Hyperinsulinism - main symptoms:
- Mood swings
- Convulsions
- Weakness
- Cardiopalmus
- Irritability
- Constant feeling of hunger
- Loss of consciousness
- Memory impairment
- Increased sweating
- Numbness of the limbs
- Malaise
- Anxiety
- Visual impairment
- Feeling of fear
- Deterioration of mental abilities
- Hand twitching
- Leg twitching
- Tingling in the limbs
- Loss of orientation in space
- Coma
What is hyperinsulinism
Hyperinsulinism is a disease associated with increased insulin levels and decreased blood sugar in a person. Characteristic signs of the disease: general weakness, dizziness, increased appetite, tremor and psychomotor agitation. The congenital form is very rare, affecting approximately one newborn out of 50 thousand.
The acquired type of the disease is most often determined in females aged 35–50 years.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
- Possible complications
- Prevention
Hyperinsulinism is diagnosed in the process of interviewing the patient, when the clinical symptoms of the disease are revealed, after which functional tests are carried out, blood glucose saturation is examined over time, ultrasound or tomography of the pancreas and brain is performed.
Pancreatic formations can only be treated surgically. For extrapancreatic pathology, therapy is aimed at eliminating the underlying disease and its symptomatic manifestations. The patient is prescribed a special diet.
If timely treatment is not given, the patient may fall into a hypoglycemic coma.
Introduction
The syndrome of organic hyperinsulinism (OH) is caused by an absolute excess of insulin and associated hypoglycemia. Occurrence of O.G. is no more than 4 cases per 1 million population per year [2, 16-18]. Despite this, the social significance of the disease is high, which is due to the predominant impact on people of working age and its severe disabling course. The causes of OH syndrome are insulin-producing neuroendocrine tumor - insulinoma (sporadic or as part of the syndrome of multiple neuroendocrine neoplasia type I - MEN-I), rarely - nesidioblastosis (diffuse hypersecretion of insulin by islet cells of the pancreas). Due to the small size of insulinomas, determination of their exact location in the pancreas (PG) at the preoperative stage, even in specialized clinics, rarely exceeds 85%. This circumstance sometimes serves as the reason for “blind” resections of the pancreas during OH, in which the tumor may not be removed [11-13, 20].
Reduced funding for domestic healthcare and the associated need to save material resources require a reasonable and expedient approach when choosing diagnostic methods without harm to the patient.
The purpose of the work is to optimize the diagnosis and tactics of surgical treatment of insulin and nesidioblastosis.
Causes of hyperinsulinism
Congenital hyperinsulinism is uncommon in children. The causes of the anomaly are:
- various pathologies in the process of fetal formation;
- genetic mutations;
- asphyxia at birth.
The acquired form of the disease has two types:
- Pancreatic. Leads to absolute hypoglycemia.
- Non-pancreatic. Causes a slight increase in insulin.
The first type occurs due to the growth of a benign or malignant tumor.
The formation of the non-pancreatic form is influenced by the following factors:
- eating disorders, prolonged fasting, large loss of fluid due to diarrhea, vomiting or during breastfeeding;
- pathological disorders in the functioning of the liver (cancer, cirrhosis, hepatosis) lead to problems with metabolism in the body;
- improper use of drugs that replace blood sugar in diabetes;
- diseases of the endocrine system;
- lack of enzymes that affect glucose metabolism.
The diagnosis of hyperinsulinism is related to sugar levels. Glucose is the main nutrient of the central nervous system and is required by the brain to function normally. If insulin levels in the blood rise and glycogen accumulates in the liver, inhibiting the process of glycogenolysis, this leads to a decrease in glucose levels.
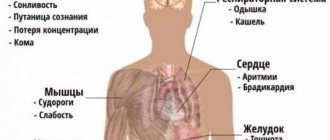
A decrease in blood sugar concentration inhibits metabolic processes, reducing the energy supply to brain cells. Redox processes are disrupted and the supply of oxygen to cells is reduced, causing fatigue, drowsiness, slowing down reactions and leading to apathy. As symptoms worsen, the disease can provoke a heart attack, seizures, respiratory and heart failure.
How the body produces insulin
Why is insulin resistance dangerous?
Even in people without serious changes in metabolism, insulin resistance triggers the processes of early aging; it is also known today that it is precisely it that is associated with severe cardiovascular pathologies and their dangerous complications (stroke, heart attack, acute cerebrovascular accidents, diabetic neuropathy, etc.).
Insulin resistance is very common. In 10-15% of adults (without chronic diseases and diagnoses) it can be detected by chance, during any examinations. This means that thousands of people not only do not know about it, but are also at risk of dangerous diseases!
It may seem that insulin resistance is a very insidious and hidden enemy of health, but in fact this disguise is very arbitrary, because a deviation can be suspected in the presence of specific problems in appearance and well-being.
