Recovery from chemotherapy should not be a completely spontaneous, months-long process with unknown results. In any case, after some time, the troubles of drug antitumor treatment will significantly decrease, but recovery will go faster and more successfully only under the supervision of a doctor, or better yet, a team of specialists who are well versed in all aspects of the rehabilitation of cancer patients.
- Causes of bruises
- Symptoms of vein inflammation after chemotherapy
- Basic methods of treating veins
- How veins are restored after IVs: useful procedures
- Prevention of complications
Causes of bruises
A bruise or hematoma in cancer patients is common, because chemotherapy is associated with introduction into the body through the destruction of the skin - intravenous administration of drugs, which is not always possible without hemorrhage into the skin and tissue around the vessel. Antitumor drugs change the composition of the blood, in particular the number of platelets, increasing bleeding, and also increase the likelihood of blood clots fivefold, while chronically existing varicose veins only double the formation of blood clots.
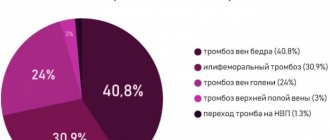
A malignant tumor changes the rheological properties of the blood, leading to the formation of blood clots. In every fifth patient, hidden thrombosis is detected before surgery. In intestinal and pancreatic cancer, excessive blood clot formation may be the first sign of a malignant disease. Chemotherapy, like the metastatic stage of any tumor, increases the likelihood of thrombosis by an average of five times. In the body of a cancer patient, two processes coexist simultaneously - excessive bleeding and increased coagulability.
Risk factors for thrombosis in cancer patients as in all “ordinary” people: high weight and age “after 40”, chronic vascular and heart diseases, diabetes mellitus, hypertension and, of course, varicose veins of the lower extremities.
These standard causes in an oncology patient are mixed with specific ones, that is, initiated by a malignant tumor and aggravated by the necessary treatment:
- compression of blood and lymphatic vessels by a tumor conglomerate;
- lymphostasis after removal of axillary lymph nodes, as a result of irradiation or removal of pelvic tissue with lymph nodes, as well as blockage of lymph outflow from the leg by metastatic inguinal ties;
- long-term use of hormonal drugs;
- stimulation of the red germ of hematopoiesis by erythropoietins;
- a permanently installed venous catheter for frequent drug infusions;
- restriction of mobility forced due to weakness;
- operations and radiation, as well as side effects of chemotherapy on blood vessels and blood cells.
To initiate a blood clot inside a vessel, a cancer patient needs only three reasons, and not necessarily all of them at once:
- damage to the inner lining of the vessel, which is common for intravenous chemotherapy;
- blood stagnation, which is called “poor circulation”, including as a result of tumor conglomerate;
- excessive coagulability along with impaired clot formation.
Book a consultation 24 hours a day
+7+7+78
So is it worth it or not to remove varicose veins?
A varicose vein is a tooth that is not affected by caries, and will not hurt as much. Complications of varicose veins develop slowly and gradually. This does not make them any less unpleasant or dangerous. A good treatment for varicose veins is timely treatment, before the symptoms of chronic venous insufficiency and thrombosis appear.
Good results in treating varicose veins without waiting for complications
Symptoms of vein inflammation after chemotherapy
Most chemotherapy drugs are used only in solution, not in tablets, which is explained by the instability of drug molecules to gastric juice and the strong irritating effect of cytostatics on the mucous membranes of the gastrointestinal tract. When the cytostatic comes into direct contact with the venous wall, it penetrates into endothelial cells and changes the DNA structure. The chemical reaction that occurs directs the endothelial cell to inflammatory changes or to death - apoptosis. The damage is aggravated by trauma to the vein wall from the injection needle or catheter.
Inflammation of the venous wall is phlebitis, to which risk factors for the formation of blood clots are quickly connected, and thrombophlebitis develops in the vein damaged by chemotherapy.
Phlebitis is manifested by pain , and during the process of administering a cytostatic, the pain can be very intense, and not only at the injection site, but throughout the arm, when the patient seems to feel the movement of the drug through the vascular network, and they say that “the vein is burning.” The pain can be short-lived, or it can remain for several days or even a week; this depends not only on the severity of the endothelial burn, but also on the patient’s personal characteristics regarding the perception of pain.
Pain during the passage of the medicine leads to spastic contraction of the vein, in response to which the small veins flowing into it expand, a mesh of dilated blue vessels against the background of skin that has turned pale due to spasm of the arterioles.
The inflamed vein can be palpated; it is dense like a cord due to local swelling of the tissue. When a blood clot appears in the lumen of the vessel, it can also be felt and seen with duplex ultrasound scanning.
Over time, the inflammation will pass, the thickening of the vessel may remain, and the skin over it may darken. The internal lumen of the vessel after several chemotherapy burns will decrease until it closes - obliteration. During the course of phlebitis, small vessels approaching the diseased vein - collaterals - will open and expand, but there will remain the possibility of slight swelling of the arm below the site of venous damage.
Why do varicose veins reappear?
Varicose veins are a chronic progressive pathology. Even the most modern treatment does not guarantee that new varicose veins will not appear again years later. In this case, why bother treating varicose veins at all? Does this make sense? When a person has caries and a tooth starts to hurt, for some reason no one doubts that it is necessary to visit the dentist and solve the problem. Without treatment, the pain will intensify, inflammation of the surrounding tissues will appear, which will lead to quite serious complications. Therefore, the patient makes an appointment with the doctor and receives appropriate treatment. However, no doctor can guarantee that caries will not appear on other teeth.
