Several years ago, diabetes was one of the indicators for termination of pregnancy. But medicine is developing, and the disease during pregnancy can be controlled.
Now gynecologists successfully manage pregnancy in patients with this diagnosis, and hospitals have special equipment that allows children to be delivered in emergency cases. There are pocket glucose meters for determining blood sugar levels and effective medications.
But the expectant mother must be under the supervision of a doctor throughout the entire period.
Definition, forms of the disease
Diabetes mellitus is an endocrine disease. It occurs due to a lack of insulin, a pancreatic hormone, in the blood. This substance is responsible for ensuring that glucose enters all cells of the human body.
Diabetes has several forms:
- Insulin dependence is an autoimmune disease. It occurs due to a lack of insulin in the body due to disruption of the pancreas. This form cannot be treated.
- Insulin-independent – older people are susceptible; the disease progresses due to the fact that cells lose sensitivity to insulin. For therapy you need to take medications and maintain a diet.
Reasons for development:
- excess body weight;
- heredity;
- metabolic disease;
- use of certain medications (steroid hormones, diuretics;
- atherosclerosis;
- vascular diseases;
- disruption of the pancreas;
- adrenal insufficiency;
- elderly age;
- neuroses, constant stress.
Negative consequences during pregnancy:
- death of the fetus in the womb;
- polyhydramnios;
- intrauterine development disorder;
- problems with uterine tone;
- late gestosis;
- jaundice in a baby;
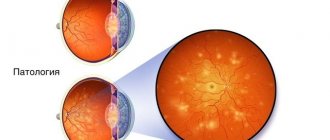
- blurred vision;
- premature aging of the placenta;
- premature birth.
Additional tests
Glucose is a source of energy and growth for the fetus. When it enters the body of the future newborn in excess, problems begin. In each trimester, a pregnant woman should undergo tests such as:
- examination by a nephrologist, ultrasound of the genitourinary system;
- general and detailed blood test, fasting glucose level should be up to 6.1 mmol/l. After eating 2 hours - no more than 7.4 mmol/l. If the rate is above 7%, conception is not recommended at all.
- urine test, 2-3 times a month;
- biochemistry;
- coagulogram;
- leukocyte count;
- fluorography;
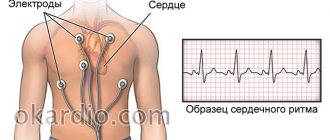
- ECG;
- take a stool test.
Carrying a child with diabetes
When a woman knows about the disease, then pregnancy should be carefully planned together with the gynecologist. If this is not done, then there is a high risk of the child developing intrauterine pathologies.
You also need to undergo diagnostics; it includes several stages:
- Blood test for diabetes. Normally 3.3-5.5 m/mol, values above this are already a deviation;
- For ten days, you need to regularly check your insulin levels using a pocket glucometer;
- Daily blood pressure monitoring;
- Urine test for kidney disease;
- ECG for women in labor over 35 years of age or at risk;
- Testing for sensitivity of limbs;
- Consultation with an endocrinologist.
During the entire gestation period, the woman in labor should be under the supervision of a doctor and listen to her own well-being.
Pregnancy planning, management, planned hospitalizations
If a woman nevertheless decides to carry and give birth to a child, the very first thing to do is to notify the specialists caring for the patient: a gynecologist, an immunologist, an endocrinologist. It is also necessary to take tests for 3 months before planning a pregnancy. With stable glucose levels, you can begin to conceive.
3 hospitalizations, routine examinations, and additional tests are prescribed. First, the woman is sent to the clinic in the first trimester. Hospitalization is needed to correct blood counts and identify possible deviations from the norm.
The second occurs at 18-20 weeks. This time, gynecologists examine the development of the fetus and correct metabolic processes in the mother’s body.
The third time hospitalization is needed at 35 weeks. A pregnant woman is being prepared for the upcoming birth.
Features and nuances during pregnancy
A woman should psychologically prepare for the fact that carrying a child with diabetes will require many restrictions, hospital visits and constant monitoring. At the beginning of the period, the patient’s tolerance to carbohydrates should improve and therefore the amount of insulin consumed is reduced.
Already in the middle of pregnancy, it will return to its original level, because the placenta actively begins to function and produces counter-insular hormones - prolactin and glycogen.
The dangerous period is the fourth gestational month. At this time, the baby’s pancreas is already functioning and responding to maternal blood. If the amount of sugar is increased, the fetal pancreas injects insulin, which causes glucose to break down and be converted into fat. As a result, the child rapidly gains weight.
During pregnancy, a woman spends some time in a hospital setting:
- for the first time in the period from 8-10 weeks, for examination and identification of contraindications;
- then 5-6 gestational months, the child’s condition and possible pathologies are assessed;
- at 8 months to determine the type of delivery: cesarean section or natural way.
Pregnancy progresses differently, depending on the form of diabetes. Insulin dependent is more common. Women with this diagnosis need to take insulin for nine months; the exact dosage will be prescribed by an endocrinologist. Usually the following scheme is supported:
- at the beginning of gestation, the amount of the hormone is reduced by 25-30%;
- second trimester - on the contrary, increase the daily dose, it is approximately 80-100 units;
- before childbirth it is lowered again.
