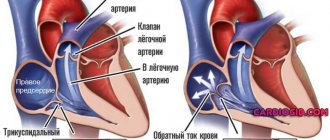
The human heart consists of several (four) chambers (two ventricles and two atria). In order for the blood to move progressively in one direction, there are valves between them that prevent reverse flow. On the right is the tricuspid valve, and on the left is the bicuspid, or mitral, valve. The latter consists of anterior and posterior rather soft valves, the opening and closing of which is regulated by the papillary muscles. They are connected to each other by means of rigid, inextensible chords.
There are two types of changes in the structure of the mitral valve: stenosis and insufficiency. In this case, its function is disrupted. In the first case, an unnecessary obstacle to the blood flow is created, and in the second, a significant portion of it returns back to the atria. Prolapse is a fairly common change in the leaflets, accompanied by mitral valve insufficiency.
Why does it occur
Mitral valve prolapse of the 1st degree usually occurs with various connective tissue pathologies. In this case, its valves become pliable and bend into the atrium cavity during ventricular contraction. Thus, part of the blood gets back, due to which the ejection fraction decreases. The degree of insufficiency is determined by measuring the volume of regurgitation, and prolapse by the distance of deviation of the leaflets. At the first degree, the valves deviate by 3-6 mm.
This defect is found much more often in children, especially girls. In this case, we are talking about a congenital pathology that causes an imperfect structure of connective tissue. In this case, the basis of the valve flaps changes, as well as the chords responsible for the rigidity of the structure.
MVP is more often detected in children during a routine medical examination
Among the acquired causes of mitral valve prolapse (MVP) grade 1 are:
- Rheumatic lesions that develop as an autoimmune reaction to certain types of streptococcus. In this case, damage to other valves and joints is also typical.
- Coronary heart disease affecting the papillary muscles and chords, which can even rupture during myocardial infarction.
- Traumatic injuries usually lead to more severe symptoms.
Symptoms of the disease
In most cases, stage 1 of the disease does not have clearly defined symptoms. Some patients may experience signs of heart failure.
If the sick person does not have this ailment, such symptoms may occur due to impaired functioning of the right cardiac ventricle. Regurgitation of the 1st degree as an independent pathology does not cause significant disturbances in the human circulatory system.
If a person has stage 2 or 3 of the disease, then a large amount of blood entering the right heart ventricle can lead to organ failure.
This is due to the expansion of the chambers and thickening of the walls of the heart muscle.
Despite the hidden heart defect at the first stage, some patients experience the following symptoms:
- severe shortness of breath;
- blue discoloration of the skin;
- mild hypertension;
- swelling;
- weakness;
- dizziness.
In cases where this pulmonary artery defect is congenital, the disease manifests itself in the first few months of the child’s life. Most sick children have severe symptoms due to the severe form of the disease.
If a newborn suffers from grade 4 regurgitation, then the disease cannot be corrected, in which case death is possible.
It is for this reason that both adults and children should annually undergo appropriate procedures and tests that will help identify the disease at an early stage.
Signs
Symptoms of first-degree mitral prolapse are usually less severe, and in some situations may be completely absent. Most often, this condition manifests itself as pain in the left half of the chest, not associated with myocardial ischemia. It can last for several minutes, or it can persist throughout the day. There is no connection with physical activity, but sometimes the pain syndrome is provoked by emotional experiences.
Other manifestations are:
- feeling of lack of air and inability to breathe deeply;
- heart rhythm disturbances (rapid or slow heartbeat, interruptions and extrasystole);
- frequent headaches accompanied by dizziness;
- loss of consciousness for no apparent reason;
- a slight increase in systemic temperature in the absence of infectious diseases.
Since MVP is quite often combined with vegetative-vascular dystonia, its symptoms may also occur.
Diagnostics
To suspect first-degree mitral valve prolapse, it is enough to ask the patient about his complaints and listen to the heartbeat with a stethoscope. But since blood regurgitation is not pronounced, this sign (heart murmur) may be absent, so it is necessary to resort to more accurate examination methods.