For example, all women, especially middle-aged women, are familiar with the problem of being overweight. There comes a time when extra pounds literally become fused with the body, it is almost impossible to lose them, no diets help. Moreover, it feels like the excess weight is concentrated in the abdominal area - which is why many women dream of losing weight specifically at the waist, pumping up their abs, without attaching importance to other parts of the body. Meanwhile, age
and
the accumulation of adipose tissue in the abdominal area
(the so-called abdominal obesity, of the central type) are two of the most important factors that trigger the development of insulin resistance and support its strengthening.
Women over 35 years of age may experience various hormonal abnormalities.
, which at this age do not yet lead to the development of diseases, but create a “storm” in the body. Fluctuations in the content of estrogen and testosterone (and long before the onset of menopause), a decrease in the concentration of thyroid hormones and an increased release of stress hormones - adrenaline, cortisol - all this primarily affects physical health. Problems that are related to each other are gradually accumulating: excess weight, increased cholesterol levels in the blood, high blood pressure. Insulin resistance can be either a consequence of these changes in the body or their faithful companion.
Bad habits, lack of physical activity, and a diet based on fast food contribute to the development of insulin resistance.
and generally
poor quality of food
. By the way, strict diets and other food restrictions can also be attributed to poor quality of nutrition: the body does not get better from them, and the constant “swing” of losing and gaining weight only increases the tendency to insulin resistance.
If you think about it, in the lives of each of us there are at least a couple of the listed harmful factors, so if some problem has been bothering you for a long time and seriously (can’t lose weight, constantly high blood pressure, headaches and weakness), you should consult a doctor and describe him a complete picture of his symptoms. It’s not uncommon to dot all the points
i is assisted by an endocrinologist and carrying out several tests (glucose, glucose tolerance test, glycated hemoglobin, insulin resistance index, etc.).
Classification
Congenital hyperinsulinism, from the point of view of the course of the disease, can be divided into the following types:
- Transitional form. Occurs in children born to mothers with uncompensated gestational diabetes mellitus.
- Persistent form. This variety is diagnosed in newborns. The appearance of the pathology is associated with a congenital disorder of cells regulating insulin and its uncontrolled release.
Morphologically, the persistent form of the disease can be divided into the following types:
- Diffuse type. It has four varieties, which are evenly distributed according to autosomal recessive and autosomal dominant modes of inheritance.
- Focal type. Characteristic is clonal degeneration and hyperplasia of only part of the insular apparatus. A somatic mutation is detected.
- Atypical type. It manifests itself with signs uncharacteristic for this disease.
The most commonly used classification is based on the causes of the disease:
- Primary hyperinsulinism - pancreatic, organic or absolute hyperinsulinism. Consequence of the tumor process. In 90% of cases, insulin rises due to tumors of a benign nature and very rarely - with a malignant variety (carcinoma). The organic variety of the disease is very difficult.
- Secondary hyperinsulinism is functional hyperinsulinism (relative or extrapancreatic). Its appearance is associated with a deficiency of contrainsular hormones and pathological processes in the nervous system and liver. Attacks of hypoglycemia occur due to fasting, overdose of drugs with sweeteners, stress and excessive exercise.
Determination of the type and form of the disease is carried out during diagnostic measures.
Insulinoma (clinic, diagnosis and treatment)
Authors: R.A.MANUSHAROVA,
Doctor of Medical Sciences, Professor,
D.I. CHERKEZOV,
Candidate of Medical Sciences, Clinic of Gynecology and Andrology, RMAPO, Moscow
Insulinoma is a tumor of the β-cells of the islets of Langerhans that produces excessive amounts of insulin, resulting in attacks of hypoglycemic symptoms. The symptom complex of hyperinsulinism was first described simultaneously and independently by Harris and V.A. Oppel in 1924.
In 1927, Wilder et al., studying tumor extracts from a patient with insulinoma, discovered an increased insulin content in them. Floyd et al. (1964), studying the reaction of the same patients to tolbutamide, glucagon and glucose, noted that they had high levels of insulin in the blood. In 1929, the first successful operation (Graham) was performed to remove an insulin-producing pancreatic tumor. Thus, it took years of persistent research to describe the clinical picture of the disease, methods of its diagnosis and treatment. In the literature, this disease is called differently: insulinoma, hypoglycemic disease, organic hypoglycemia, relative hypoglycemia, hyperinsulinism, insulin-secreting insulinoma, but the term “insulinoma” is currently generally accepted. This neoplasm occurs mainly in patients aged 26-55 years. Children suffer from insulinoma extremely rarely.
Insulinoma occurs mainly in patients aged 26-55 years.
