Percussion of the heart - a method for determining its boundaries
The anatomical position of any organ in the human body is determined genetically and follows certain rules. For example, the stomach in the vast majority of people is located on the left in the abdominal cavity, the kidneys are on the sides of the midline in the retroperitoneal space, and the heart occupies a position to the left of the midline of the body in the human chest cavity. The strictly occupied anatomical position of the internal organs is necessary for their full functioning.
During an examination of a patient, a doctor can presumably determine the location and boundaries of a particular organ, and he can do this with the help of his hands and hearing. Such examination methods are called percussion (tapping), palpation (palpation) and auscultation (listening with a stethoscope).
The boundaries of the heart are determined mainly using percussion, when the doctor uses his fingers to “tap” the front surface of the chest, and, focusing on the difference in sounds (voiceless, dull or voiced), determines the estimated location of the heart.
The percussion method often makes it possible to suspect a diagnosis even at the stage of examining the patient, before prescribing instrumental research methods, although the latter still play a leading role in the diagnosis of diseases of the cardiovascular system.
Percussion - determining the boundaries of the heart (video, lecture fragment)
Percussion – Soviet educational film
Heart defects
Rubella
Cold
Stroke
Atherosclerosis
Diabetes
4543 19 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Heart defects: causes, symptoms, diagnosis and treatment methods.
Definition
Heart disease is defined as an atypical or abnormal structure of its structures (chambers, valves, large vessels), which is a consequence of disturbances in the formation and development (congenital heart disease) or various pathological changes (acquired heart disease). As a result of the formation of this pathology, the functioning of the heart is disrupted and oxygen deficiency of organs and tissues of the body is formed, which can ultimately lead to heart failure.
Causes of heart defects
In humans, the blood returning to the heart from all organs and tissues (oxygen-poor blood) passes through the right atrium and then through the right ventricle into the pulmonary artery, and from there it enters the lungs. In the lungs, the blood is enriched with oxygen, releases carbon dioxide and enters the left atrium and left ventricle, and from there it is pumped to all organs and tissues through the aorta, and then through smaller arteries. The performance of the heart muscle depends on the functioning of the valves, which, when contracting, freely allow blood to flow into the next section, and when relaxing, do not allow blood to flow back.
If the function of the valves is impaired, the function of the heart is also impaired.
Congenital heart defects are very diverse. More than one and a half hundred different variants of atypical heart structure have been described. About one in 100 babies is born with a heart defect. Common heart pathologies diagnosed in infancy and childhood are atrial and ventricular septal defects (the openings between the chambers of the heart). Often the defects are combined with anomalies of the valvular apparatus of the heart or large vessels. The most common congenital heart defect is the bicuspid aortic valve, which opens with every heartbeat, allowing blood to flow from the heart to all organs. A normal aortic valve has three leaflets.
Bicuspid aortic valve does not usually cause problems during infancy or childhood, so it is often not diagnosed until adulthood.
The causes of congenital heart defects include genetic, environmental and infectious. In addition, their formation can be caused by certain diseases (gestational diabetes mellitus, rubella and systemic lupus erythematosus) in the mother, taking certain medications, drugs and alcohol during pregnancy, and other factors.
Acquired defects are anomalies and defects of the heart valves, its openings or partitions between the chambers, and the vessels extending from it, which appeared during life under the influence of morphological and functional changes in the functioning of the heart. The mitral valve is affected more often than the aortic valve. Pathologies of the tricuspid (tricuspid) valve and pulmonary valve are less common. Diseases can manifest at any age under the influence of atherosclerosis, cardiosclerosis, ischemic or hypertension, rheumatism, systemic pathology, trauma, syphilis and some other reasons. Also, degenerative changes in the valves lead to valvular heart defects - as the disease develops, their structure and function are disrupted, which causes a restructuring of hemodynamics, overload of the corresponding parts of the heart occurs, hypertrophy of the heart muscle, and impaired circulation in the heart and in the body as a whole.
Classification of the disease
It is customary to highlight:
- defects of the “white” type, when there is no tendency to mix arterial and venous blood;
- “blue” type defects - venous blood enters the arterial bed, resulting in oxygen deficiency.
Type of functional pathology:
- stenosis - as a result of the pathological process, deformation of the valve tissue occurs and the hole through which blood flows to the next part of the heart narrows;
- valve insufficiency - failure of the heart valves to close due to changes in shape, their shortening as a result of scarring of the affected tissues;
- combined and concomitant heart defects:
- combined – in the presence of both stenosis and insufficiency of one valve;
- combined – when several valves are affected at once.
Based on the reasons for their formation, acquired defects are classified as follows:
- degenerative, or atherosclerotic (occur in 5-6% of cases) - more often these processes develop after 40-50 years, when calcium is deposited on the leaflets of the affected valves, which leads to the progression of the defect;
- rheumatic, developing against the background of rheumatic diseases (80% of cases);
- defects that arise as a result of inflammation of the inner lining of the heart (endocarditis);
- syphilitic (in 5% of cases).
