Pregnant women and their families usually expect one answer from an ultrasound examination - what is the sex of the child. For an obstetrician-gynecologist, a research method is necessary to promptly identify impaired blood flow during pregnancy and abnormal fetal development.
The management plan and delivery tactics depend on this. To understand the mechanisms of the disorder, it is necessary to consider the capabilities of the circulatory system between mother and child.
Structure of the uteroplacental blood flow
Mother and child are connected not only by the placenta, but also by a complex system of blood vessels. Therefore, all joint blood circulation is usually divided into levels that cannot exist in isolation, but work only in combination.
- The central part of the system is the placenta. It ensures the “absorption” of products from the maternal blood through the villi that have grown deep into the wall of the uterus. At the same time, the blood of mother and child does not mix. Several rows of special cells form a hematoplacental barrier, which is a serious obstacle to substances unnecessary for the fetus. Through it, the waste blood returns to the mother's venous system.
- The second part of the blood flow consists of the branches of the uterine arteries. If before pregnancy in the female body they are in a collapsed state and are called spiral, then from the period of 1 month they lose the muscle layer that can cause spasm. And by four months, the arteries transform into full-fledged trunks, filled with blood and heading to the placenta area. It is this mechanism, useful for feeding the fetus, that can turn out to be fatal during uterine bleeding: the walls of the vessels can no longer contract.
- The vessels in the umbilical cord form the third pathway of blood flow. There are 2 arteries and a vein here. They connect the baby with the placenta and form the fetal-placental circle. Reduced blood flow at this level causes the most severe damage to the fetus.
How is placental circulation disrupted?
Poor blood flow associated with the placenta is called placental insufficiency. It can occur at any stage of pregnancy in two forms.
Acute appears suddenly, even during childbirth, and does not depend on the duration of pregnancy. The fetus falls into a state of hypoxia (oxygen deficiency), which threatens its death.
The main pathological mechanisms of this condition:
- premature placental abruption;
- heart attack due to thrombosis.
Chronic often complicates the course of pregnancy after 13 weeks. Symptoms appear in the third trimester. The mechanism of formation is early aging of the placenta due to the deposition of fibrin on the villi.
As a result of changes in the structure of chorionic villi (placental tissue), the functioning of the hematoplacental barrier ceases, metabolic processes between the maternal body and the fetus are disrupted
Negative consequences in such conditions, depending on the degree of violation, can lead to inevitable death of the fetus.
Kasabulatov N.M.
It is currently known that the most common cause of disturbances in the condition of the fetus during pregnancy is placental insufficiency (PI), which is the main cause of intrauterine hypoxia, delayed growth and development of the fetus, and its injuries during childbirth [4,14,8].
Placental dysfunction can occur under the influence of various damaging factors - endocrine, hypoxic, toxic, infectious; due to obstetric and extragenital pathology of the mother, environmental and pharmacological influences during pregnancy [1].
In clinical practice, primary and secondary PN are distinguished
Primary PN is characterized by changes in the structure, location, attachment of the placenta and maturation of chorionic villi. Secondary PN is characterized by involutional-dystrophic and inflammatory changes in the placenta, developing in the II–III trimesters of pregnancy.
PN can have both an acute and chronic course. Acute PN is determined by disturbances of the uteroplacental circulation. It often develops against the background of extensive infarctions and premature abruption of a normally located placenta, resulting in fetal death and termination of pregnancy. Chronic PN occurs as a result of a violation of compensatory-adaptive mechanisms in combination with circulatory disorders and involutionary-dystrophic processes [13,15].
PN is also divided into relative (compensated) and absolute (decompensated). Compensated PN does not require treatment, and pregnancy in these cases can result in timely birth of a viable and healthy child. Failure of one of the links in the physiological adaptation of the maternal body to pregnancy can manifest itself as hypertensive disorders, acute (placental abruption) or chronic PN, intrauterine fetal growth restriction (IUGR). The nature of the adaptive-homeostatic reactions of the placenta depends on the cause of PN and differs in extragenital and obstetric complications [13]. Absolute placental insufficiency occurs in severe form and is accompanied by IUGR and fetal hypoxia (up to its intrauterine death). Pregnancy in such women often occurs against the background of the threat of miscarriage.