Varicose veins rarely manifest as pain; symptoms increase gradually, sometimes over a period of years. Many people get used to the presence of swelling, then get used to the fact that the skin has begun to darken. An ulcer appears, chronic visits to the surgeon at the clinic begin, and dressings begin with an unclear effect.
Trophic ulcer with untreated varicose veins
And the main problem, varicose veins, is treated at best with tablets and compression. In addition to problems associated with trophic disorders, there are thromboembolic complications, which can be even more dangerous. It’s strange, but thrombophlebitis that occurs against the background of varicose veins is perceived by some doctors in public medical institutions as something force majeure and little expected. The fact that the patient has not received adequate treatment for varicose veins for a number of years does not bother anyone.
Basic methods of treating veins
After introducing the cytostatic into the cells, all that remains is to wait for the completion of the side process and help recovery.
The pathophysiology of drug-induced toxic phlebitis has been little studied, no clinical studies have been conducted on the problem, all recommendations are based only on the personal experience of medical personnel. In each case and after each administration, it is necessary to consult with the attending physician who knows the specifics of the local interaction of the cytostatic and the range of local adverse reactions.
To relieve pain and reduce inflammation, NSAIDs are best suited - non-steroidal anti-inflammatory drugs, but the benefits of any one drug have not been proven; it is better to rely on the patient’s “everyday” preferences, because sensitivity to pain is different, and the analgesic effect is also individual.
If there is a high risk of pulmonary thromboembolism, the patient is prescribed a special “blood thinning” therapy, usually long-term - at least a week and with regular monitoring of coagulation.
You can use ointments with heparin to rub into the area of the damaged vessel. Hepatrombin™ gel consists of heparin and prednisolone, the latter has an anti-inflammatory effect, the drug is not officially certified for use in peripheral phlebitis and thrombophlebitis.
Troxevasin™ ointment has a good reputation , which simultaneously reduces inflammation and swelling of tissues, changing the rheological properties of blood towards dilution, but less than is typical for heparin. However, studies have shown that the drug is capable of dissolving microthrombi.
Indovazin™ gel is a mixture of troxerutin and the NSAID indomethacin, therefore it reduces the severity of pain and does everything that is inherent in Troxevasin™. It is not advisable to combine both ointments, since the spectrum of action of the combined drug is greater, but with Indovazin™ it is quite possible to alternate the application of Hepatrombin™. The absorption of ointments is microscopic; they do not replace NSAIDs and anticoagulants taken orally, but they help to endure the unpleasant consequences of treatment.
How veins are restored after IVs: useful procedures
They try to reduce local irritation of the mucous membrane lining the inner wall of the vein by large dilutions and slow administration in droppers, literally over hours. Not all cytostatics can withstand high dilution and long administration; some lose their properties, so they are administered as a bolus using a syringe. In this case, immediately after chemotherapy, the vein is “washed” with saline, trying to reduce its damage.
Be sure to check the patency of the vessel and the possibility of extravasation - the spread of cytostatics in the tissue during microscopic ruptures of the vascular wall - before administration and during the drip.
It is recommended not to administer chemotherapy to the same vein; it is better to alternate hands, giving the vessel more time to restore its mucous membrane. The prophylactic use of ointments with heparin or troxerutin before chemotherapy has no pathomorphological basis, that is, it is useless.
When planning multi-month chemotherapy, it is advisable to think about installing a venous port; its service life is at least five years. The device completely eliminates such a side effect as drug phlebitis, but only taking anticoagulants can save you from thrombosis.
Indeed, veins can appear even after removal, so why eliminate them?
In addition, existing varicose veins are not only the cause of various complications of varicose veins, but also a significant factor in the destruction of healthy veins.
You can wait until such huge veins appear
Venous vessels are a system of interconnected tubes filled with blood. When blood flow slows down and a pathological volume forms in a certain segment of the venous bed, nearby vessels are inevitably involved in the process. This is one of the mechanisms of progression of varicose veins.
Prevention of complications
Many cytostatics damage veins, the aggressive cisplatin, anthracyclines and vinca alkaloids, as well as the relatively “mild” gemcitabine with fluorouracil, are especially zealous in initiating chemical phlebitis. Based on their effect on tissue, anthracyclines with vinca alkaloids are classified as blister agents, cisplatin is only an irritant, and gemcitabine is definitely not a blister agent. Nevertheless, any chemotherapy drug, and even more so a combination of cytostatics, can damage a vein, therefore, during intravenous administration, personnel must strictly follow the instructions for the duration and method of injection.
Physiotherapeutic procedures and acupuncture, phototherapy and infrared irradiation, and magnetic field stimulation help recovery.
In our Clinic, each patient undergoes a specific program of support for chemotherapy and recovery after treatment, focused on the characteristics of the body and tissue resistance.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Russian clinical guidelines for the prevention and treatment of venous thromboembolic complications in cancer patients // M.: Planida; 2012
- Somonova O.V., Antukh E.A., Elizarova A.L., et al. /Practical recommendations for the prevention and treatment of thromboembolic complications in cancer patients // Malignant tumors: Practical recommendations RUSSCO #3s2; 2017 (vol. 7).
- Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines // Chest Am Coll Chest Phys.; 2012.
- Jones S., Holmes F., O'Shaughnessey J., et al. /Docetaxel with cyclophosphamide is associated with an overall survival benefit compared with doxorubicin and cyclophosphamide: 7-year follow-up of US Oncology Research trial 9735// JCO 2009; 27.
- International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology // Lymphology; Mar 2013; 46(1).
- Khorana AA, Kuderer NM, Culakova E., et al./ Development and validation of a predictive model for chemotherapy-associated thrombosis// Blood 2008; 15.