ECHO-cardiography most clearly allows one to judge the condition and operation of the valves. With an additional Doppler study, it is possible to estimate what volume of blood and at what speed returns to the atrium during systole (contraction of the ventricles). The ECG is of an auxiliary nature, since it does not fully reflect the changes accompanying MVP.
ECHO-cardiography is the most accurate diagnostic method for mitral valve prolapse
Short description
As you know, the main job of the heart muscle is to continuously transport blood throughout the human body and saturate it with oxygen.
In the heart itself, blood moves in a certain order from one section to another, after which it continues its movement through the veins in the systemic circulation.
With regurgitation, a reverse movement of blood occurs in various volumes, and the severity of symptoms depends on the indicators of the latter.
Regurgitation is a pathological process indicating improper functioning of the heart muscle due to a serious disease. This condition has 5 stages of development. Each of them needs to be considered:
- Regurgitation 1st degree. It is this stage that is called mild and at this moment is of greater interest. The pathological process occurring in the heart during the first stage can be described as follows: blood entering the cardiac ventricle flows out of it into the atrium through the valve leaflets.
- Grade 2 regurgitation cannot be ignored and must be treated. The flow of blood flow from the valves exceeds 25 mm.
- Regurgitation of the 3rd degree is diagnosed if the blood stream exceeds 2 cm. This phenomenon should in no case be ignored, the patient is registered.
- Stage 4 disease - blood flow exceeds 2.5 cm.
- Grade 5 is considered a physiological feature of a person. That is, if the pathology does not develop, it does not pose a threat to human life.
Treatment methods
Treatment of grade 1 mitral valve prolapse is not required in some cases. This applies to identifying such changes during ultrasound in a child who does not experience any symptoms of the disease. At the same time, children have no restrictions for physical education, but it is not advisable to engage in professional sports.
If there are symptoms of the disease, then it is necessary to select therapy to reduce or eliminate them. In each case, the doctor prescribes therapy, taking into account individual characteristics. The main groups of drugs used in the treatment of MVP include:
- sedatives (calming), which are used when disorders of the autonomic nervous system occur;
- beta blockers are indicated for tachycardia and extrasystole;
- products that improve myocardial nutrition (panangin, magnerot, riboxin) contain electrolytes necessary for the functioning of the heart;
- Anticoagulants are prescribed quite rarely, only for concomitant thrombosis.
It is very important to optimize your lifestyle, because the symptoms are often aggravated by chronic fatigue and nervous tension. Necessary:
- observe the rest and work regime;
- maintain motor activity at an acceptable level (as far as general condition allows);
- periodically go to specialized sanatoriums, where they conduct restorative courses of massage, acupuncture, mud therapy, etc.
In some cases, herbal medicine is recommended, which includes the use of infusions from various mixtures containing motherwort, hawthorn, sage, and St. John's wort.
Surgical intervention for the first degree of mitral valve prolapse is not indicated.
Diagnosis and treatment of pulmonary arterial hypertension in children
Increased pressure in the pulmonary circulation in children is a common occurrence and is observed in many diseases of the cardiovascular system.
The first pathological description of pulmonary hypertension (PH) dates back to 1865, when the German researcher Julius Klob reported autopsy findings of severe narrowing of the small branches of the pulmonary artery in a patient who had progressive edema, shortness of breath and cyanosis [1]. In 1891, the pathomorphological picture of pulmonary arterial hypertension (PAH) of unknown etiology with severe hypertrophy of the right ventricle of the heart was described by Ernst von Romberg [2]. In 1897, Victor Eisenmenger presented a patient who had suffered from dyspnea and cyanosis since childhood. She subsequently suffered a fatal pulmonary hemorrhage. An autopsy revealed a large ventricular septal defect. Ten years later, in 1901, the Argentine physician Abel Ayerza reported a case of sclerosis of the pulmonary arteries, accompanied by cyanosis, shortness of breath, and polycythemia. His two students F. Arrillaga and P. Escudero subsequently named this syndrome Aerza disease [3].