Based on the general hemodynamic condition, compensated, subcompensated and decompensated heart defects are distinguished.
Symptoms of heart defects
Clinical symptoms of heart defects include shortness of breath, weakness, fatigue, swelling of the lower extremities, sleep disturbances, interruptions in heart function, arrhythmia (usually tachycardia), change in skin color (blueness or pallor), swelling of the veins of the neck and head, causeless anxiety, pressing pain in the heart area (especially during physical activity) or between the shoulder blades, in rare cases - loss of consciousness.
Specific symptoms of congenital heart defects depend on the patient's age. Because normal circulation of oxygen-rich blood is essential for normal growth and development, infants may experience difficulty or rapid breathing, poor appetite, sweating or increased breathing during feeding, cyanosis of the lips and/or skin, unusual irritability, or failure to gain weight. .
Children and adolescents may experience decreased exercise tolerance, dizziness, and fainting.
Most serious heart defects in children are identified based on symptoms noticed by parents and abnormalities found when examined by a doctor. Impaired blood flow through the heart usually manifests as a heart murmur that can be heard with a stethoscope. Abnormal heart murmurs are often loud or harsh. However, in the vast majority of cases, heart murmurs noted in childhood are functional and not caused by heart defects.
The severity and nature of symptoms depend on the location of the affected valve. With valve defects of the left half of the heart (mitral and aortic), the lungs are primarily affected, since blood stagnates in their vessels, which is manifested by shortness of breath and cough. In addition, there are signs of insufficient blood supply to the brain and the heart itself, dizziness, fainting, and angina. In the presence of cyanosis, one of the most common pathologies is tetralogy of Fallot (restriction of blood flow to the lungs).
When the valves of the right half of the heart (the tricuspid and pulmonary valves) malfunction, blood stagnates in the vessels of the systemic circulation, so all organs except the lungs suffer. Swelling of the legs and feet, ascites (accumulation of fluid in the abdominal cavity), enlarged liver, and other lags in weight gain develop.
Signs of acquired defects are often combined with other heart diseases, in particular coronary artery disease, which makes their clinical differentiation difficult.
Diagnosis of heart defects
Diagnostic measures carried out to detect heart defects require an integrated approach, but always begin with collecting an anamnesis: the doctor finds out the patient’s complaints, the time and circumstances of their manifestation, intensity, and hereditary factors. Next, a physical examination is carried out, which includes visual inspection, palpation, percussion (tapping), auscultation (listening).
Laboratory tests that are prescribed for suspected heart disease:
- clinical blood test;
Normal values for the boundaries of cardiac dullness
Normally, the human heart has a cone shape, is directed obliquely downwards, and is located in the chest cavity on the left. On the sides and top the heart is slightly covered by small sections of the lungs, in front by the anterior surface of the chest, behind by the mediastinal organs, and below by the diaphragm. A small “open” area of the anterior surface of the heart is projected onto the anterior chest wall, and just its borders (right, left and upper) can be determined by tapping.
boundaries of relative (a) and absolute (b) dullness of the heart
Percussion of the projection of the lungs, whose tissue has increased airiness, will be accompanied by a clear pulmonary sound, and tapping the area of the heart, whose muscle is a denser tissue, will be accompanied by a dull sound. This is the basis for determining the boundaries of the heart, or cardiac dullness - during percussion, the doctor moves his fingers from the edge of the anterior chest wall to the center, and when the clear sound changes to a dull sound, he marks the border of dullness.
The boundaries of relative and absolute dullness of the heart are distinguished:
- The boundaries of relative dullness of the heart are located along the periphery of the projection of the heart and indicate the edges of the organ, which are slightly covered by the lungs, and therefore the sound will be less dull (dull).
- The absolute border marks the central area of the projection of the heart and is formed by an open area of the anterior surface of the organ, and therefore the percussion sound is more dull (dull).
Approximate values of the limits of relative cardiac dullness are normal:
- The right border is determined by moving the fingers along the fourth intercostal space from the right to the left, and is usually marked in the 4th intercostal space along the edge of the sternum on the right.
- The left border is determined by moving the fingers along the fifth intercostal space on the left to the sternum and marking along the 5th intercostal space 1.5-2 cm inward from the midclavicular line on the left.
- The upper border is determined by moving the fingers from top to bottom along the intercostal spaces to the left of the sternum and is marked along the third intercostal space to the left of the sternum.
The right border corresponds to the right ventricle, the left border corresponds to the left ventricle, and the upper border corresponds to the left atrium. The projection of the right atrium cannot be determined using percussion due to the anatomical location of the heart (not strictly vertical, but obliquely).
In children, the boundaries of the heart change as they grow, and reach the values of an adult after 12 years.
