastolic and lasts 0.04 seconds.
After this, an isometric relaxation phase begins, lasting 0.08 seconds. The cusps of the tricuspid and mitral valves are closed and do not allow blood to flow into the ventricles. But when the pressure in them becomes lower than in the atria, the atrioventricular valves open. During this time, blood fills the atria and now freely flows into other chambers. This is a fast filling phase lasting 0.08 seconds. Within 0.17 sec. the slow filling phase continues, during which blood continues to flow into the atria, and a small part of it flows through the atrioventricular openings into the ventricles. During the diastole of the latter, blood enters them from the atria during their systole. This is the presystolic phase of diastole, which lasts 0.1 seconds. Thus the cycle ends and begins again.
Theory
Tests
Help the site
Disable advertising
Cardiac muscle, like skeletal muscle, has the following physiological properties:
- excitability,
- contractility,
- conductivity.
However, the myocardium, unlike skeletal muscles, has another special property - automaticity .
Automaticity is the ability of the heart to rhythmically excite and contract without any external influences, that is, under the influence of impulses arising within itself .
Spontaneous excitation occurs in the heart in the nodes and bundles of the conduction system .
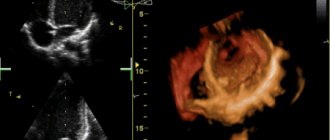
Heart sounds
The heart makes characteristic sounds similar to a knock. Each beat consists of two main tones. The first is the result of contraction of the ventricles, or, more precisely, the slamming of valves, which, when the myocardium is tense, close the atrioventricular openings so that blood cannot return to the atria. A characteristic sound is produced when their free edges close. In addition to the valves, the myocardium, the walls of the pulmonary trunk and aorta, and tendon threads take part in creating the shock.
The second sound is formed during ventricular diastole. This is the result of the semilunar valves, which prevent blood from flowing back, blocking its path. A knock is heard when they connect in the lumen of the vessels with their edges.
In addition to the main tones, there are two more - the third and fourth. The first two can be heard using a phonendoscope, while the other two can only be recorded by a special device.
Heartbeats have important diagnostic value. Based on their changes, it is determined that disturbances have occurred in the functioning of the heart. In case of illness, the beats can bifurcate, be quieter or louder, and be accompanied by additional tones and other sounds (squeaks, clicks, noises).
Conduction system of the heart
The conduction system of the heart includes the following sections:
1. Sinoatrial (sinoatrial node):
- located under the right ear at the junction of the superior vena cava into the right atrium,
- located under the epicardium
- area 20*2 mm^2,
- consists of 40 thousand cells,
- richly supplied with capillaries and nerves.
2. Interatrial and internodal pathways - transmit excitation through the atria.
There are 3 of them:
- anterior (Bachmann's bundle),
- medium (Wennebach),
- rear (Torela).
3. Atrioventricular node (atrioventricular):
- located in the lower part of the interatrial septum,
- under the endocardium of the right atrium,
- innervated by fibers of the vagus and sympathetic nerves.
4. The bundle of His arises from the atrioventricular node:
- length 8-10 mm,
- goes along the interventricular septum,
- at its apex it bifurcates into right and left legs.
5. Purkinje fibers:
- a network of atypical fibers in the walls of both ventricles,
- from them excitation is transmitted to the contractile myocardium of the ventricles.
Conducting system of the heart:
- atypical cardiomyocytes,
- cells are rich in sarcoplasm,
- the transverse striations in them are less clearly expressed,
- few myofibrils,
- retains signs of embryonic myocardium,
- resistant to hypoxia,
- energy is generated due to the activation of anaerobic glycolysis processes.
During diastole in the cells of the sinoatrial node (1st order pacemaker - pacemaker):
- the membrane potential decreases , that is, slow diastolic depolarization (SDD) ;
- membrane potential (MP) reaches CUD , that is, the MP changes from 50-60 mV to 30-40 mV spontaneously - action potential (AP) or pacemaker potential , which propagates through the conduction system of the heart, passes to the myocardium.
Features of pacemaker cells:
- low level of membrane potential (-50 - -60 mV),
- ability to DMD (decrease in MP to CUD spontaneously),
- low AP amplitude (-30 - -50 mV) without reversal (mostly).
Causes of DMD ( related to the special properties of the pacemaker membrane ):
- a gradual spontaneous increase in diastole of membrane permeability for Na and Ca entering the cell;
- decreased permeability of K leaving the cell;
- decreased activity of the Na-K pump (Na-K-ATPase).
The frequency of excitations in the cells of the sinoatrial node is 60-80 per 1 minute. first order pacemaker .
All underlying conduction systems of the heart (atrioventricular node, His bundle, Purkinje fibers, atypical atrial fibers) have the ability to automate They are normally only potential or latent pacemakers.
The atrioventricular node has an automatic capacity of 40-50 impulses/min . second order pacemaker .
His bundle cells - 30-40 imp/min .
Purkinje fibers - about 20 imp/min .
W. Gaskell introduced the concept of an automaticity gradient:
The further the center of automation is located from the venous end of the heart and the closer to the arterial end, the less ability it has for automaticity.
The true pacemaker is the cells of the sinoatrial node.
Features of the structure of smooth muscles
The muscles of this group are found in almost all important internal organs, such as the intestines, stomach, uterus, and they are also present in the walls of blood vessels, skin and eyes. Smooth muscles perform involuntary movements, obeying only automatic signals from the nervous system.
Muscle cells have a spindle-shaped shape; they shorten due to the sliding of their filaments. The speed of this process is much slower than that of skeletal muscles, due to which they are able to remain in a tense state for a long time without expending a lot of energy.
An important feature of smooth muscles is their ability to maintain their shape, changed by stretching or deformation, as well as high plasticity, which is important for the functioning of internal organs. The muscles of this group are characterized by the slowest contraction and relaxation, which can last up to several tens of seconds. They can also remain in a state of tone for a long time, practically without getting tired. The main functions of smooth muscles: •
- maintaining pressure in hollow internal organs (ureter, intestines, uterus);
- contracting, they ensure natural peristalsis of organs and their emptying;
- regulate pressure in blood vessels;
- in the organs of vision they provide dilation and constriction of the pupil;
- located on the skin, they promote the secretion of subcutaneous fat.
Prolonged stretching of smooth muscles leads to their tension, which, in turn, plays an important role in promoting the contents of the gastrointestinal tract and ureters. The smooth muscles of the walls of blood vessels, contracting, affect the body's blood supply and blood pressure.