Thus, for about a century and a half, the problem of PH has not lost its relevance and has attracted the attention of the wider medical community.
Classification and diagnostic criteria for pulmonary hypertension
World symposia on the problem of PH are convened every 5 years. The last 5th, held in 2013 in Nice, France, turned out to be a record number of participants - more than 1000 doctors, researchers, pharmacists, and drug manufacturers. It was decided to maintain the general philosophy developed earlier in 1998, 2003 and 2008 in Evian, Venice and Dana Point for the systematization of LH.
According to the modern classification, there are 5 groups of variants of pulmonary hypertension in accordance with clinical, pathophysiological and therapeutic features [4]:
I. Pulmonary arterial hypertension
1.1. Idiopathic (primary) 1.2. Hereditary
1.2.1. BMPR2 gene 1.2.2. ALK1 gene, endoglin (with or without hereditary hemorrhagic telangiectasia) 1.2.3. Unknown etiology
1.3. Associated with medicinal and toxic effects 1.4. Associated with:
1.4.1. Systemic connective tissue diseases 1.4.2. HIV infection 1.4.3. Portal hypertension 1.4.4. Congenital heart defects (systemic-pulmonary shunts) 1.4.5. Schistosomiasis 1.4.6. Chronic hemolytic anemia
1.5. Persistent pulmonary hypertension of newborns
I. Pulmonary veno-occlusive disease and/or pulmonary capillary hemangiomatosis
II. Pulmonary hypertension associated with left heart disease
2.1. Systolic dysfunction 2.2. Diastolic dysfunction 2.3. Lesions of the valvular apparatus of the heart
III. Pulmonary hypertension associated with pathology of the respiratory system and/or hypoxia
3.1. Chronic obstructive pulmonary diseases 3.2. Interstitial lung diseases 3.3. Pulmonary pathology with mixed obstructive-restrictive disorders 3.4. Breathing disorders during sleep 3.5. Alveolar hypoventilation 3.6. High altitude pulmonary hypertension 3.7. Developmental defects
IV. Pulmonary hypertension due to chronic thrombotic and/or embolic diseases
V. Mixed forms
5.1. Hematological diseases: myeloproliferative diseases, splenectomy 5.2. Systemic diseases: sarcoidosis, pulmonary Langerhans cell histiocytosis, lymphangiomatosis, neurofibromatosis, vasculitis 5.3. Metabolic disorders: with impaired glycogen metabolism, Gaucher's disease, pathology of the thyroid gland 5.4. Others: tumor obstruction, fibrosing mediastinitis, chronic renal failure
According to the presented classification, variants of “classical” PH, implying primary and/or primary involvement of the pulmonary arterial bed, are combined into group I under the name “pulmonary arterial hypertension”.
All forms of PH included in the classification have been described in children. However, the most common are PAH due to heart defects and idiopathic pulmonary hypertension.
The criterion for diagnosing PAH in both adults and children is an increase in pulmonary artery pressure > 25 mmHg. Art. at rest with normal pulmonary capillary wedge pressure ≤ 15 mm Hg. Art.
At the same time, attempts are being made to develop terminology, diagnostic criteria and classification of PH in relation to pediatrics.
Considering that systemic arterial pressure (BP) in a child is lower than in an adult, it is proposed to diagnose PH in children when the ratio of systolic pressure in the pulmonary artery/systolic systemic BP increases more than 0.4 [5].
The working group of the Institute for the Study of Pulmonary Vascular Diseases in 2011 in Panama proposed the terminology and classification of PH, and most precisely hypertensive pulmonary vascular disease in children [7]. According to their recommendations, a mandatory criterion for hypertensive pulmonary vascular disease in children is an increase in pulmonary vascular resistance of more than 3 units. Wood × m2. This is due to the fact that in some cases, for example, with left-right systemic-pulmonary shunts, the increase in pressure in the pulmonary artery is not accompanied by an increase in pulmonary vascular resistance, and these children require prompt surgical correction of the defect rather than drug treatment. The Panamanian systematization is the first classification applicable exclusively to pediatrics. It divides pulmonary hypertensive vascular diseases into 10 categories.