Normal values in childhood are:
| Age | Left border | Right border | Upper limit |
| Up to 2 years | 2 cm outward from the midclavicular line on the left | Along the right parasternal (parasternal) line | At the level of the second rib |
| From 2 to 7 years | 1 cm outward from the midclavicular line on the left | Inward to the right parasternal line | In the second intercostal space |
| From 7 to 12 years old | Along the midclavicular line on the left | Along the right edge of the sternum | At the level of the third rib |
The aortic configuration is formed in all conditions accompanied by hypertrophy of the left ventricle and its overload (aortic defects, arterial hypertension of any origin). Signs of an aortic configuration are: a shift of the boundaries of relative cardiac dullness to the left in the IV-V intercostal spaces due to hypertrophy or dilatation of the left ventricle, the waist of the heart at the level of the III rib is emphasized and well defined, the angle between the vascular bundle and the left ventricle is approaching a straight line. Radiographically, the heart resembles a “boot” or “sitting duck” shape.
Among other pathological configurations, a peculiar configuration can be noted in effusion pericarditis - it resembles the shape of a trapezoid. With it, due to the accumulation of exudate or transudate in the pericardial cavity in a vertical position, mainly the lower parts of the relative cardiac dullness on the left and right expand. In the supine position, these boundaries decrease.
Determination of the boundaries of absolute cardiac dullness
When percussing an area of the heart not covered by the lungs, a dull sound is heard - this is an area of absolute cardiac dullness formed by the right ventricle. Percussion is carried out with the quietest percussion from the border of relative cardiac dullness inwards to an absolutely dull sound. The right one is determined in the 4th intercostal space to the right of the sternum, the left - in the 5th intercostal space to the left of the sternum, and the upper one - from top to bottom along the left edge of the sternum or retreating from it outward by 1 cm.
1. The right border of absolute cardiac dullness runs in the 4th intercostal space along the left edge of the sternum.
2. The left border is located at the level of the 5th intercostal space - 2-3 cm medially from the midclavicular line (or 1-1.5 cm medially from the border of relative cardiac dullness), the upper one is on the 4th rib.
Changing the boundaries of relative cardiac dullness in pathological conditions
1. Shifting the borders of relative dullness of the heart to the right is caused by expansion of the right ventricle (increased pressure in the a. pulmonalis with mitral defects, chronic diseases of the bronchopulmonary system, pulmonary embolism).
2. A shift of the border of relative dullness of the heart to the left at the level of the IV-V intercostal spaces occurs with expansion of the left ventricle (mitral valve insufficiency, aortic defects, arterial hypertension of any origin, coronary artery disease). It should be remembered that a sharply enlarged and hypertrophied right ventricle, pushing the left one, can sometimes shift the border of the relative dullness of the heart to the left.
3. When the diaphragm is high, the heart takes a horizontal position, which leads to an increase in its transverse size; when the diaphragm is low, on the contrary, its transverse size decreases.
4. The accumulation of fluid or air in one of the pleural cavities leads to a displacement of the borders of the heart to the healthy side, with atelectasis or shrinkage of the lungs, pleuropericardial adhesions - to the diseased side.
An increase in the boundaries of absolute cardiac dullness is observed:
1. with dilatation of the right ventricle,
2. with wrinkling and atelectasis of the lungs,
3. after pneumonectomy,
4. with a tumor of the mediastinum,
5. when exhaling deeply,
6. with exudative pleurisy or hydrothorax on the left and compaction of the edges of the left lung,
7. with exudative pericarditis,
8. with sharp hypertrophy of the right ventricle.
A decrease in the boundaries of absolute cardiac dullness is observed:
1. with a deep breath,
2. with a low aperture,
3. for pulmonary emphysema,
4. during an attack of bronchial asthma,
5. for pneumothorax,
6. with pneumopericardium.
Expansion of the vascular bundle is observed in atherosclerosis, syphilis, as well as aneurysms of the ascending part and aortic arch.
Auscultation of the heart
Auscultation of the heart is based on the fact that when the heart contracts and vibrates its main structures (valves, contractile myocardium, large vessels), sounds arise, which in ordinary medical practice are called heart sounds.
Auscultation of the heart is the most important method for diagnosing many diseases, especially congenital and acquired heart defects. To master this method, the doctor must have a good ear for music, as well as a clear understanding and knowledge of the basic patterns of intracardiac hemodynamics, the genesis of sound phenomena in the heart, the sequence and general rules of auscultation of the heart, the projection of the valves onto the chest and the points of their best auscultation.
Auscultation rules. It is carried out in a calm, comfortable environment, noise and extraneous sounds should be excluded.
1. Auscultation of the heart is carried out with the patient standing and lying down, and, if necessary, on the left, right side, after physical activity.
2. The stethoscope should fit tightly to the point being listened to.
3. Listening to the heart is most often done with a stethoscope, which makes it possible to isolate all sounds obtained during auscultation at a certain point. Direct auscultation can be used much less frequently.
4. Listening should be carried out in different phases of breathing. It is imperative to listen to the heart during the breath-holding phase, during inhalation and exhalation, in order to exclude the influence of respiratory sounds on the auscultatory picture of the heart.
5. Heart valves are auscultated in descending order of frequency of their damage. It must be remembered that the places of the anatomical projection of the valves on the chest do not coincide with the points of their auscultation (Fig. 36). In particular:
• The mitral valve is projected at the site of attachment of the third rib to the sternum on the left, and its listening point is the apex of the heart.