There are two main forms of chronic placental insufficiency
1) a violation of nutritional function (trophic insufficiency), in which the absorption and assimilation of nutritious products, as well as the synthesis of the fetus’s own metabolic products, are impaired;
2) respiratory failure due to impaired transport of oxygen and carbon dioxide. Both forms of PN can exist independently or in combination. In the pathogenesis of PN, disorders of the uteroplacental and fetal placental circulation, metabolism, synthetic function and state of the cell membranes of the placenta are distinguished. With pathology of the uteroplacental circulation, there is a disturbance in the flow of blood into the intervillous space, difficulty in the outflow of blood from it and a change in the rheological and coagulation properties of the uterine blood. The most important pathophysiological changes in the body during chronic PN in a pregnant woman include hypovolemia and decreased organ perfusion. At the same time, the sensitivity of vascular elements to circulating pressor agents increases and the coagulation cascade is activated, which leads to a simultaneous decrease in the perfusion of the intervillous space [13,15,17,19].
Reocoagulation disorders play an important role in disrupting the hemodynamics of the placenta. Hypercoagulation occupies a special place in the pathogenesis of PN. The initial physiological hypercoagulation of the blood, which reaches its maximum development by the end of the third trimester, provides local hemostasis in the uterus after childbirth. During pregnancy, the body develops hypervolemia and decreases peripheral vascular resistance. These mechanisms are adaptive and protective in nature in healthy pregnant women. In the case of pathology leading to activation of the hemostatic system, they lose their protective function and contribute to the worsening of PN [17,19]. During pregnancy complicated by intrauterine growth retardation, the number of trophoblastic elements penetrating the myometrium decreases. Incomplete trophoblast invasion into the maternal spinal arteries causes insufficient trophoblast perfusion and changes in the secretion of humoral factors. The development of modern methods for studying the state of the fetoplacental complex in the dynamics of pregnancy and childbirth allows for timely diagnosis and treatment of the main clinical forms of fetal suffering - intrauterine growth retardation (hypotrophy) and/or its chronic hypoxia.
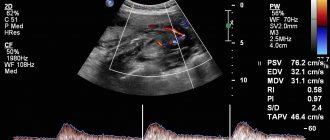
Prenatal diagnosis of these conditions is established on the basis of echography and fetometry of the placenta, cardiotocography, Doppler flowmetry in the vessels of the “mother-placenta-fetus” system, cytology, amnioscopy, hormonal methods (determination of free estriol, human chorionic gonadotropin, placental lactogen). Postpartum diagnosis of the placenta is carried out mainly using morphometric and morphological methods. The Doppler ultrasound method, which uses direct measurements of blood flow in various vascular zones of the mother-placenta-fetus system in dynamics, allows one to assess the state of uteroplacental blood flow and therefore has important diagnostic and prognostic significance in the group of pregnant women at high perinatal risk. A directly proportional relationship with a high correlation coefficient was noted between the degree of hemodynamic disturbances in the mother-placenta-fetus system and the incidence of fetal growth retardation, intrauterine hypoxia, surgical delivery by cesarean section, severe condition of the newborn and perinatal losses. The final diagnosis is established taking into account the complementary data of a comprehensive study: echography, CTG and Doppler measurements [9].
Prevention and treatment of PN and intrauterine growth retardation
include measures aimed at improving uteroplacental blood circulation and microcirculation, normalizing gas exchange in the mother-fetus system, improving the metabolic function of the placenta, and restoring impaired function of cell membranes.
In recent years, the arsenal of drugs used for PN has expanded significantly. The effect of the drugs used is realized mainly at the level of the microvasculature of the placenta. In this case, agents are conventionally identified that act on the vascular component of the blood flow and on the rheological properties and anticoagulant potential of the blood. Medicines that affect the vascular component of the uteroplacental vascular system include adrenergic agonists. Their effect is due to a decrease in the tone and amplitude of uterine contractions, general peripheral vascular resistance, diastolic blood pressure, and an increase in heart rate without a significant decrease in blood pressure (BP). Under their influence, pulse blood pressure and cardiac output significantly increase, and hemoperfusion of the uterus and feto-placental area increases. This group includes fenoterol, terbutaline, hexopenaline. With high activity of the uterine muscles and acute fetal hypoxia, intravenous administration of adrenergic agonists to the mother helps improve uteroplacental blood flow. The best effect from their use is achieved with a “fluid load” and cardiotonic agents. This treatment method is complemented by metabolic therapy, laser exposure, etc. [5,10,11,12]. To improve oxygen transport to the fetus, vasodilators and drugs that normalize microcirculation processes in the placenta and uterus (theophylline, xanthinol nicotinate) can be used. In recent years, drugs such as Actovegin, Instenon, and Troxerutin have found widespread use in the treatment of placental insufficiency. These drugs act on the pathogenetic links in the development of placental insufficiency , being involved in metabolic processes, participating in the regulation of energy supply, correcting the impaired compensatory capabilities of the mother and fetus [15].