Classification of hypertensive vascular pulmonary disease in children
- Prenatal hypertensive pulmonary vascular disease.
- Perinatal maladaptation of pulmonary vessels (persistent pulmonary hypertension of newborns).
- Cardiovascular diseases.
- Bronchopulmonary dysplasia.
- Isolated hypertensive pulmonary vascular disease (isolated pulmonary arterial hypertension).
- Multifactorial hypertensive pulmonary vascular disease associated with congenital defects/syndromes.
- Lung diseases.
- Thromboembolism of pulmonary vessels.
- Hypobaric hypoxia.
- Hypertensive vascular pulmonary disease associated with diseases of other organs and systems.
Thus, pulmonary arterial hypertension, corresponding to the 1st section of the Dana Point classification, can be found in the 2nd, 3rd, 5th and 10th points of the Panama classification.
Apparently, it is necessary, by combining the efforts of experts, to take the best of the two classifications and, on their basis, to create a systematization of PH that is convenient for clinicians.
The tactics for diagnosing and treating PH uses the terms of evidence-based medicine, such as the class of recommendations and the level of evidence, and also takes into account the functional class of disease severity (Table 1–2).
To characterize the severity of PH, the functional classification of the New York Heart Association is used (Table 3) [7].
In 2011, in Panama, members of the working group of the Institute for the Study of Pulmonary Vascular Diseases proposed a functional classification of PH in children separately for ages up to 6 months, 6 months - 1 year, 1–2 years, 2–5 years, 5–16 years [6] . Considering that medications approved in Russia for the treatment of PH in children are prescribed from 3 years of age, in Table. Figure 4 shows the functional classes of PH severity in children 2–5 and 5–16 years old. Since, in general, the age differences presented are not significant, we considered it possible to combine these age groups.
Clinical picture of pulmonary hypertension
The clinical picture of PAH in children is poor and nonspecific. The main complaint is usually shortness of breath. At first, shortness of breath is detected only during physical exertion, then, as the disease progresses, it appears at rest, sometimes accompanied by attacks of suffocation. The higher the pressure in the pulmonary artery, the more pronounced the shortness of breath [7]. During a clinical examination of children with idiopathic PH, attention is drawn to the pallor of the skin with bright coloring of the cheeks, earlobes, fingertips, and the “raspberry” tint of the mucous membranes of the lips.
Syncope in patients with idiopathic pulmonary arterial hypertension is recorded in 30% of cases and is a serious complication of the disease, indicating an unfavorable prognosis. When syncope occurs, the patient automatically moves to IV, the most severe functional class of pulmonary hypertension, reflecting its important prognostic value.
Attacks of chest pain are possible, which are associated with right ventricular ischemia.
In children, noticeable increased pulsation in the second intercostal space on the left and in the epigastric region, caused by hypertrophy of the right ventricle.
On auscultation, the second tone above the pulmonary artery is sharply intensified, accentuated, and sometimes acquires a metallic tint. Characteristic is the presence of a third tone, heard to the right of the sternum, which intensifies with the appearance of right ventricular failure. A systolic murmur of pulmonary ejection along the left edge of the sternum, a diastolic murmur in the 2nd intercostal space on the left due to pulmonary valve insufficiency (Graham-Still murmur), a systolic murmur of relative tricuspid valve insufficiency in the 5–6 intercostal spaces to the left of the sternum and on the xiphoid may be heard. process, intensifying with inspiration (Rivero-Corvallo symptom).
When signs of right ventricular failure occur, peripheral edema, hepatomegaly, and peripheral cyanosis appear. Due to compression of the laryngeal nerve by the dilated pulmonary artery, hoarseness (Ortner's sign) may occur.
Diagnosis of pulmonary hypertension
The earlier PH is diagnosed and treatment begins, the greater the chance of preventing vascular remodeling and stopping the progression of the disease.