• The aortic valve is projected onto the middle of the sternum at the level of attachment of the 3 ribs to the sternum, but is heard in the 2nd intercostal space at the right edge of the sternum.
• The projection of the pulmonary artery valve and the point of listening to it coincide and is located in the second intercostal space at the left edge of the sternum.
• The tricuspid valve is projected in the middle of the distance between the place of attachment of the third rib to the sternum on the left and the 5th rib on the right, and the point of its best auscultation is at the base of the xiphoid process.
Rice. 36. Points of projection and auscultation of heart valves: 1- mitral; 2- aortic valves; 3- pulmonary valve; 4- tricuspid valve.
The first place to listen is the mitral valve, at the apex of the heart. Then the aortic valve - 2nd intercostal space on the right at the edge of the sternum. Then the pulmonary valve - 2nd intercostal space on the left at the edge of the sternum and the tricuspid valve (right atrioventricular) - the base of the xiphoid process of the sternum. 5th point - Botkin-Erb point is located in the third intercostal space on the left at the edge of the sternum. This is an additional listening point for the aortic valve. The Botkin-Erb point has been proposed especially for the early detection of aortic valve insufficiency.
6. If any noise is heard at the main points, then the entire region of the heart should be listened to.
Heart sounds
In healthy people, two tones are heard. The first sound occurs at the beginning of systole, which is why it is called systolic. The second sound occurs at the beginning of diastole, which is why it is called diastolic.
The first tone consists of 3 components: valve, muscle and vascular. The sequence of formation of these components becomes clear during the phase analysis of left ventricular systole. As is known, it consists of phases of asynchronous, isometric tension and the expulsion phase. During the phase of asynchronous contraction, only individual muscle fibers enter a tonic state, therefore the possible influence of this phase on the formation of the first tone is insignificant. Of greatest importance is the subsequent isometric tension phase, when virtually the entire contractile myocardium comes into tone. In this case, the pressure in the ventricles increases sharply, and a pressure gradient (difference) between the ventricles and atria occurs. Since the pressure in the ventricles is higher, the atrioventricular valves close and the most important component of the first sound, the valve sound, appears. At the same time, the muscle component is partially formed during this phase. The next moment, the expulsion phase begins, in which the muscular component is finally formed (as a result of contraction of the left and right ventricles), as well as the vascular component of the first tone (oscillation of the initial parts of the aorta and pulmonary artery during the ejection of blood from the ventricles). The “period of closed valves,” which is observed in the phase of isometric tension, is of utmost importance in the formation of a full-fledged I current. In this case, the atrioventricular valves are already closed, and the semilunar valves of the aorta and pulmonary trunk have not yet opened. The resulting closed system leads to a significant increase in intraventricular pressure, an increase in the potential energy of the ventricles, which is then realized in a loud, strong first tone. In the absence of a “closed valve period,” the first tone weakens.
Reasons for deviations from the norm
Focusing on the boundaries of relative cardiac dullness, which gives an idea of the true boundaries of the heart, one can suspect an enlargement of one or another cardiac cavity due to any diseases:
- A shift to the right (expansion) of the right border accompanies myocardial hypertrophy (enlargement) or dilatation (expansion) of the cavity of the right ventricle, expansion of the upper border - hypertrophy or dilatation of the left atrium, and displacement of the left - the corresponding pathology of the left ventricle. The most common expansion of the left border of cardiac dullness occurs, and the most common disease that leads to the borders of the heart expanding to the left is arterial hypertension and the resulting hypertrophy of the left chambers of the heart.
- With a uniform expansion of the boundaries of cardiac dullness to the right and left, we are talking about simultaneous hypertrophy of the right and left ventricles.
Diseases such as congenital heart defects (in children), previous myocardial infarction (post-infarction cardiosclerosis), myocarditis (inflammation of the heart muscle), dishormonal cardiomyopathy (for example, due to pathology of the thyroid gland or adrenal glands), long-term arterial hypertension. Therefore, an increase in the boundaries of cardiac dullness may lead the doctor to think about the presence of any of the listed diseases.
In addition to an increase in the boundaries of the heart caused by myocardial pathology, in some cases there is a shift in the boundaries of dullness caused by the pathology of the pericardium (heart lining) and neighboring organs - the mediastinum, pulmonary tissue or liver:
- Pericarditis, an inflammatory process of the pericardial layers, accompanied by the accumulation of fluid in the pericardial cavity, sometimes in a fairly large volume (more than a liter), often leads to a uniform expansion of the boundaries of cardiac dullness.
- Unilateral expansion of the borders of the heart towards the affected side is accompanied by pulmonary atelectasis (collapse of a non-ventilated area of lung tissue), and towards the healthy side – accumulation of fluid or air in the pleural cavity (hydrothorax, pneumothorax).
- Displacement of the right border of the heart to the left side is rare, but still observed in severe liver damage (cirrhosis), accompanied by a significant increase in liver volume and its upward displacement.