To improve uteroplacental circulation, intravenous infusions of rheopolyglucin, dextrans, as well as drugs that improve the rheological properties of blood (heparin, fraxiparin) are also used. In recent years, efferent treatment methods (plasmapheresis) have begun to be used to treat PN. It is recommended to use ultraviolet blood irradiation, medical ozone, and laser therapy. Prevention and treatment of this pathology are most promising in early manifestations of PN. Improvement of ultrasound diagnostic equipment makes it possible to identify early, preclinical stages of placental dysfunction. Currently, the emphasis of perinatal care is shifting towards preventing the development of placental insufficiency. Therefore, it is especially important to find safe and effective means of preventing this pathology in women with complicated pregnancy. Treatment of pregnant women at high risk of PN is justified. First of all, these are pregnant women with intrauterine infection, gestosis, and autoimmune pathology. According to the literature, the most effective method for treating the initial manifestations of PN is the use of the cellular metabolism activator Actovegin a in combination with ß-mimetics [18]. Actovegin activates tissue metabolism, which improves trophism, and stimulates the regeneration process. The active substance is a deproteinized hemoderivative from calf blood with low molecular weight peptides and nucleic acid derivatives. Actovegin improves cellular metabolism by increasing the transport and accumulation of glucose and oxygen, enhancing intracellular utilization. These processes lead to an acceleration of ATP metabolism and an increase in the energy resources of the cell. Under conditions that limit the normal functions of energy metabolism (hypoxia, lack of substrate), and with increased energy consumption (healing, regeneration), Actovegin stimulates the energy processes of functional metabolism and anabolism. The secondary effect is increased blood supply. In cases of metabolic and blood supply disorders to the brain, for example, in cerebral insufficiency syndrome (dementia), the transport of glucose across the BBB and its utilization by cells deteriorate. The activity of pyruvate dehydrogenase and the concentration of acetylcholine also decrease. The use of Actovegin improves the transport and utilization of glucose, while an increase in oxygen consumption is observed. Under the influence of Actovegin infusions, central hemodynamic parameters significantly improve in pregnant women who had a hypokinetic type of blood circulation. At the same time, the total peripheral vascular resistance is significantly reduced and fetal-placental blood flow improves [6]. The use of Actovegin significantly improves the indicators of arterial and venous blood flow in the mother-placenta-fetus system, which makes it possible to reduce the frequency of early delivery in PN and adverse perinatal outcomes [2]. Infusion therapy with Actovegin has a pronounced therapeutic effect on the condition of the fetus developing under conditions of placental insufficiency, which is expressed in a significant improvement in blood flow in the fetal-placental vessels and the dynamics of its intrauterine growth. In addition, treatment with Actovegin promotes better tolerance of labor to the fetus. The positive effect of Actovegin on fetal-placental circulation is associated primarily with improved oxygen delivery, increased glucose perfusion and restoration of aerobic metabolism in the placenta [6]. Complex treatment of PN developing in the third trimester with Actovegin and Ginipral allows one to achieve satisfactory perinatal outcomes, despite concomitant extragenital pathology in the mother [3]. Falyants A.G., Zakharov I.V. [16] treated PN in 53 pregnant women with uterine fibroids. A complex of drugs was proposed that improved uteroplacental blood flow, each of which normalized individual parts of the impaired placental circulation and, in general, created a system for protecting the condition of the fetus. Treatment was carried out at gestational ages of 22–26 weeks and at 32–36 weeks. The complex included dipyridamole (tablet) - 25 mg 3 times a day. pentoxifylline 400 mg 1 dr. 2 times a day and Actovegin (tablet) – 0.2 g 3 times a day. In case of decompensation of PN, infusions of Actovegin and rheopolyglucin with pentoxifylline were carried out. Significant positive changes were obtained during control CTG and ultrasound examinations. There were no perinatal losses. Demidovich E.O., Ignatko I.V. [7] used Actovegin in the form of tablets 200 mg three times a day for three weeks to correct identified hemodynamic disorders in fetuses with growth retardation syndrome. For pregnant women with PN on the background of extragenital pathology, long-term gestosis, long-term threat of miscarriage and stage II fetal growth restriction syndrome, this drug was prescribed intravenously in the form of a 10% solution with sodium chloride (250 ml for a course of 7–10 procedures). The recommended regimen for using Actovegin for therapeutic purposes includes starting its use with intravenous drip administration of the drug every other day 5 times at a dose of 5 ml in 250 ml of 5% glucose or saline solution. Then continue taking the drug orally, 1 tablet 3 times a day for 3–4 weeks. In patients with recurrent miscarriage, prophylactic use of Actovegin is also possible. In this case, you can limit yourself to oral administration of the drug, 1 tablet 3 times a day for 2–3 weeks. Thus, Actovegin is one of the promising drugs, the use of which can achieve good results in the treatment and prevention of placental insufficiency. However, the problem of treating PN remains not fully resolved and requires further research in this direction.
