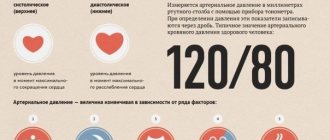
Blood pressure is an indicator related to constant changes. It changes at certain times of the day and increases after physical activity and stressful situations. Tonometer readings of 120/80 are considered normal values around the world, but they can deviate by several units in one direction or another, depending on age, lifestyle and the individual characteristics of the human body. What to do if the tonometer increasingly records pressure as 120/100? What causes this condition and whether it needs correction, we need to understand in more detail.
What pressure is considered normal?
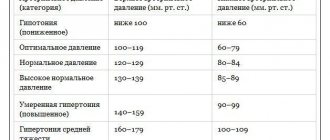
A person’s blood pressure has two indicators - the upper (systolic), recorded at the moment the heart contracts, and the lower (diastolic), noted when the heart relaxes and pushes blood into the arteries. When the heart and capillaries are functioning normally, the tonometer readings are within 120/80 or 110/70; a slight deviation up or down is not considered a pathology.
For each person, the pressure is individual, but, in addition to fixing the two indicators, it is necessary to monitor the difference between them. This difference is called pulse pressure and can also indicate existing health problems. Changes in tonometer readings are affected by:
- Times of Day;
- nervous tension, stress;
- physical exercise;
- binge eating;
- alcohol consumption;
- taking certain medications.
If, after an unexpected increase in blood pressure (BP) levels, the indicators stabilize on their own, and the fact of jumps is rarely observed, there is nothing to worry about. The normal difference between the upper and lower limits should be from 35 to 55 mmHg, and a regular decrease in this indicator indicates the development of cardiovascular pathology.
Complications
Complications with high lower blood pressure, 125 over 95 may be just the beginning, can be very serious. If the diastolic arterial value is high for a significant time, the process of sclerotic changes may begin:
- connective tissue grows;
- replaces organ cells;
- the functioning of the organ is impaired.
Such a process in the heart can lead to myocardiosclerosis. As the disease progresses, stagnation of blood circulation occurs, which leads to cardiovascular failure.
Problems of blood stagnation in the systemic circulation lead to:
- swelling;
- ascites.
Cardiovascular insufficiency in the small circle can cause:
- shortness of breath;
- pulmonary edema.
Complications can affect the brain:
- problems with intelligence;
- memory impairment.
A high lower value may contribute to the development of diseases. Problems with kidney function can develop into kidney failure.
It is necessary to distinguish the norm from the disease
If a person regularly sees a blood pressure of 120/100 during measurement, he should visit a cardiologist. Despite a slight deviation in the normal pulse pressure, this is a demonstration of the onset of pathological changes in the condition of the heart and blood vessels. A constant departure of the lower indicator beyond normal limits, while the upper one remains unchanged, indicates the possible presence of the following problems:
Why does blood pressure jump during menopause?
- sclerotic changes in the capillary system;
- diseases of the renal system;
- hormonal imbalances;
- diseases of the spinal column;
- elevated blood sugar levels;
- problems with the thyroid gland.
Blood pressure of 125/100 and even 130/100 should not frighten a person if it appears once after hard physical work, as a result of stress or mental overstrain. Therefore, in such a situation, it is important to separate a single jump in tonometer readings from the first signs of a developing disease. It is not possible to do this on your own; if your diastolic pressure constantly increases, you should consult a specialist and undergo an examination.
Does anything need to be done?
Having considered all possible variations on the theme of blood pressure 120 over 90, we can conclude that in the vast majority of cases such indicators do not pose any danger to humans. A slight upward deviation in diastolic pressure (albeit towards a borderline value) is not critical and, as a rule, does not cause discomfort.
If discomfort is still present, how should you feel about the pressure of 120 to 90, what to do with the “lower” value - lower it or increase it to the usual levels? Cardiologists advise not to rush and make do with symptomatic therapy.
- If you have a headache, then you can take any painkiller, for example, an analgesic or an analgesic + antispasmodic. Antispasmodics slightly dilate blood vessels, so a slight decrease in diastolic pressure can be expected.
- If you feel dizzy, then you need to lie down and rest, providing fresh air. Perhaps it was the disturbance of cerebral circulation that caused the disorder of the vestibular apparatus.
- If a hypertensive patient experiences pain in the chest, and the pressure continues to drop rapidly, then you should call a doctor without hesitation.
And if a hypotensive person’s blood pressure is already 120 over 95, what does this mean, what to do at home in this case? The main thing is not to panic; increasing diastolic pressure may indicate overwork or stress; try to calm down, take a comfortable position, and relax.