Exam / Lectures on PVB / No. 09 Cardiac percussion
LECTURE No. 9
PERCUSSION OF THE HEART
Percussion or percussion of the heart involves determining the size, shape, position of the heart and vascular bundle. The physical basis of cardiac percussion is the same as described earlier.
The heart is mostly located in the left half of the chest and can be schematically represented as an obliquely located cone, the apex of which corresponds to the apex of the heart. It is directed down and to the left. The base of the heart faces upward. It is believed that only one third of the anterior surface of the heart lies in the right half of the chest, counting from the linea mediana anterior. Two thirds of it are located in the left half of the chest. The heart is, as it were, fixed from above by large vessels (aorta, pulmonary artery, superior vena cava). The right ventricle of the heart lies on the left dome of the diaphragm. The right, upper and left borders of the heart are identified, which are determined by percussion. The lower border of the heart is not determined! The semilunar space of Traube is located below the heart. In the projection of this space there is a gas bubble of the stomach, which gives a tympanic sound to percussion.
When percussed, the heart, as a muscular airless organ with blood contained in it, gives a dull sound. Therefore, over the area of the anterior chest wall to the left of the sternum, to which the heart is directly adjacent, a dull sound occurs upon percussion, called the zone of absolute dullness of the heart. The lungs surrounding the heart on both sides and above contain sound and, when percussed, give a clear pulmonary sound. The heart on the right and left is partially covered by the lungs. Therefore, when percussion occurs over this part of the heart, a dull percussion sound occurs. Dullness obtained at the border separating the airy lung tissue from the airless tissue of the heart is called relative, or deep, dullness of the heart.
Cardiac percussion can be performed in both a vertical and horizontal position of the patient. However, it must be taken into account that the size of cardiac dullness in a horizontal position of the patient is slightly larger than in a vertical position. This is due to the mobility of the heart and the displacement of the diaphragm when the body position changes. Typically, cardiac percussion is performed with the patient standing or sitting with arms down, with normal quiet breathing. In seriously ill patients, percussion can be performed in a horizontal position of the patient's body. When performing percussion, the doctor should take a position that allows him to comfortably place a finger-pessimeter and apply percussion blows. When percussing the heart, mediated finger-on-finger percussion is usually used. Percussion according to Sokolsky is most often used. When determining the boundaries of absolute dullness of the heart, the quietest threshold percussion according to Goldscheider (Goldscheider) with finger placement according to Plesch is often used. Some clinicians, especially in pediatric practice, use percussion according to Obraztsov or Yanovsky.
When tapping the heart, the pessimeter finger should fit snugly to the surface of the chest parallel to the expected border of the heart. Percussion blows should be of medium strength and directed strictly in the sagittal direction. Typically, percussion is carried out in the direction from a clear pulmonary sound to a dull one,
those.
from the lungs to the heart, although some clinicians prefer to tap from dull to clear. In all cases, the boundary is marked along the edge of the finger facing towards the clear pulmonary sound,
i.e. to the side facing the lungs.
When percussing the borders of the heart, first the right, then the left, then the upper borders are determined
his.
Determination of the boundaries of relative cardiac dullness
Right contour of relative cardiac dullness
and the vascular bundle in the direction from top to bottom is formed by the superior vena cava to the upper edge of the 3rd rib, then down - by the right atrium.
The left contour of the relative dullness of the heart
is formed by the left part of the aortic arch, then by the pulmonary trunk, at the level of the 3rd rib by the left atrial appendage, further down by a narrow strip of the left ventricle. Thus, the expansion of each of the boundaries of the relative dullness of the heart reflects an increase in certain chambers of the heart: the right border - the expansion of the right atrium, the left border - the left ventricle, the upper border - the left atrium. An increase in the size of the right ventricle cannot be detected when assessing the boundaries of relative dullness of the heart, since it forms the anterior surface of the heart.
When determining the boundaries of relative dullness, the heart is percussed along the intercostal spaces to avoid lateral propagation of vibrations along the ribs. The percussion blow should be of medium strength. It is necessary to ensure that the pessimeter finger is pressed tightly against the chest wall, thereby achieving a deeper distribution of vibration.
Determination of the right border of relative dullness of the heart begins with determining the upper border of relative hepatic dullness (or the lower border of the right lung), i.e. height of the right dome of the diaphragm. Percussion is carried out along the right mid-clavicular line from the 3rd intercostal space down until a dull percussion sound appears. The upper limit of relative hepatic dullness (or the lower limit of the right lung) is normally located at the level of the 5th rib. Then the plessimeter finger is turned at a right angle (parallel to the expected border of the heart), placed 1 rib above the found edge of the lung
and begin to percussion along the intercostal space towards the right edge of the sternum.
Carefully monitor the nature of the resulting percussion sound, i.e., the transition from a clear pulmonary sound to a dull one. At the border of a dull percussion sound, a mark is made along the edge of the finger facing the clear pulmonary sound. This mark corresponds to the right border of the relative dullness of the heart. In a healthy person, it is located 1 - 1.5 cm outward from the right edge of the sternum in the 4th intercostal space
and is formed by the right atrium.