The pathophysiological basis of the clinical manifestations of tumors from β-cells of the islets of Langerhans is determined by the hormonal activity of these neoplasms. By not obeying the physiological mechanisms that regulate glucose homeostasis, B-cell adenomas lead to the development of chronic hypoglycemia. Due to the fact that the symptomatology of insulinoma occurs as a result of hyperinsulinemia and hypoglycemia, the severity of the clinical manifestations of the disease in each individual case indicates the patient’s individual sensitivity to insulin and lack of blood sugar. The results of our observations indicate that patients tolerate blood glucose deficiency differently. The extreme polymorphism of symptoms and the predominance of one or another of them in the general symptom complex of the disease in individual patients are also understandable. Blood glucose is necessary for the functioning of all organs and tissues of the body, especially the brain. Brain function uses approximately 20% of all glucose entering the body. Unlike other organs and tissues of the body, the brain does not have glucose reserves and does not use free fatty acids as an energy source. Due to the cessation of glucose entering the cerebral cortex for 5-7 minutes, irreversible changes occur in its cells and the most differentiated elements of the cortex die.
Unlike other organs and tissues of the body, the brain does not have glucose reserves and does not use free fatty acids as an energy source.
Gittler
et al. identified 2 groups of symptoms that develop during hypoglycemia. Group I includes fainting, weakness, trembling, palpitations, hunger, and increased excitability. The author associates the development of these symptoms with reactive hyperadrenalineemia. Disorders such as headache, blurred vision, confusion, transient paralysis, ataxia, loss of consciousness, coma are combined into group II. With gradually developing symptoms of hypoglycemia, changes associated with the central nervous system (CNS) prevail, and with acute hypoglycemia, symptoms of reactive hyperadrenalineemia prevail. As a result of the disruption of contrainsular mechanisms and the adaptive properties of the central nervous system, acute hypoglycemia develops in patients with insulinomas.
Most authors, when considering the clinical picture and symptomatology of insulinoma, focus on the manifestations of hypoglycemia attacks, but the study of the symptoms observed in the interictal period is no less important, because they reflect the damaging effects of chronic hypoglycemia on the central nervous system. The most characteristic signs of insulinoma are obesity and increased appetite. O.V. Nikolaev (1962) divides all the symptoms observed with insulin-producing pancreatic tumors into manifestations of the latent period and into signs of a period of severe hypoglycemia. This concept reflects the phases of relative well-being observed in patients, which are periodically replaced by clinically significant manifestations of hypoglycemia.
The most characteristic signs of insulinoma are obesity and increased appetite.
In 1941, Whipple described a triad of symptoms that most fully unite the various aspects of the clinical manifestations of insulinoma, as well as the results of a study of blood sugar levels at the time of an attack of hypoglycemia:
1. The occurrence of attacks of spontaneous hypoglycemia on an empty stomach or 2-3 hours after eating. 2. A drop in blood sugar levels below 50 mg% during an attack. 3. Stopping an attack with intravenous glucose or sugar intake.
In the latent phase of hyperinsulinism, as well as in insulinoma, neuropsychiatric disorders play a leading role. Neurological symptoms in this disease include insufficiency of the VII and XII pairs of cranial nerves of the central type, asymmetry of tendon and periosteal nerves, unevenness or decreased abdominal reflexes. Sometimes pathological reflexes of Babinsky, Rossolimo, Marineske - Radovich are observed, and less often - others. Patients may experience symptoms of pyramidal insufficiency without pathological reflexes, as well as sensory disturbances, which consist in the appearance of zones of cutaneous hyperalgesia, S3, D4, D12, L2-5. Zakharyin-Ged zones, characteristic of the pancreas (D7-9), are observed extremely rarely. Brainstem disorders in the form of horizontal nystagmus and upward gaze paresis are observed in approximately 15% of patients. Neurological analysis shows that the left hemisphere of the brain is more sensitive to hypoglycemic conditions, which explains the higher frequency of its lesions compared to the right. In severe cases of the disease, symptoms of combined involvement of both hemispheres in the pathological process are observed. Some men developed erectile dysfunction in parallel with the worsening of the disease. According to our data, neurological disorders in the interictal period in patients with insulinoma were characterized by polymorphism and the absence of any symptoms characteristic of this disease. The extent of these lesions reflects the individual sensitivity of the body's nerve cells to blood glucose levels and indicates the severity of the disease. Disruption of higher nervous activity in the interictal period led to a decrease in memory and mental capacity, indifference to the environment, loss of professional skills, which often forced patients to engage in less skilled work, and sometimes led to disability. In severe cases, patients did not remember past events, and sometimes could not even name their last name and year of birth. The decisive factor in the development of mental disorders is not the duration, but the severity of the disease, which depends on the patient’s individual sensitivity to a lack of blood glucose and the severity of compensatory mechanisms.