During the examination, it is very important to detect possible primary causes of pulmonary hypertension - heart defects, systemic connective tissue diseases, thromboembolic disorders, portal hypertension, HIV, etc.
We recommend screening of such children.
In the diagnosis of PH, Doppler echocardiography, right ventricular catheterization, electrocardiography (ECG), determination of blood gas composition, radiography, determination of respiratory function, ventilation-perfusion lung scintigraphy, computed tomography, and magnetic resonance imaging are used.
However, to establish a diagnosis of pulmonary hypertension, only those examination methods that allow one to determine the pressure in the pulmonary artery are key. PH can be preliminarily diagnosed using a non-invasive method such as Doppler echocardiography, but the most accurate method, the so-called “gold standard” for diagnosing PH, is invasive measurement of pressure in the right side of the heart through catheterization [4, 8].
We have developed an algorithm for diagnosing pulmonary hypertension in children, based on an initial echocardiographic study in children with symptoms of PH or at risk.
Examination of a patient with suspected PH includes a number of studies to confirm the diagnosis, determine the clinical group of PH and specify the nosology within this group. PAH and especially idiopathic PH are diagnoses of exclusion.
An echocardiographic diagnosis of PH is unlikely if tricuspid regurgitation velocity is less than 2.8 m/s and pulmonary artery systolic pressure is less than 36 mmHg. Art., with no additional signs of PH. If additional echocardiographic criteria are present, the diagnosis of PH is possible. A diagnosis of PH is also possible if the tricuspid regurgitation velocity is more than 2.9 m/s and the systolic pressure in the pulmonary artery is more than 37 mmHg. Art. If the speed of tricuspid regurgitation is more than 3.4 m/s and the systolic pressure in the pulmonary artery is more than 50 mm Hg. Art., the diagnosis of PH is very likely.
Additional echocardiographic criteria for PH include: an increase in the rate of regurgitation on the pulmonary valve, a shortening of the acceleration time of flow in the pulmonary artery, an increase in the size of the right chambers of the heart, disruption of the shape and function of the interventricular septum, right ventricular hypertrophy, dilatation of the pulmonary artery.
Determination of blood oxygen saturation is important for the differential diagnosis of PH.
A decrease in blood oxygen saturation is observed with right-to-left shunting, as well as with pulmonary hypertension combined with respiratory failure (chronic obstructive pulmonary diseases, massive pulmonary embolism).
Pulmonary function testing can identify obstructive or restrictive disorders.
Ventilation-perfusion lung scintigraphy is a reliable method for the differential diagnosis of chronic thromboembolism and idiopathic pulmonary hypertension.
Modern research methods such as computed tomography and magnetic resonance imaging also play an important role in the diagnosis and differential diagnosis of PH. They make it possible to see the size of cavities, blood vessels, the condition of the walls of the heart, septal defects, blood clots, and tumors.
Read the end of the article in the next issue.
L. I. Agapitov, Doctor of Medical Sciences
A separate structural unit of the Research Clinical Institute of Pediatrics, State Budgetary Educational Institution of Higher Professional Education, Russian National Research Medical University named after. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
Contact Information
Prevention and prognosis
Prevention can be carried out only in case of a secondary defect, while timely treatment of the foci in which the chronic infection is localized, as well as the fight against hypercholesterolemia, is necessary. With primary valve changes and an asymptomatic course of the disease, the prognosis is favorable and you can lead a normal life. It is also not contraindicated to carry a child and give birth on your own. At the same time, it is worth performing an ultrasound of the heart annually in order to identify possible changes in time.
Mitral valve prolapse is the sagging of its walls into the atrium during contraction of the ventricles. In this case, a reverse flow of blood occurs, the volume of which determines the severity of the deficiency. The first degree is the most initial and in most cases is asymptomatic, but is often accompanied by a disorder of the autonomic nervous system. With grade 1 MVP, symptomatic treatment can be carried out, but the most important thing is to follow a daily routine, perform moderate exercise, and then the heart defect may never manifest itself.