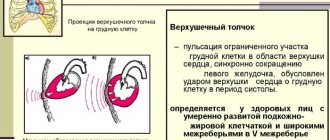
Before proceeding with percussion determination of the left border of the relative dullness of the heart, the location of the apex beat, which is formed by the left ventricle of the heart, should be palpated. In the case when percussion is performed on a woman with a developed mammary gland, the doctor asks her to lift and hold the mammary gland with her left hand. If the apical impulse cannot be detected, percussion is carried out along the 5th intercostal space, and then along the 6th intercostal space, starting from the anterior axillary line, moving the finger towards the heart. The plessimeter finger is placed across the intercostal space, i.e. parallel to the expected border of relative dullness of the heart. They try to apply a percussion blow strictly in the sagittal direction. If dullness of percussion sound is detected, a mark is placed along the outer edge of the finger facing the clear pulmonary sound. This mark corresponds to the left border of the relative dullness of the heart and is formed by the left ventricle of the heart. In a healthy person, it is located 1–2 cm medially from the left midclavicular line in the 5th intercostal space
and coincides with the apical impulse.
When determining the upper limit of the relative dullness of the heart, the plessimeter finger is placed 1 - 1.5 cm away from the left sternal line (from the left edge of the sternum) parallel to the ribs. Percussion begins in the 1st intercostal space and moves the finger – plessimeter – down until the sound becomes dull. A mark is made along the upper edge of the finger in the direction of a clear percussion sound. In a healthy person, this border runs along the 3rd rib
and is formed by the left atrial appendage.
The lower border of the heart is not determined by percussion, since the heart here comes into contact with the diaphragm and liver.
Having determined the boundaries of the relative dullness of the heart, measure the diameter of the heart
measuring tape.
The diameter of the heart is defined as the sum of perpendiculars to the anterior midline from the most distant points of the right and left borders of the heart. Normally, the distance from the right border of the relative dullness of the heart to the anterior midline is 3–4 cm, from the left border of the relative dullness of the heart to the anterior midline is 8–9 cm. Accordingly, the diameter of the relative dullness of the heart is 11–13 cm.
In practice, it is determined and long heart
.
The length of the heart is the distance from the right cardiovascular angle (the intersection of the border of cardiac dullness with the lower edge of the 3rd rib) to the apex of the heart (the left border of relative dullness of the heart). Normally, in a healthy person, the length of the heart is 13–15 cm.
width and height were previously determined
. The width of the heart is the sum of perpendiculars to the length of the heart from the most distant point of the upper left contour (the place of transition of the vascular bundle to the left border of the heart) and from the hepatic cardiac angle. The height of the heart consists of 2 segments: 1 – from the highest point of the upper border to the base of the xiphoid process and 2 – from the base of the xiphoid process to the lower contour of the heart. Since the lower contour cannot be determined, the second component is taken equal to 1/3 of the first.
The boundaries of the heart can change both due to a number of physiological circumstances and due to some pathological conditions. The area of absolute dullness of the heart will increase with scarring, wrinkling or inflammatory compaction of the anterior edges of the lungs, with exudative pleurisy, and large tumors of the posterior mediastinum. An increase in the size of the relative dullness of the heart also occurs with a high position of the diaphragm in hypersthenics, patients with flatulence and ascites, and in pregnant women. In this case, the heart takes a horizontal position and is closer to the anterior chest wall. An increase in the size of the relative dullness of the heart, associated with an increase in the size of the heart itself, most often occurs with expansion (dilatation) of the chambers of the heart. It depends only to a small extent on the increase in thickness (hypertrophy) of the myocardium. Hypertrophy of the heart muscle alone usually cannot cause an increase in the size of the relative dullness of the heart, since such a slight increase in the size of the heart cannot be reliably determined using percussion.
As the chambers (cavities) of the heart expand, the boundaries of cardiac dullness shift in different directions. The shift of relative dullness of the heart to the right is caused by expansion of the right atrium. To a lesser extent, this is due to dilation of the right ventricle of the heart, displacing the right atrium to the right. Such an increase in the size of the relative dullness of the heart to the right can occur with stenosis (narrowing) of the opening of the tricuspid valve, tricuspid valve insufficiency, stenosis of the pulmonary artery, with late stages of mitral valve stenosis, leading to hypertension in the pulmonary circulation, as well as with other conditions leading to pulmonary tipertension.
A shift of the borders of relative dullness of the heart to the left occurs with dilatation and hypertrophy of the left ventricle of the heart. This occurs in patients with aortic heart defects, in the initial stages of mitral valve insufficiency, general atherosclerosis, in patients with hypertension and other diseases leading to arterial hypertension in the systemic circulation. With a significant increase in the size of the right ventricle of the heart, a shift in the boundaries of the relative dullness of the heart to the left may also be noted due to the pushing of the left ventricle to the left and posteriorly.