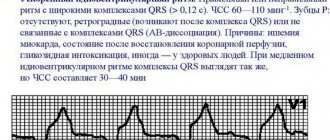
Electroencephalograms of patients recorded outside of an attack of hypoglycemia (on an empty stomach or after breakfast) revealed high-voltage discharges of O-waves, local sharp waves and discharges of sharp waves, and during an attack of hypoglycemia, in addition to the described EEG changes, high-voltage slow activity appeared, which in most patients at the height of the attack occupied the entire length of the recording. One of the constant symptoms characteristic of insulinoma is considered to be a feeling of hunger. Thus, the majority of our patients had increased appetite with a pronounced feeling of hunger before the attack. 50% of them were overweight (from 10 to 80%) due to frequent meals (mainly carbohydrates). It should be emphasized that some patients ate up to 1 kg or more of sugar or sweets per day. However, some patients, on the contrary, experienced an aversion to food, required constant care and even intravenous infusion of glucose and protein hydrolysates due to extreme exhaustion.
Thus, neither increased appetite nor hunger can be considered characteristic of this disease, although these symptoms may occur in isolated cases. Instructing the patient to carry sweets with him is more valuable from a diagnostic point of view. Most of our patients always had sweets, baked goods, and sugar with them. Some patients developed an aversion to this kind of food after a certain time, but they could not refuse to take it.
Poor nutrition gradually led to weight gain and even obesity. However, excess body weight was not observed in all patients; in some of them it was normal or even below normal. Weight loss was more often observed in patients whose appetite was reduced, as well as in patients experiencing an aversion to food.
Some patients experienced muscle pain, which many authors associate with the development of various degenerative processes in muscle tissue and its replacement with connective tissue. Low awareness of doctors about this disease often leads to diagnostic errors, as a result of which patients with insulinoma are treated for a long time and unsuccessfully for other diseases.
Diagnosis of insulinoma
When examining patients with insulinoma, the time of occurrence of the attack and its connection with food intake are determined from the anamnesis. The development of a hypoglycemic attack in the morning, as well as when skipping another meal, during physical and mental stress, in women on the eve of menstruation, indicates insulinoma. Physical research methods do not play a significant role in the diagnosis of insulinoma due to the small size of the tumor.
Functional diagnostic tests play an important role in the diagnosis of insulinoma.
A study of fasting blood sugar levels before treatment revealed a decrease below 60 mg% in the vast majority of patients. However, it should be noted that in the same patient, the blood sugar level varied on different days and could be normal. When determining the level of insulin in blood serum on an empty stomach, an increase in its content was noted in the vast majority of patients; however, in some cases, during repeated studies, normal values were observed. Such fluctuations in fasting blood sugar and insulin levels can be associated with the unequal hormonal activity of insulinoma on different days, as well as with the heterogeneous expression of contrainsular mechanisms.
Conducting a daily glycemic profile against the background of a normal diet in 52 patients allowed us to identify 3 groups of patients. Group I included patients whose blood sugar levels remained fairly consistently below normal levels throughout the day (below 60 mg%). In this group, clinically significant hypoglycemic conditions developed more often. Group II included patients with alternating normal and low blood sugar levels, Group III included patients with normal blood sugar levels throughout the day. In patients of the last 2 groups, an attack of hypoglycemia developed much less frequently than in group I.
Thus, in some cases, the results of studying blood sugar levels during the day make it possible to judge the nature of the clinical course of the disease.
The fasting test is the most informative when diagnosing insulinoma. During a fasting test, in 48 of 52 patients a hypoglycemic attack developed within 7-24 hours after the start of fasting, and in only 4 patients - after 40-50 hours. Blood sugar decreased to an average of 21 mg%. Thus, an attack of hypoglycemia developed in all patients during the fasting test, although at different times. In 20 out of 52 patients, the insulin activity of the blood serum was determined simultaneously with the study of blood sugar levels. The level of total insulin activity during an attack of hypoglycemia in 7 patients increased 2-2.5 times, and in 10 it changed slightly compared to the initial level, and in 3 it decreased. The level of free insulin activity during an attack of hypoglycemia increased in 18 of 20 patients (on average 1.5-3 times), in one patient it did not change, and in one it decreased. The level of radioimmune insulin during a fasting test was studied during an attack of hypoglycemia in 9 patients; however, in 3 of them it increased 1.5-2 times, and in 6 patients it did not change.
When performing a fasting test, the majority of patients experienced an increase in the biological activity of insulin. The reason for this is unclear. Perhaps it was this change that led to the occurrence of a hypoglycemic attack in these patients. At the same time, an attack of hypoglycemia during a fasting test was not always accompanied by a high level of insulin and could occur against the background of the same level of insulin as at the beginning of the test. It should be noted that in healthy people, during prolonged fasting, there is a sharp decrease in insulin levels, reaching undetectable values due to a decrease in its formation in b-cells, as a result of the cessation of glucose supply to the latter. Thus, it can be assumed that in this group of patients, the insulin level at the time of a hypoglycemic attack can be regarded as elevated if we consider it in relation to the blood sugar level that was observed at the time of the attack.