Manifestations of isolated hypertension are often accompanied by rapid heartbeat, so you can drink something sedative - valocordin, valerian (preferably in tablets) and try to rest. A short rest, as a rule, quickly returns blood pressure to normal.
Reasons for a sustained increase in diastole
What does pressure 120/100 mean if the lower reading is constantly elevated? Doctors warn about the danger of developing isolated diastolic hypertension when only the lower reading fluctuates. A similar diagnosis is made if the tonometer readings are constantly recorded: the upper one is below 140, and the lower one is above 90.
Previously, doctors believed that it was important to control only systolic pressure, and diastolic pressure was not so important, but later the importance of both marks was confirmed. Isolated diastolic hypertension often goes unnoticed, because a person does not feel the severe symptoms inherent in the disease. It is sometimes possible to detect jumps in the lower numbers only during routine examinations by a cardiologist.
A steady increase in the lower pressure threshold is noted for a number of reasons:
- kidney disease (most often chronic glomerulonephritis) - in this case, the vessels in the renal system undergo destructive changes. The veins and arteries located there narrow, causing an increase in lower pressure;
- malignant and benign neoplasms in the kidneys - they provoke a constant release of adrenaline into the blood plasma, which is why the diastolic indicator is always elevated;
- problems with the endocrine system - observed in women during menopause, pregnancy, as well as in patients with thyroid pathologies (hypothyroidism, hyperthyroidism, diffuse goiter);
- Essential hypertension is a condition in which an increase in diastolic pressure is provoked not by existing diseases, but by a general poor emotional or physical state of the body. Often, doctors cannot determine the true cause of blood pressure surges until they conduct a full examination of the body.
Why might a person still exhibit signs of isolated diastolic hypertension? Unfavorable factors affecting the condition of the heart and blood vessels include excess weight, poor diet, lack of a good night's rest, psycho-emotional and physical stress.
Unfortunately, if a person’s blood pressure becomes normal at 120/100, doctors may suspect the development of atherosclerosis.
Indicators 120/90 in a pregnant woman
Is it normal for blood pressure to be 120 over 90 during pregnancy? The optimal level of blood pressure during pregnancy is determined by gestational age. Thus, the first trimester is characterized by a decrease in tonometer values, which is due to changes in hormonal levels, and the second is characterized by an increase in parameters as a result of an increase in the volume of the cardiovascular system.
Blood pressure parameters of 120/90 in a pregnant woman are considered a variant of the norm, but it is necessary to take into account the woman’s “working” pressure before fertilization occurs. If a woman had a low blood pressure of 100/70 before pregnancy, then an increase in values to 125/90 can cause a deterioration in her health. However, such a ratio will be regarded by experts as a variant of the norm, since against the background of hormonal changes, an increase in pressure by 10-20 units is an irreversible process.
Important! Hypertension is diagnosed in a pregnant woman if the blood pressure level exceeds 130/95 mm. Hg Art.
Characteristic symptoms
Isolated diastolic hypertension - what it means has become clear. Now you need to understand the signs that may indicate existing problems. The insidiousness of the disease is that it is often asymptomatic, and not every person will measure pressure with a tonometer for no apparent reason.
You can guess about pathological changes in the body by the following symptoms:
- headaches that appear at the time of increase in diastolic pressure, not of a pronounced nature and accompanied by dizziness;
- signs from the visual system - flashing “flies” before the eyes, double objects, a foggy veil;
- shortness of breath that occurs regardless of physical activity;
- regular nosebleeds, indicating weak capillaries.
As a rule, there are no more pronounced signs when the lower pressure threshold increases, so many patients do not go to doctors, attributing the symptoms to fatigue, lack of sleep and stress. An important indicator in such a situation is the pulse. Normally, even with increased diastole, it should not be more than 90 beats per minute.
A pulse of 100 against a background of pressure of 120–130 per 100 indicates pathological changes in the functioning of the cardiovascular system. This condition is most dangerous for children, elderly patients and pregnant women. If you ignore the symptoms of increased diastolic pressure against the background of normal systolic pressure, the risk of dangerous consequences for the body increases.
These include thinning and loss of elasticity of the vascular walls, deterioration in the blood supply to tissues and vital organs, and pathological narrowing of the capillaries until they are completely blocked. The condition is also dangerous due to overstrain of the heart muscle due to the impossibility of its complete relaxation.
Possible symptoms
Isolated arterial diastolic hypertension is more often determined by chance, since it does not cause obvious symptoms. The main complaint of patients with this ratio is headache, which becomes constant. Headaches often occur when weather conditions change; depending on the intensity, they are accompanied by dizziness.