An upward shift of the border of relative dullness of the heart is usually caused by a significant expansion of the left atrium. This can occur with narrowing (stenosis) of the mitral valve opening, as well as with mitral valve insufficiency. An increase in the boundaries of relative dullness of the heart in both directions is detected with lesions of the heart muscle - myocardiosclerosis, acute and chronic myocarditis.
An increase in the boundaries of the heart in all directions is observed with a simultaneous increase in the left and right ventricles of the heart and the left atrium. This can happen with combined valvular heart defects, when several heart valves are affected and there are signs of cardiac decompensation. This change in the boundaries of the heart is called “bull’s heart” (cor bovinum).
An increase in the relative dullness of the heart in all directions can also occur with the accumulation of fluid in the pericardial cavity. In this case, the shape of cardiac dullness takes the form of a truncated triangle or trapezoid, with the base facing down.
A decrease in the size of the relative dullness of the heart often occurs with prolapse of the diaphragm, enteroptosis, pulmonary emphysema, and pneumothorax. In these cases, the heart not only moves downwards, but also takes on a more vertical position, called a hanging or drip heart.
The accumulation of fluid or air in one of the pleural cavities leads to a shift in the boundaries of cardiac dullness towards the healthy side. With the development of atelectasis or with shrinkage of the lung, with pleuropericardial adhesions, the boundaries of cardiac dullness shift to the affected side.
Determination of the configuration of cardiac dullness
, or the contour of the heart, is carried out by percussing strictly along the intercostal spaces, starting from the second intercostal space on the right and left and moving sequentially to the 5th - 6th intercostal spaces. The plessimeter finger is placed perpendicular to the intercostal spaces or parallel to the expected border of the heart. The mark of the found dullness is marked along the edge of the finger towards the clear pulmonary sound. Then the resulting points are connected with solid lines and the right and left contours of cardiac dullness are obtained.
The boundaries of the contour of cardiac dullness in relation to the anterior midline of the body are located in a healthy average-sized normosthenic as follows. The right border of the contour of cardiac dullness in the 2nd and 3rd intercostal spaces is spaced from the anterior midline by 3 cm, in the 4th intercostal space - by 4 cm. The left border of the contour of cardiac dullness in the 2nd intercostal space is spaced from the anterior midline by 3 cm, in the 3rd intercostal space - by 4 cm, in the 4th and 5th intercostal spaces - by 9 cm.
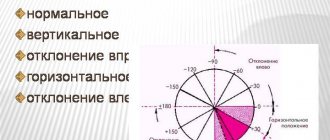
Depending on the disease the patient has, mitral and aortic configurations of the heart are distinguished. Before characterizing these concepts, it is necessary to introduce the term “heart waist”. The waist of the heart is the angle between the vascular bundle on the left and the left contour of the heart formed by its left ventricle. Normally, this angle is 140 - 150o.
The mitral configuration of the heart occurs with mitral heart defects - mitral valve insufficiency and advanced stage of mitral valve stenosis. It is characterized by enlargement of the left atrium of the heart. With a mitral configuration of the heart, the heart's waist flattens or even bulges due to a sharp increase in the left atrium.
The aortic configuration of the heart occurs in patients with aortic heart defects - aortic valve insufficiency and stenosis of the aortic mouth, as well as in severe hypertension. It is characterized by significant isolated enlargement of the left ventricle. At the same time, the waist of the heart becomes emphasized, the angle forming it approaches a straight line. The configuration of cardiac dullness is compared with the shape of a boot or the pose of a sitting duck.
After determining the boundaries of relative dullness of the heart, they begin to determine the boundaries of absolute dullness of the heart.
, i.e.
to the area of the heart not covered by the lungs. It is formed by the right ventricle of the heart
. The term "absolute dullness" is misleading to novice researchers, since they are looking for truly absolute dullness, such as is detected, for example, in the hip. The heart, even where it is not covered by the lungs, produces not an absolutely dull sound, but a dull sound with an admixture of tympanitis. This is due to the fact that it is surrounded by air-containing lungs, and is bordered below by the gas-containing stomach and large intestine. When percussing this area, an absolutely dull percussion sound is determined. When determining the extent of absolute dullness of the heart, the same principles are used as when determining the boundaries of relative dullness of the heart, but they use quiet or even the quietest percussion according to Goldscheider with finger placement according to Plesch.
There are 2 ways to determine the boundaries of absolute cardiac dullness. In the first method, determining the boundaries of absolute dullness of the heart, having determined the boundaries of relative dullness, they continue to percussion, but with quiet percussion, with weak blows without bouncing of the percussion finger, further towards the center until an absolutely dull percussion sound appears. The pessimeter finger should be pressed against the chest with considerable force. This achieves a greater spread of vibrations deeper in the direction of the percussion blow and less in the lateral directions.
First, the left, then the right, then the upper limit of absolute cardiac dullness are determined. The mark of the found border is made along the outer edge of the finger, from the dull sound towards the dull percussion sound. Normally, the right border of absolute cardiac dullness on the right goes along the left edge of the sternum
.
The left border of absolute cardiac dullness is usually 1–1.5 cm inward from the left border of relative cardiac dullness.