Literature
1. Aylamazyan E.K. antioxidants in the complex therapy of late toxicosis and associated chronic fetal hypoxia // Obstetrics and Gynecology. 1991, No. 3, pp. 30–34.
2. Afanasyeva N.V., Strizhakov A.N. outcomes of pregnancy and childbirth with fetoplacental insufficiency of varying severity.// Issues of gynecology, obstetrics and perinatology. 2004, T. 3, No. 2, pp. 7–13.
3. Vozovik A.V. Correction of fetoplacental insufficiency in pregnant women with non-toxic nodular goiter. //Materials of the V Russian Forum “Mother and Child”, Moscow, 2003, 44–45.
4. Garmasheva N.L., Konstantinova N.N. Pathophysiological basis for the protection of human intrauterine development. L., 1985., 159 p.
5. Grishchenko V.I., Shcherbina N.A. Improving the diagnosis and therapy of perinatal pathology // Obstetrics and Gynecology. 1990, No. 10, pp. 3–6.
6. Gromyko G.L. Actovegin: Experience of use in obstetric practice./Edited by Ailamazyan E.K./St. Petersburg, 2000, 33–41.
7. Demidovich E.O., Ignatko I.V. Features of fetal renal blood flow in fetoplacental insufficiency. //Materials of the V Russian Forum “Mother and Child”, Moscow, 2003, pp. 56–57.
8. Kosheleva N.G., Arzhanova O.N., Gromyko G.L. et al. New approaches to the treatment of threatened premature birth // Bulletin of the Russian Association of Obstetricians and Gynecologists. 1996, No. 1, pp. 55–60.
9. Medvedev M.V. Clinical guidelines for ultrasound. 1996, Volume II.
10. Ordzhonikidze N.V., Klimenko P.A., Dzhivigelova G.D. et al. New in the treatment of pregnant women with fetal growth retardation syndrome // Obstetrics and Gynecology. 1996, no. 3, pp. 32–36.
11. Parashchuk Yu. S., Grishchenko O. V., Lakhno I. V., Shevchenko O. I. Fetoplacental insufficiency. Tutorial. Kharkov: KhSMU, 1999. 45 p.
12. Pestrikova T. Yu., Chizhova T. V., Petrichko M. I., etc. Management of high-risk pregnancy and childbirth. M.: Souvenir, 1994. 287 p.
13. Radzinsky V.E., Ordiyants I.M. Placental insufficiency in gestosis. // Obstetrics and gynecology, 1999; No. 1, pp. 11–6.
14. Savelyeva G.M., Fedorova M.V., Klimenko P.A. et al. Placental insufficiency. M, 1991, 276 p.
15. Sidelnikova V.M. Current problems of miscarriage. M., 1999, 138 p.
16. Falyants A.G., Zakharov I.V. Correction of placental insufficiency in pregnant women with uterine fibroids. //Materials of the V Russian Forum “Mother and Child”, Moscow, 2003, pp. 244–246.