In 15 patients with insulinomas, a test with tolbutamide was carried out with a simultaneous study of blood sugar and insulin levels. Administration of tolbutamide to healthy individuals caused a marked decrease in blood sugar at 15-30 minutes by approximately 40% compared to the initial level, with a simultaneous increase in insulin activity (total and free) by 1.7-2.5 times. 120 minutes after administration of the drug, insulin and blood sugar levels in healthy individuals returned to baseline and they did not develop an attack of hypoglycemia. Of the 15 patients with insulinomas, the test with tolbutamide was positive in 10 patients, although in all 15 patients an insulinoma was discovered and removed during surgery. In 8 patients, a hypoglycemic attack developed 30-120 minutes after the administration of tolbutamide, while the blood sugar level decreased to 21-42 mg%. The insulin level at the time of the attack increased 1.5-8 times, i.e. could increase as much as in healthy people, but the absolute values of insulin levels during an attack were significantly higher than in healthy people. In 2 patients, a hypoglycemic attack did not develop, but their blood sugar levels after administration of tolbutamide decreased by 40% from the initial level and remained low until the end of the study (within 3 hours). In these 2 patients, the test was regarded as positive. After patients were brought out of a hypoglycemic attack by intravenous administration of a 40% glucose solution, insulin levels decreased, approaching initial values. A test with leucine was carried out in 12 patients with insulinomas. In healthy people, after taking leucine, the level of blood sugar and insulin changed slightly, and in patients with insulinomas, at 30-60 minutes after administration of the drug, there was a pronounced decrease in blood sugar levels (by 40-80%) compared to the initial level and an increase in insulin levels on average 1.5-3 times. At this point, the patients developed a hypoglycemic attack. After the patient was brought out of an attack of hypoglycemia by intravenous administration of a 40% glucose solution, the blood sugar level increased, and serum insulin decreased. In 10 out of 12 patients, an insulinoma was discovered and removed during surgery, one patient had not yet been operated on at the time of the study, and in one patient the tumor was not detected during surgery (perhaps in the latter case there was an atypical location of the tumor of a very small size, if we assume taking into account that all his other tests were positive). Thus, the leucine test is a valuable diagnostic tool for the rapid detection of β-cell tumors of the islets of Langerhans.
In 55 patients, a glycemic curve was performed with an oral load of 50 g of glucose. A flattened type of glycemic curve without a pronounced rise in blood sugar levels at 30 and 60 minutes was found in the vast majority of patients (44 out of 55). In 11 patients, the glycemic curve was the same as in healthy people. The flat type of curves in insulinomas can be explained by the presence of high levels of insulin in the blood serum, which apparently prevents the increase in blood sugar concentrations during carbohydrate loading. In all patients, the level of insulin activity (total and free) was high on an empty stomach and remained at this level until the end of the study, sometimes increasing by the end of the 2nd or 3rd hour. This response of the insular apparatus of the pancreas to the administration of glucose in patients with insulinomas, which differs from the reaction of healthy individuals, can be explained by the altered sensitivity of tumor cells to the physiological stimulant, which is glucose. However, in some patients, towards the end of the carbohydrate load, a hypoglycemic attack developed, accompanied by an increase in insulin levels.
A comparison of fasting blood sugar and insulin levels during tests with fasting, leucine and tolbutamide showed that the vast majority of patients during the period of severe hypoglycemia, i.e. During the attack, the highest insulin levels were observed. At the same time, some patients had a high level of insulin activity on an empty stomach with normal blood sugar concentrations. This discrepancy between insulin and fasting blood sugar levels may be due to excessive activity of the contrainsular mechanisms in response to increased insulin secretion, as well as the fact that the majority of insulin in the fasting blood may be less active forms.
Thus, we can conclude that the most informative and accessible diagnostic test for insulinomas is a fasting test, which in all patients was accompanied by the development of an attack of hypoglycemia with a sharp decrease in blood sugar levels, although the insulin level with this test often remains unchanged compared with its level before the attack. A test with leucine and tolbutamide in patients with insulinomas leads to a marked increase in serum insulin levels and a significant decrease in blood sugar levels with the development of an attack of hypoglycemia. However, these tests do not give positive results in all patients. Glucose load is less indicative in diagnostic terms, although it has a certain significance when compared with other functional tests and the clinical picture of the disease.
Recently, great diagnostic importance has been attached to the C-peptide suppression test. Within 1 hour, the patient is administered insulin intravenously at the rate of 0.1 U/kg. The presence of insulinoma can be assumed when C-peptide decreases by less than 50%.