The non-insulin-dependent form of the disease in women giving birth practically does not occur. This is due to the fact that such diabetes develops after 40 years, and conception at this age occurs very rarely.
Another type of pathology that develops exclusively during pregnancy is gestational diabetes mellitus. After childbirth it completely disappears. It usually develops at the end of the term and the causes of its occurrence still remain unexplored. Doctors are more inclined to believe that it appears due to the heavy load on the pancreas.
Symptoms of complications:
- constant hunger;
- acute desire to drink;
- swelling;
- frequent urination;
- increase in blood sugar.
To diagnose this type of pathology, it is necessary to pass a glucose tolerance test. The referral is issued by the attending physician. Often the patient does not suspect that she has a latent form of diabetes, and the symptoms are usually attributed to simple malaise during pregnancy.
Therefore, you need to know what contributes to pathology:
- overweight;
- polycystic ovary syndrome;
- gestational diabetes in previous pregnancies;
- the presence of sugar in urine before conception and at the beginning of pregnancy.
Diabetes diagnosed in time can be corrected.
Diabetes and pregnancy: interview with the director of MONIIAG
The traditions of the MONIIAG school are based on:
– on a combination of knowledge and experience accumulated over two centuries (the history of the institution begins in the 19th century), as well as the latest achievements of modern medicine and high technology;
– on the use of the most advanced and effective methods of diagnosis and treatment in obstetrics and gynecology;
– on caring for a woman and a child, responsible and careful management of any pregnancy, and especially one occurring against the background of various somatic diseases;
– on an individual approach to pregnancy management and a comprehensive assessment of the risks of developing various complications for the mother and fetus, complications of surgical treatment of gynecological diseases, as well as their prevention through preparation for childbirth and operations.
– on collegial decision-making in the interaction of a whole team of competent specialists, each of whom takes into account all the characteristics of the body to achieve the best results.
MONIIAG is a leading system-forming scientific and practical institution of health care and obstetric services in the Moscow region. We are doing everything possible to increase the birth rate, preserve the health of the population and introduce advanced achievements of world medicine into healthcare practice in the Russian Federation. During the calendar year, more than 50,000 women are consulted in the outpatient department of MONIIAG. Over the course of a year, the research institute gives birth to 2,700–2,800 new residents of the Moscow region, 800–900 of whom are born to women at extreme risk.
The main function of the institute is to organize and provide high-quality medical care to the female population of the Moscow region. This is a cause that each of our employees serves responsibly and conscientiously. Therefore, the quality of the medical services we provide meets high international standards.
The life and health of a woman and child, and therefore their well-being and happiness, are our main values. We use all the possibilities of modern reproductology in order to achieve the most important thing - the birth of a new life and preservation of health.
The importance of the institute as a regional center for women's health is highly appreciated by government authorities and the civil community of the Moscow region.
The priority areas of work of the institute and its clinics are:
– preparation and management of pregnancy if a woman has severe diseases of the heart, kidneys, lungs, endocrine organs, central and peripheral nervous system, visual organs, etc., as well as reducing their negative impact on the body of the mother, fetus and newborn;
– provision of medical assistance to infertile couples and management of pregnancy after assisted reproductive technologies until its completion;
– surgical preparation for pregnancy of women with an operated cervix;
– comprehensive examination of pregnant women in order to identify and clarify the presence of congenital malformations in the fetus, including invasive diagnostic procedures (chorionic villus biopsy, cordocentesis, etc.);
– gynecological operations in women with extreme obesity, urinary incontinence, endometriosis with damage to adjacent pelvic organs (bladder, ureters, intestines), severe extragenital diseases;
– prevention of cervical cancer, early diagnosis and treatment of cervical precancer and other HPV-associated diseases in women at different age periods of life;
– preservation of a woman’s reproductive health during the period from menarche to menopause;
– expert-level ultrasound examinations in obstetrics and gynecology.
MONIIAG offers a unique range of medical services and has everything necessary to solve complex surgical problems: highly qualified specialists, laboratories and operating rooms equipped with modern equipment.
Our leading specialists are the best of the best in their field, they know and love their work. These are doctors of the first and highest categories, candidates and doctors of medical sciences, professors, members of the Russian Academy of Sciences, laureates of state awards of the Russian Federation.
Every year the institute performs up to 3,000 gynecological operations. Of these, at least 900 are classified as extreme-risk surgical interventions due to the danger of anesthesia, the complexity of the intervention itself, and the need for operations on adjacent organs. High-tech care combined with the work of professional surgeons has allowed the institute to have no postoperative mortality for more than 10 years.
Acquired with the assistance of the Governor of the Moscow Region A.Yu. Vorobyova in 2012, the Da Vinci robotic surgical unit allows for high-tech operations to restore reproductive function in young women. The installation makes it possible to perform unique operations during pregnancy and at the same time maintain pregnancy. Surgical interventions performed on this installation are characterized by low trauma, which also makes it possible to provide surgical care to women of almost any age.