17. Fedorova M.V. Placental insufficiency. // Obstetrics and gynecology, 1997; 6:40–3. 18. Shapovalenko S.A. Complex diagnosis and treatment of placental insufficiency in pregnant women at different stages of gestation. // Bulletin of the Russian Association of Obstetricians and Gynecologists, 2001, No. 2, pp. 43–7.
19. Salafia CM Placental pathology of fetal growth restriction. // Clin. Obstet. Gynecol, 1997; 40: 740–9.
Causes of blood flow disorders during pregnancy
Various reasons can cause disruption of uteroplacental blood flow. These include common maternal diseases:
- pathology of the neuroendocrine system (diabetes mellitus, diseases of the thyroid gland and adrenal glands, changes in the hypothalamus region of the brain stem);
- lung diseases (emphysema, bronchial asthma);
- disorders in the cardiovascular system caused by developmental defects, the consequences of hypertension, a tendency to hypotension;
- renal pathology (chronic nephritis, pyelonephritis, especially in the stage of renal failure;
- anemia (anemia) associated with deficiency of iron and vitamins;
- conditions accompanied by increased blood clotting contribute to increased thrombus formation in the vessels of the placenta;
- acute and exacerbation of chronic infectious processes cause corresponding inflammation in the placenta, vascular edema and reduction in blood flow; in the first trimester this can result in miscarriage.
Pathology of the uterus creates local conditions for inadequate blood flow:
- any changes in the layers of the uterus (myometrium, endometrium);
- malformations (for example, “bicornuate”, “saddle-shaped” uterus);
- underdevelopment (hypoplasia);
- tumor formations from muscle tissue (fibroids), especially in a primiparous woman over the age of 35; at a younger age, small fibroids help compensate for blood flow.
The causes of insufficient blood flow include unfavorable conditions during pregnancy in the following cases:
- multiple births;
- Rhesus conflict;
- preeclampsia;
- breech presentation of the fetus;
- pathological placenta previa.
The risk of impaired blood flow occurs when:
- previous abortions;
- maternal smoking, alcoholism and drug addiction;
- constant nervous environment associated with social or everyday unsettlement;
- violation of proper nutrition of a woman.
Causes
Poor blood flow in the uterus during pregnancy can develop in women with anemia. When the level of hemoglobin decreases, the blood circulation process accelerates so that the tissues receive the necessary amount of oxygen. This reaction is called compensatory and can occur in the uteroplacental system.
Blood flow during pregnancy is impaired, perhaps due to placenta previa and or its low attachment. In this case, the blood circulation process slows down, since the muscle layer of the lower segment of the uterus is much thinner. This condition can occur in women who have previously had a caesarean section delivery and the placenta has implanted in the area of the scar.
Impaired blood flow in the uterine artery during pregnancy can occur against the background of late toxicosis, since such a complication leads to damage to small vessels. Also, the circulatory process is often disrupted in the presence of an infectious disease that was suffered during pregnancy.
If there is a conflict between the Rh factor or blood group, hemolytic disease of the fetus may develop in difficult situations. This leads to anemia in the unborn child, and accordingly, blood flow is disrupted. When a woman’s blood pressure is unstable, the speed of transportation of biological fluid through the veins and arteries changes.
Impaired blood flow in the left uterine artery during pregnancy can develop if a woman has malformations of the reproductive organ. A bicornuate uterus is especially dangerous, since with such a structure there is a septum in its cavity that divides the organ in half. In this case, fetal development occurs in one part of the uterus, since the two arteries are not connected to each other and the network cannot expand, the circulatory process is disrupted.
This pathological condition can develop against the background of endometrial diseases. This often occurs in women who have undergone diagnostic curettage, had abortions, or have suffered from inflammatory diseases. Impaired blood flow in the right uterine artery during pregnancy can be caused by uterine fibroids or diabetes mellitus.
Types of chronic placental insufficiency
Depending on the development of consequences for the fetus and the ability of the mother’s body to adapt, 4 forms or stages of chronic placental insufficiency are distinguished:
- compensation - the mother’s body fully protects the fetus by improving blood flow through other pathways, and the child does not feel a lack of oxygen, develops normally, is born on time and develops well;
- subcompensation - the mother is not able to fully compensate for the lack of nutrition, and the fetus lags behind in development, there is a risk of complications and congenital defects;
- decompensation - accompanied by a complete disruption of the adaptation mechanisms, normal pregnancy is impossible, the fetus develops serious defects that are incompatible with viability, and death in utero is very likely;
- critical - due to severe changes in the structure of the placenta, further gestation of the fetus is impossible, inevitable death occurs, any treatment is ineffective.