The vast majority of insulin-producing pancreatic tumors do not exceed 0.5-2 cm in diameter, which makes it difficult to detect them during surgery. Thus, in 20% of patients, the tumor cannot be detected during the first, and sometimes during the second and third operations.
Malignant insulinomas occur in 10-15% of cases, and a third of them metastasize. For the purpose of topical diagnosis of insulinomas, mainly three methods are used: angiographic, catheterization of the portal system and computed tomography of the pancreas (Antonov A.V., 1991). Angiographic diagnosis of insulinomas is based on the hypervascularization of these neoplasms and their metastases. The arterial phase of the tumor is represented by the presence of a hypertrophied artery feeding the tumor and a thin network of vessels in the area of the lesion. The capillary phase is characterized by local accumulation of contrast agent in the area of the tumor. The venous phase is manifested by the presence of a vein draining the tumor. Most often, signs of the capillary phase are found. The angiographic research method makes it possible to diagnose a tumor in 60-90% of cases. However, the greatest difficulties arise when the tumor is small, up to 1 cm in diameter, and when it is localized in the head of the pancreas. The difficulties of localizing insulinomas and their small size make them difficult to detect using computed tomography. Such tumors, located in the thickness of the pancreas, do not change its configuration, and in terms of X-ray absorption coefficient they do not differ from normal pancreatic tissue, which makes their determination difficult. The reliability of the method is 50-60%. In some cases, they resort to catheterization of the portal system in order to determine the level of IRI in the veins of various parts of the pancreas. The localization of a functioning neoplasm can be judged by the maximum IRI value. Due to technical difficulties, this method is usually used when the results of the previous two studies are negative.
Sonography in the diagnosis of insulinoma is not widespread due to excess body weight in the vast majority of patients, because the fat layer is a significant obstacle to the ultrasonic wave.
In 80-95% of patients with insulinomas, topical diagnostics using modern research methods makes it possible to establish the localization, size, extent and malignancy (metastases) of the tumor process before surgery.
Differential diagnosis of insulinoma is carried out with non-pancreatic tumors (liver, adrenal gland, various mesenchymomas). Hypoglycemia is observed with all these tumors. Non-pancreatic tumors differ from insulinomas in their large size (1000-2000 g). Tumors of the liver, adrenal cortex and various mesenchymomas have such sizes. Neoplasms of this size are easily detected by physical or conventional x-ray examination methods. Great difficulties arise in diagnosing insulinoma with the secret exogenous use of insulin preparations. The main evidence of exogenous use of insulin is the presence of antibodies to insulin in the patient’s blood, as well as low levels of C-peptide with a high level of total IRI. Endogenous secretion of insulin and C-peptide is always in equimolar ratios.
Nesidioblastosis - hypoglycemia in children caused by the total transformation of the ductal epithelium of the pancreas into β-cells, occupy a special place in the differential diagnosis of insulinoma. Nesidioblastosis can only be established morphologically. Clinically, it manifests itself as severe, difficult-to-correct hypoglycemia, which forces us to take urgent measures to reduce the mass of pancreatic tissue. The generally accepted volume of surgery is 80-95% resection of the gland. Treatment of insulinoma
The only radical treatment for insulinoma is surgery. Conservative methods of treatment are used only in inoperable patients, and also as means that temporarily eliminate hypoglycemia and are used to prepare the patient for surgical treatment.
Conservative therapy for insulinoma includes relief and prevention of hypoglycemic conditions and impact on the tumor process. For this purpose, various hyperglycemic agents are used. Traditional hyperglycemic agents include adrenaline and norepinephrine, glucagon, and glucocorticoids. However, their effect is short-lived and the parenteral route of administration of most of them limits their use.
For example, the hyperglycemic effect of glucocorticoids occurs when large doses of drugs that cause Cushingoid manifestations are used. Some authors note a positive effect on glycemia of diphenylhydantoin (Difenin) at a dose of 400 mg/day. The hyperglycemic effect of this non-diuretic benzothiazide is based on inhibition of insulin secretion from tumor cells. The drug is used at a dose of 100-600 mg/day in 3-4 doses. Available in capsules of 50 and 100 mg, due to its pronounced hyperglycemic effect it can be used for a long time.
When treating insulinoma, preference is given to drugs that have a hyperglycemic effect.
Performing surgical operations on the pancreas is complicated by its anatomical features, location in a hard-to-reach area, in close proximity to a number of vital organs, increased sensitivity to surgical trauma, the digestive properties of its juice, proximity to extensive nerve plexuses, and connection with reflexogenic zones. Due to appropriate preoperative preparation, selection of the most rational method of pain relief, minimally traumatic manipulations when searching for and removing a tumor, and carrying out preventive and therapeutic measures in the postoperative period, it is possible to reduce the risk of surgical intervention (Nikolaev O.B. and Weinberg E.G., 1968).