The medical, scientific, pedagogical and organizational-methodological activities of the institute’s staff had a significant impact on improving such demographic indicators in the Moscow region as maternal, infant and perinatal mortality: maternal mortality decreased by 2.6 times (from 20.4 to 7.8 per 100 thousand live births) infant – 2.7 times (from 18.9 to 6.9 per 1000 live births); perinatal – 2.4 times (from 19.8 to 8.2 per 1000 births). At the same time, the perinatal mortality of newborns at the institute does not exceed 3.5% (in 2021 it was 1.2%), which corresponds to the performance indicators of the best foreign obstetric clinics. There has been no maternal mortality at the institute over the past 15 years.
MONIIAG carries out scientific, teaching, organizational and methodological activities on an ongoing basis. We are ready for dialogue with specialists, including at the conferences and seminars we hold. We do not rest on our laurels and constantly improve our professionalism. We also invite colleagues to discuss practical and scientific issues on the pages of the journal “Russian Bulletin of Obstetrician-Gynecologist”.
We are ready to accept those who wish to study at our institute. Currently, more than 50 people are undergoing internship, residency and postgraduate studies at MONIIAG.
On the institute’s website, patients can find information on how to receive medical care at the institution, get acquainted with the main activities of the institution, and ask questions about their problem to our employees. Specialists in the field of obstetrics and gynecology will be able to familiarize themselves with the regulatory framework, the main activities of the research institute, and receive information about ongoing events and training opportunities.
Our patients are people who choose professionalism and quality. To solve your problems - for this we do everything possible and impossible, only the impossible requires more desire, effort, experience and skill. And the best reward for us is the happy smiles of our patients!
I wish you health, joy and prosperity! Director of MONIIAG, Doctor of Medical Sciences, Professor V.A. Petrukhin
Treatment of diabetes during gestation
Treatment for diabetes while pregnant includes taking insulin and a certain diet. The medicine and dosage will be prescribed by the attending physician.
Nutrition rules:
- reduce the amount of carbohydrates consumed, and proteins need to be increased;
- you need to eat at least 2000-2200 kilocalories per day, if you are overweight - 1600-1990 kilocalories;
- sweets are prohibited;
- fractional meals, approximately 8 times a day;
- It is necessary to consume vitamins A, B, C, D.
Additionally, you need to drink special herbal teas: from blueberry leaves, flax seeds, green beans. If there are no contraindications, then it is necessary to engage in physical exercise. They perfectly tone the body, improve well-being and prepare the ligaments for childbirth.
Childbirth with diabetes
At the end of the term, a month before the expected date of birth, the woman undergoes a final examination in the hospital to determine the type of delivery. If you are allowed to give birth on your own naturally, they usually follow the same pattern:
- The doctor punctures the amniotic sac.
- Oxytocin, insulin and, if necessary, pain medication are administered.
- The fetus is monitored using CHT, the doctor monitors the level of insulin in the mother's blood.
Each case is considered individually.
Fetal development
The main and crucial period is the beginning of fetal development. In the first trimester, most vital organs are formed. The child is not yet formed, so it actively feeds at the expense of the mother. An increase in blood glucose levels is fraught with the development of hyperglycemia in the unborn baby. Also, the organs of the nervous and cardiovascular systems are no less susceptible to pathologies.
From the 12th week of pregnancy, the condition of mother and child becomes better. The fetus develops its own pancreas, which produces insulin independently. It is important to carry out the necessary tests to monitor blood glucose levels and prevent unwanted complications.
The worst thing that can happen is termination of pregnancy, miscarriage, bleeding. The development of abnormalities in the development of the fetus (cleft lip, absence of organs) also dangerous To maintain the health of the baby and mother, it is necessary to take pregnancy and its planning seriously. Take tests according to the doctors’ schedule, do not neglect the recommendations. With diabetes, it is difficult to bear a healthy baby, but with desire and effort, it is possible. The main thing in this period is blood glucose control. Complications from the disease can be avoided.
Consequences and complications of the disease
Diabetes mellitus sometimes still has a detrimental effect on a pregnant woman, it all depends on the form of the disease and stage:
- early miscarriages;
- development of gestosis;
- severe and prolonged toxicosis;
- can cause polyhydramnios, which affects the intrauterine development of the child.
Diabetes mellitus is a serious pathology. Pregnancy with this disease is possible, but requires special monitoring and observation. A woman, having learned about an interesting situation, should immediately seek advice and follow the doctor’s instructions.
Recommended Diet
Even a healthy woman is required to follow a proper diet. For pregnant women who suffer from diabetes, the food entering the body is especially important. The content of sucrose in it is excluded, as before. Also, the expectant mother should control her carbohydrate intake and count calories. The disease weakens a woman’s body, and the process of glucose absorption may be further disrupted.
Eliminate from your diet:
- fruit juices;
- fast food;
- dates;
- pasta;
- fried potatoes;
- bananas;
- artificial drinks (exclude all carbonated drinks);
- milk, etc.