The upper border of absolute cardiac dullness is normally
located along the lower edge of the cartilage of the 4th rib on the left.
The second method of determining the boundaries of absolute cardiac dullness can be used more often with greater success than the simpler first method. It gives reliable results in all cases where the use of the first method causes questionable results. With this method, percussion is carried out starting from the zone of absolute dullness of the heart, usually from the 4th intercostal space at the left edge of the sternum. The finger-plessimeter is installed at this point according to the Pleshu method. Goldscheider's quietest or threshold percussion is used, when the result of a percussion blow is assessed not only by ear, but also by tactile vibration that occurs. The plessimeter finger is placed in such a way that the percussion blow is distributed strictly in the sagittal direction. The plessimeter finger is gradually moved in the direction of the points (borders) of relative dullness of the heart. The first addition of a pulmonary admixture to the percussion sound will indicate a transition from the region of absolute dullness to the region of relative dullness of the heart. The resulting dull sound is marked in the direction of the dull sound (from the dull sound).
If necessary, the boundaries of absolute dullness of the heart can be determined using Obraztsov’s tactile percussion, when to determine the boundaries of organs that do not contain air, they use not only hearing, but also the touch of greater or lesser resistance, greater or lesser density of the underlying tissues.
When working, it is advisable to determine the boundaries of cardiac dullness not only in 3 places (right, left and upper borders), but to systematically tap out all the dullness and draw its outline on the patient’s skin using a demographer.
Expansion of the boundaries of absolute dullness of the heart from the indicated boundaries in a healthy person indicates an enlargement of the right ventricle of the heart. However, it will also increase with the accumulation of fluid in the pericardial cavity. In this case, the boundaries of relative and absolute dullness of the heart may coincide. In addition, an increase in the size of absolute dullness of the heart can also occur with extracardiac pathology, for example, with shrinkage of the lungs covering the heart.
A decrease in the size of absolute dullness of the heart under physiological conditions is observed with deep inspiration. A pathological decrease in the size of absolute dullness of the heart is observed in patients with pulmonary emphysema. They experience a decrease in the size of the absolute dullness of the heart until it completely disappears and is replaced by a box sound. In patients with an attack of bronchial asthma, with pneumothorax, with pneumopericardium, with subcutaneous emphysema in the heart area, with a low diaphragm, a decrease in the size of absolute dullness of the heart also occurs.
Determination of the boundaries of the vascular bundle
.
Percussion determination of the boundaries of the vascular bundle, the main part of which is the aorta, is carried out at the level of the manubrium of the sternum in the 2nd intercostal space to the right and left of its edges. The pessimeter finger is placed in the 2nd intercostal space along the midclavicular line parallel to the expected dullness. When percussing, use quiet percussion. The pessimeter finger is gradually moved 0.5 - 1 cm towards the right edge of the manubrium of the sternum until a dull sound appears. At the site of the found dullness, a mark is made along the outer edge of the finger in the direction of the clear pulmonary sound. Then percussion is performed on the left in the same way and the left edge of the vascular bundle is found. The distance between the boundaries of the found dullness is measured with a centimeter tape. Normally, the width of the vascular bundle is 4–5 cm.
Usually, dullness of the percussion sound from the vascular bundle is obtained only on the sternum itself. When the aorta dilates, the dullness of the percussion sound extends beyond the contour of the sternum. With the expansion of the ascending aorta, the dullness of the percussion sound extends beyond the right edge of the sternum into the 2nd intercostal space. When the descending aorta expands, the dullness of the percussion sound extends beyond the left contour of the sternum. Lengthening the aorta results in dullness of percussion sound on both sides of the sternum. In the case of dilatation of the pulmonary artery, dullness of percussion sound is detected to the left of the sternum in the 2nd intercostal space or below this level.
12
Can changes in the boundaries of the heart manifest clinically?
If the doctor reveals expanded or displaced borders of cardiac dullness during examination, he should find out in more detail from the patient whether he has some symptoms specific to diseases of the heart or neighboring organs.
Thus, heart pathology is characterized by shortness of breath when walking, at rest or in a horizontal position, as well as swelling localized in the lower extremities and face, chest pain, and cardiac arrhythmias.
Pulmonary diseases are manifested by cough and shortness of breath, and the skin becomes bluish in color (cyanosis).
Liver diseases may be accompanied by jaundice, abdominal enlargement, stool disorders and edema.
In any case, expansion or displacement of the borders of the heart is not normal, and the doctor should pay attention to the clinical symptoms if he detects this phenomenon in the patient for the purpose of further examination.
When might treatment be needed?
Directly expanded or displaced borders of the heart cannot be treated. First, you should identify the cause that led to an enlargement of the parts of the heart or displacement of the heart due to diseases of neighboring organs, and only then prescribe the necessary treatment.
In these cases, surgical correction of heart defects, coronary artery bypass surgery or stenting of coronary vessels may be necessary to prevent recurrent myocardial infarction, as well as drug therapy - diuretics, antihypertensives, rhythm-slowing and other drugs to prevent the progression of enlargement of the heart.