Thus, the main method of treatment with insulin is surgical, and conservative therapy is prescribed in inoperable cases, if the patient refuses surgery, as well as in unsuccessful attempts to detect a tumor during surgery. In this case, drugs that have a hyperglycemic effect are used.
Literature
1. Antonov A.V./Guide for doctors. Clinical endocrinology.-1991.- P. 262-274. 2. Manusharova R.A./Functional state of the pancreas in patients with insulinomas before surgery and in the long term after tumor removal. Author's abstract. dis. Ph.D. honey. Sciences. - 1972. 3. Klyachko V.R., Manusharova R.A., Sertsman V.I. and others. Test with leucine in the diagnosis of insulinoma.//Soviet Medicine.-1972.- No. 6.- P. 18-22. 4. Manusharova R.A., Frenkel G.M., Klyachko V.R. Problems of endocrinology.-1973.- No. 2.- P. 30-37. 5. Manusharova R.A. Functional state of the insular apparatus of the pancreas in patients with insulinomas in the long term after surgical treatment. // Problems of endocrinology. - 1972. - No. 5. - P. 17-21. 6. Nikolaev O.V., Weinberg E.G., Manusharova R.A.//Comparative assessment of tests with tolbutamide and leucine for insulinomas. Surgery.- 1972.- No. 8.- P. 109-113. 7. Nikolaev O.V., Weinberg Z.G. Insuloma - M., Medicine, 1968. 8. Broder L.E., Carters K.//Ann. Intern. Med.- 1973. 79, No. 4.- P.108-118. 9. Eastman RC, Come SE, Strewler QJ, et al. WJ.Clin.Endocr.-1977. - vol.44, No. 1.-H/142-148. 10. Okada Yosuke, Tanikawa Takahisa, Inokuchi Nobuo, et al. // J. Jap. Diabetes Soc. - 2002. - vol.45. P.815—820.
Symptoms of hyperinsulinism
Symptoms of hyperinsulinism depend on the degree of low blood glucose levels. The onset of an attack is characterized by:
- acute need for satiety, strong feeling of hunger;
- sweating increases;
- general malaise and weakness are felt;
- tachycardia increases.
If the patient is not provided with emergency assistance, the following signs are added:
- loss of orientation in space;
- trembling, numbness and tingling in the arms and legs.
Subsequent symptoms are aggravated by the following symptoms:
- fear;
- anxiety;
- irritability;
- convulsions;
- visual impairment;
- the patient loses consciousness and falls into a coma.
A person should eat as often as possible to prevent complications of the condition, which leads to weight gain.
Hyperinsulinism has three degrees of development:
- Mild degree. It has no interictal period and does not affect the cerebral cortex. The disease can worsen no more than once a month and is quickly relieved by taking medications or eating sweet foods.
- Average degree. Characterized by the presence of attacks more than once a month. The patient may lose consciousness and fall into a coma. In the period between attacks, poor memory, inattention, and decreased thinking abilities are noted.
- Severe degree. Associated with frequent exacerbations with loss of consciousness and irreversible changes in the cerebral cortex. During the interictal period, memory loss, tremors of the limbs, sudden mood swings and irritability are observed.
It is very important to respond to symptomatic manifestations in a timely manner, since the patient’s life depends on it.
Pathogenesis
β-cell adenomas, constantly releasing insulin even at low glucose concentrations, cause the development of chronic hypoglycemia . Hyperinsulinism also causes increased glycogen breakdown in the liver and muscles. Glucose is an important component of metabolism and a source of energy for all tissues, especially the brain. The brain does not have glucose reserves, so about 20% of the glucose entering the body is consumed for its function. If the supply of glucose to the cerebral cortex stops, irreversible changes develop in its cells (death of cortical elements) and cognitive and other mental disorders occur.
Hypoglycemia causes the release of catecholamines , which is manifested by weakness , anxiety , sweating , rapid heartbeat, trembling, and excitability. As a result of hypoglycemia, all types of metabolism in the brain slow down, vascular tone decreases and blood flow to the brain increases due to vascular spasm in the periphery. All this leads to the development of cerebral edema .
Diagnostics
The diagnosis of hyperinsulinism is made based on the results of the following studies:
- interviewing the patient, listening to complaints;
- collecting anamnesis (during the perinatal period, the condition of the mother during pregnancy, the presence of concomitant diseases, hereditary predisposition to the disease).
Laboratory testing methods:
- daily checking of blood glucose using a portable glucometer;
- assessment of glucose needs - a special calculation formula is used;
- fasting test - carried out if a congenital form of hyperinsulinism is suspected: for each age there is a norm for the time of fasting, after which the level of insulin, ketone bodies, free fatty acids, ammonium is checked, a blood test is taken for lactate;
- glucagon test - the patient is given a certain dose of the drug and after a certain time the blood glucose level is checked;
- stimulation studies - protein load test, exercise test.