Patients also report pain and a feeling of heaviness in the chest area. These sensations lead to difficulty breathing, which causes rapid heartbeat and shortness of breath.
Diagnostics and methods of correction
What to do if you suspect isolated diastolic hypertension? First of all, visit a specialist and undergo an examination. It includes the following methods of studying the body:
- Ultrasound of the heart, kidneys and thyroid gland;
- Dopplerography of cerebral vessels;
- ECG;
- laboratory blood tests for biochemistry.
If the presence of tumors in the kidneys is suspected, magnetic resonance imaging is performed. To identify problems with the endocrine system, it is recommended to donate blood for hormones, this is especially important for women during pregnancy and menopause. The goal of treatment is not to correct the condition when low blood pressure regularly increases, but to eliminate the cause.
Usually, after the underlying disease is cured, be it a pathology of the thyroid gland or the renal system, the pressure stabilizes on its own. What can you do if your blood pressure increases again? It is not recommended to take antihypertensive drugs on your own, because in this case both the lower and upper levels will drop at the same time.
Only the doctor decides whether there is a need to take medications and how to combine drugs with each other in order to maintain both tonometer indicators normal.
Among the drugs intended for the correction of isolated diastolic hypertension are:
- Diuretics are necessary to remove excess fluid from the body and eliminate swelling, which are always present in the complex therapy of hypertension. These are Veroshpiron, Triamterene, Furosemide, Hypothiazide.
- Alpha blockers are well tolerated and help stabilize blood pressure. These include Terazosin and Prazosin.
- Beta-blockers - stabilize the functioning of the heart muscle, reducing the number of contractions and affecting the nerve centers. The heart begins to function in an economical mode, and the pressure is restored. This group includes Bisoprolol, Atenolol, Metoprolol.
- ACE inhibitors – inhibit the production of angiotensin, a substance that increases blood pressure. This group includes the drugs Captopril, Fosinopril, Enalapril and their derivatives.
- Calcium antagonists - expand the lumens of the capillaries, due to which the pressure stabilizes. Verapamil and Nifedipine tablets are effective.
Therapy also includes taking sedatives if pressure surges are provoked by nervous tension and stress. The patient is prescribed herbal remedies - tincture of peony, motherwort, valerian, drugs Glycine, Nervohel, Valocordin, Corvalol, Persen.
First aid measures
Before the medical team arrives, the patient needs to be seated comfortably, windows should be opened to allow oxygen in, and clothing should be loosened. You can give a sedative like Corvalol to stop an anxiety attack. Taking any pills on your own is not recommended so as not to aggravate the condition and cause side effects. After first aid has been provided and the patient has been examined by a doctor, the need for medication is assessed.
If a person has a blood pressure of 120–130 over 100, while feeling weak, nauseated, complaining of shortness of breath and severe headaches, you should immediately call a doctor
In the initial stages of isolated diastolic hypertension, when there are no signs of serious diseases in the body, the following treatment methods can be used:
- Diet with limited salty, smoked and spicy foods. Preference should be given to natural products, lean meat, fish, vegetables and fruits. You should avoid caffeine-containing drinks, fast carbohydrates, and foods high in animal fats.
- Moderate physical activity. Morning jogging, yoga, swimming, and walking will help relieve signs of hypertension. Even walking in the fresh air every night helps stabilize blood pressure.
- Limiting stress. We must try to eliminate all factors that cause a regular release of adrenaline into the blood and an increase in tonometer readings. If the problem lies in psychosomatics (when psychological problems are expressed in physiological diseases), it is worth visiting a psychologist.
- Rejection of bad habits. Addiction to smoking and alcoholic beverages has been proven by scientists to affect blood pressure levels and contribute to destructive changes in the functioning of the heart and blood vessels.
- Body weight control. Overstrain of the capillaries and heart muscle is often provoked by extra pounds. Doctors never tire of repeating that every hypertensive patient should lose weight by following a diet and providing the body with regular physical activity to stabilize blood pressure.
Also, to restore normal blood pressure levels, you should get enough sleep and avoid mental and physical exhaustion. Night rest should be at least 7 hours in a row. For symptoms of diastolic hypertension, the patient should regularly take measurements using a tonometer. An increase in lower pressure for no apparent reason is a reason to undergo examination by a cardiologist, identify the causes of the disease and begin appropriate therapy.
While it is possible to do without the use of medications, a person is advised to change their lifestyle, give up bad habits, go on a diet and keep their weight under control. If the diastolic reading regularly increases, over time this can lead to chronic hypertension, when there is a need for lifelong use of antihypertensive drugs, and the risk of dangerous complications also increases.