What degrees of blood flow disturbance does placental insufficiency cause?
A comparison of clinical manifestations and ultrasound examination results made it possible to distinguish 3 degrees of blood flow disturbance between mother and fetus.
The first is characterized by minimal changes at the uteroplacental level, provides a “reserve” of time of about a month for treatment and full recovery without consequences, there are 2 types:
- Ia - only the uteroplacental blood flow is reduced, with the fetal-placental blood flow unchanged. It manifests itself as a delay in fetal development in 90% of cases.
- Ib - fetal-placental circulation suffers, but the uteroplacental circulation remains normal. Delayed formation and development of the fetus suffers somewhat less (in 80% of cases).
The conclusion is issued after examining all components of the fetal blood flow
The second is that the disorder occurs both at the level of the uterine and umbilical vessels; hypoxia can be fatal to the fetus.
Third, blood circulation indicators are at a critical level, and it is even possible that the direction of blood flow is reversed (reverse).
For clinicians, such a classification provides an opportunity to accurately determine the level of disorders and choose the most appropriate treatment tactics.
Complications
Violation of uterine blood flow during pregnancy is a very serious pathological condition. If it is present, specialists often diagnose fetal growth retardation syndrome, which manifests itself in the insufficient weight of the child. If the electrolyte composition of the blood is disturbed, the occurrence of tachycardia, bradycardia and arrhythmia cannot be ruled out.
When the blood circulation process is disturbed, the fetus develops hypoxia. Source: beremennostnedeli.ru
The acidity level of the biological fluid may also change, the hormonal levels will not correspond to the norms, and the amount of fat depots decreases sharply. All this, in most cases, can provoke spontaneous abortion, and in a severe situation, intrauterine fetal death cannot be ruled out.
Symptoms of impaired blood flow
If the impaired blood flow is compensated, then the woman does not feel any abnormalities, but learns about them only after the examination.
Pronounced manifestations occur in acute form and chronic decompensation:
- the motor activity of the fetus increases sharply or completely disappears (at 28 weeks, normal development is accompanied by ten movements per day), this symptom requires immediate contact with an obstetrician-gynecologist;
- a slow increase in abdominal circumference, detected during monthly examination and measurement in the antenatal clinic (associated with excessive formation or lack of amniotic fluid);
- late toxicosis;
- high blood pressure;
- large weight gain;
- swelling in the legs;
- the appearance of protein in the urine.
The most dangerous thing is bleeding from the vagina. This sign can be regarded as beginning placental abruption. You must not delay in providing medical care.
What does the mother feel and what does the doctor determine during the examination?
Hypoxia stimulates fetal motor activity.
At an appointment with an obstetrician-gynecologist, the doctor listens to the fetal heartbeat and pays attention to high frequency, arrhythmia or bradycardia. This necessitates referral for Doppler examination.
A pregnant woman pays attention to increased movements, tremors
Diagnostics
The most complete picture of blood circulation between the uterus and the fetus is obtained through Doppler ultrasound, which is performed on all women three times during pregnancy.
The technique allows:
- measure blood flow by the speed of movement of the formed elements;
- determine its direction in arteries and veins;
- record changes before clinical manifestations.
The effect is based on the properties of ultrasonic wave reflection and is completely safe for the child and mother.
All changes are recorded on the monitor, measured with special sensors, and can be photographed in the required format.
By comparison with normal indicators, a conclusion is made about the degree of pathology. Violations can be detected at any level, in the vessels:
- umbilical cord,
- uterus,
- fetus
The doctor has time to prescribe treatment and check it at the next examination.
A type of Doppler ultrasound is Doppler ultrasound. It is prescribed for:
- maternal concomitant pathology;
- suspected premature aging and disruption of the placental barrier;
- signs of high or low water;
- preliminary data on intrauterine growth retardation, the formation of congenital malformations of the fetus;
- presence of genetic diseases in the family;
- clinical symptoms of fetal hypoxia.
The examination can reveal:
- thinning of the placenta;
- increase in growth area;
- intrauterine infection.
The method of long-term inpatient monitoring of the degree of fetal hypoxia allows you to see the results of using medications
Treatment of pathology
The possibility of maintaining pregnancy with the help of conservative treatment remains with the degree of impaired blood flow Ia and b. The second degree is considered borderline, the third requires urgent surgical delivery.
Treatment takes into account the pathogenesis of disorders. To achieve results it is necessary to influence all links:
- In case of mild disturbance of microcirculation, Chofitol (with a mineral-herbal composition) is prescribed, in more severe cases - Actovegin, Petoxifilin.
- If a mother’s tendency to form blood clots and disrupt the aggregation properties of blood is detected, then drugs such as Curantil, Trental are indicated. They can improve blood flow through the vessels.
- If low blood pressure is detected, Venofundin, Stabizol, ReoHES are used.
- Vasodilators - No-spa, Eufillin in injections - eliminate spastic contraction of blood vessels.
- It is recommended to reduce the tone of the uterus with the help of Magnesia, the drug Magne B6, this acts as an antihypoxic way to improve blood flow.
- A group of vitamins with antioxidant action eliminates negative consequences (vitamin E, ascorbic acid).
Medications are prescribed by a doctor. If necessary, the woman is offered hospitalization. This allows:
- provide bed rest;
- Constantly monitor the progress of pregnancy.
If there is an effect of conservative treatment, the woman independently carries to term and gives birth to a child. If there are no results, doctors may decide to perform an early cesarean section. In the third stage, only surgical delivery is indicated.
Therapy
If the fetus does not receive enough blood, it will develop hypoxia. When such a condition is detected, gynecologists must respond immediately and offer the girl the most appropriate treatment regimen, which will be based on simultaneous action on several stages of pathogenesis.
Initially, medications are selected that have the ability to improve the process of blood microcirculation, for example, it could be Actovegin or Pentoxifylline. Particular attention is paid to maintaining good blood flow in the vessels and stabilizing blood pressure.
For this purpose, medications based on hydroxyethyl starch are prescribed, including: Stabizol, Infucol, Voluven, ReoHES, Venofundin. These drugs act as an osmotic solution of starches, due to which the liquid does not leave the lumen of the blood vessels. It is best to take them during gestosis, since this way you can avoid the occurrence of edema and stabilize blood flow.
To relieve arterial spasm, medications with a vasodilating effect are prescribed. Eufillin, No-shpa or Magnesia are often prescribed (the drugs are best used in injection form). Hypoxia can also be prevented or eliminated by eliminating uterine tone. To do this, a woman will have to take Magnesia, Ginipral or vitamin B6.
It is not enough to eliminate hypoxia, it is also necessary to prevent the likelihood of complications, so Tocopherol, Ascorbic acid and Chophytol are introduced into the therapeutic complex. Some patients are injected intravenously with a 5% concentration of glucose solution, which makes it possible to remove toxins from the body.
To improve the condition of the placenta and saturate it with phospholipids, Essentiale is prescribed. To improve cellular nutrition, Cocarboxylase is prescribed, and if pregnancy occurs in a woman who has a history of uterine fibroids, taking Curantil will be useful.
When carrying a child, a woman must be prescribed a study of uteroplacental blood flow using Doppler ultrasound. As medical practice shows, it is this diagnostic method that makes it possible to identify all deviations, even minor ones; accordingly, doctors have the opportunity to start therapy in a timely manner and stabilize the condition of the pregnant woman.
What to do to prevent blood flow disorders?
Gynecologists urge women at risk to prepare themselves for pregnancy in advance and prevent unplanned conception.
Choosing the right body position while sleeping helps fetal blood flow
If you are already pregnant, it is recommended:
- avoid emotional and physical overload;
- eliminate bad habits;
- organize nutritious meals for the pregnant woman;
- monitor daily walks and stay in a ventilated room;
- do special gymnastics for pregnant women, yoga exercises;
- control body weight, carry out monthly weighing and measurement of abdominal circumference;
- It is considered more beneficial to sleep on the left side; this position reduces pressure on the inferior vena cava, which runs to the right of the uterus, but in some cases, with stagnation in the kidneys, sleeping on the right side improves the outflow from these important organs.
Modern diagnostic methods and approaches to the management of pregnant women make it possible to prevent severe disorders. However, many possibilities depend on the woman herself and her desire to have a healthy heir.