Genetic testing involves checking specific genes and regions of chromosomes for mutations.
Additional procedures:
- ultrasound diagnostics of the abdominal cavity;
- scintigraphy;
- Magnetic resonance imaging of the pancreas and brain.
The doctor is obliged to differentiate with Zollinger-Ellison syndrome, diabetes mellitus, epilepsy, head tumors, psychosis, and neurosis.
List of sources
- Demidova T. Yu., Titova V. V. Long-term relapse of insulinoma in clinical practice // Breast Cancer. 2018; 11 (II): 122-125.
- Shevchenko Yu. L., Karpov O. E., Stoyko Yu. M. et al. Modern diagnostics and surgical tactics for pancreatic insulinomas // Bulletin of the National Medical and Surgical Center named after. N.I. Pirogova. 2016; vol. 11, no. 1: 6-9.
- Khatsimova L.S., Karonova T.L., Tsoi U.A., Yanevskaya L.G., Grineva E.N. Insulinoma: diagnostic approaches and medical tactics / Problems of endocrinology 2017; 63(4): 212-218.
- Kalinin A.P. et al. Insulinoma. Medical newspaper, 2007, No. 45, p. 8–9.
- Dedov I. I., Melnichenko G. A., Krivko A. A., Kuznetsov N. S., Troshina E. A. Long-term results of surgical treatment of insulinoma // Obesity and Metabolism. — 2014. No. 3(40), p. 18-23.
Treatment of hyperinsulinism
Treatment of hyperinsulinism depends on the cause of the disease. A patient with an organic origin is sent for a surgical procedure - partial resection of the pancreas or total pancreatectomy. The extent of surgical intervention will depend on the location of the pathology and its size.
After surgical procedures, medication and an appropriate low-carbohydrate diet are prescribed. Stabilization of the condition occurs within a month after removal of the tumor.
When a malignant tumor is detected, chemotherapy is prescribed. When a functional form is detected, the underlying disease is treated.
Diet is mandatory for any type of hyperinsulinism. Carbohydrate consumption is kept to a minimum; it is preferable to consume complex carbohydrates: whole grain cereals, nuts, pasta, rye bread. You should eat as often as possible, up to 6 times a day.
If the patient feels an attack approaching, it is worth drinking sweet tea, eating candy or white bread. During loss of consciousness, a 40% glucose solution is administered. If there are convulsions, injections of tranquilizers are indicated. A person is taken out of serious conditions in the intensive care unit.
Diet
Diet 15 table
- Efficacy: therapeutic effect after 2 weeks
- Timing: constantly
- Cost of food: 1600-1800 rubles per week
Before surgery, patients are advised to eat frequently (8-10 times a day). It should contain a sufficient amount of protein and carbohydrates. To avoid hypoglycemic conditions at night, you need to have protein foods (meat, eggs, cheese, cottage cheese) for dinner. During the day, the patient should have carbohydrates with him (sweets, sugar, gingerbread, sweet cookies), which can prevent an attack at the first signs of hypoglycemia.
Possible complications
Hyperinsulinism can lead to severe and irreversible consequences that are incompatible with the patient’s life.
Main complications of the disease:
- stroke;
- heart attack;
- coma;
- problems with memory and speech;
- parkinsonism;
- encephalopathy;
- diabetes;
- obesity.
The prognosis will depend on the severity of the disease and the cause of its occurrence. If a benign tumor is detected, the lesion is eliminated, and the patient recovers in 90% of cases. If the tumor is malignant and surgery is not possible, the survival rate is low.
Forecast
The prognosis for a benign tumor with surgical intervention performed in a timely manner is favorable in 90% of cases - patients experience clinical recovery after removal of the tumor. With early diagnosis and treatment, changes in the central nervous system disappear. With a longer duration of the disease and constantly recurring attacks, irreversible changes in the brain remain.
In 5-10% there are malignant insulinomas that metastasize to the liver. With metastases, survival is no more than 2 years. For malignant tumors, radical surgery and chemotherapy relieves patients from clinical manifestations and allows them to prolong life by more than 4 years.
Diseases with similar symptoms
Hypoglycemia (overlapping symptoms: 7 out of 20)
Glucose plays the role of the most important source of energy in the human body. This universal fuel, contrary to popular belief, is found not only in sweets: glucose is found in all foods containing carbohydrates (potatoes, bread, etc.).
Normal blood glucose levels are approximately 3.8–5.8 mmol/L for adults, 3.4–5.5 mmol/L for children, and 3.4–6.5 mmol/L for pregnant women. However, sometimes pathological conditions arise when blood glucose levels differ significantly from the norm. One such condition is hypoglycemia.
Did you like the article? Share with friends on social networks: