Few people know what systolic and diastolic blood pressure are and how important it is for both of these indicators to remain normal. Blood pressure is measured using the Korotkoff method. Tonometers today work precisely on this principle. After measuring blood pressure, doctors receive two numbers showing the systolic as well as the diastolic index.
The norm of such indicators may vary, depending on many factors, age, gender of the person, as well as the presence of concomitant diseases. A large difference between systolic and diastolic pressure is considered normal, but a small difference between these indicators can mean health problems.
The word systolic comes from the medical term systole, which refers to a short period of heartbeat. This level is considered the upper level and characterizes the force of pressure in the arteries during cardiac contraction. At the same time, the ventricles of the heart are compressed, as a result of which blood is pushed into the arteries and vessels, which is why such pressure occurs.
This indicator directly depends on the activity of the heart muscle and its condition, as well as on the speed with which cardiac contraction occurs and the strength of this process. Doctors believe that upper blood pressure is high when the heart beats rapidly, which is why systolic pressure is also called cardiac pressure. However, this statement is erroneous, because in the process of forming this indicator, large vessels and arteries are involved, serving as a kind of buffer.
Blood is released into the circulatory system during one systole, reaches the arteries and vessels in a short period, and they are able to provide resistance, on which the upper pressure indicator depends. The stronger the resistance provided by the arteries, the higher the tonometer needle will be when measuring the systolic indicator.
The normal systolic blood pressure reading is 120 mm Hg. pillar
Such indicators can be calculated based on a person’s age, as well as some individual characteristics. Sometimes doctors record a patient’s upper pressure level in the area of 130-140 mmHg. pillar and this may also be a variant of the norm. If this figure is even higher, we are talking about hypertension.
Causes of increased systolic pressure:
- diseases of the cardiovascular department of the body;
- thickening of vascular walls;
- menopause;
- decreased hemoglobin in the blood (anemia);
- kidney pathologies;
- excessive activity of the kidneys and thyroid gland in producing hormones;
- disruption of the aortic valve;
- age-related changes in the walls of large arteries.
There should be a large gap between the systolic and diastolic arterial index; if there is a small difference between these indicators, this is a reason to immediately consult a doctor.
Diastolic pressure is called lower, this medical term comes from the word diastole, the decoding of which means cardiac relaxation following systole. The formation of the lower numbers occurs due to the contraction of peripheral arteries that carry blood to the organs and tissues of the whole body. The state of the vascular system plays a significant role in diastolic pressure. If the tone of the vessels is low, their elasticity is insufficient, then the lower values will be far from normal.
At the end of the heartbeat, the aortic valve closes, preventing blood from flowing back. During this period, the heart is filled with new blood, enriched with nutrients and oxygen for the next contraction. At this time, blood moves freely through the arteries. In addition, the lower pressure index is influenced by the total blood volume in the circulatory system and heart rate. A large gap between systolic and diastolic blood pressure indicates normal processes in the cardiovascular system.
Why does discomfort occur?
The fact is that blood circulates in the human body all the time, even when the person is absolutely not susceptible. While blood enters the ventricles of the heart, the heart muscle spasms, and the blood in the ventricles under pressure comes out into the vessels. The process of filling the vessels occurs so quickly that pressure is created.
As soon as a failure occurs in this mechanism, a person begins to feel a deterioration in his general condition.
We can conclude that blood pressure depends on how intensely the heart contracts. As soon as you see that your blood pressure has deviated from the norm, you should immediately consult a doctor. It is possible that this is due to heart disease. If no heart problems are found, it is worth looking for a problem in other areas of the cardiovascular system.
Blood pressure, which is recorded at the moment the heart muscle pushes blood out of the heart, is called symbolic or upper pressure.
what is the difference between high and low blood pressure
Using systolic pressure, you can accurately determine the heart rate. Normally it is about 110-130.
As a person ages, a person's blood pressure increases. After 50 years, a blood pressure of 140 is considered normal.
But the pressure on the walls of the arteries at the moment of complete relaxation of the heart muscle is called diastolic or lower pressure.
From this indicator one can judge the force with which blood moves through the vessels of the body. If a person is absolutely healthy, then the indicator can be 65-80.
As you noticed, the difference between blood pressure and heart pressure
65 and 80 is significant. It is determined by the individual characteristics of each individual person. If your vessels are in good tone and elastic enough, then the pressure will be about 75-80 units.
What is blood pressure?
Tonometers record the blood pressure on the walls of the arteries, which is why it is called arterial pressure. In other words, the indicator means how much the level of fluid pressure in the circulatory system is higher than atmospheric pressure.
If we describe the whole process in simple words, it will look like this:
- The heart muscle contracts;
- The aortic valve closes;
- The heart receives highly oxygenated blood from the lungs;
- The following reduction occurs;
- Blood moves to all organs.
The entire circulatory system is involved in the formation of blood pressure, including the blood itself, which supplies tissues with oxygen, removes waste products, and provides thermoregulation. BP shows how well these functions are performed.
What is the normal difference between systolic and diastolic pressure?
Let's find out what difference in pressure is considered normal
. If we take the norm, which for an adult is 120/80 mm. rt. Art. , then it is easy to calculate the difference, which is 40 units.
But, if this difference becomes more than 65, this is a signal about the possibility of the rapid development of cardiovascular diseases. In addition, incorrect functioning of the heart and blood vessels leads to their early staining and, accordingly, acceleration of the aging process.
A difference of more than 45 or less than 35 units may indicate the appearance of pathological processes in the body. Symptoms may not appear with such a difference; sometimes general weakness and drowsiness occur.
If we talk about older people, then a difference of up to 50 units between systolic and diastolic pressure is considered the age norm. After all, their tissues are worn out enough and have lost the elasticity of blood vessels.
Norm of upper and lower blood pressure
Constant fixation of indicators within 120/80 or 140/90 means that a person’s heart muscle and renal system are functioning correctly, and there is no reason to worry about health. In young people, indicators of 90/60 are considered normal, if the person feels well and does not complain of dizziness, weakness and weather sensitivity.
Weak pulse with high blood pressure
Also, indicators of upper and lower blood pressure are divided according to the norm depending on age groups:
- 16–20 years – normal values are 100/70, 120/80;
- 20–45 years – there is no reason to worry if the pressure is fixed at 120/70, 130/80;
- 50–60 years – normal blood pressure is 140/90;
- over 60 years old - blood pressure fluctuates within 150/90.
A gradual increase in blood pressure with age is the result of changes in the condition of the vascular walls, capillaries lose their former elasticity, and the heart muscle wears out. If you do not keep the aging process and natural wear and tear of the body under control, a disease may develop that affects all internal organs and systems and requires correction with medications - it is called hypertension.
The first degree of hypertension occurs with an increase in systolic pressure to 160 mm Hg, the second degree is diagnosed at the upper level of 180 mm Hg, and the third (dangerous to health and life) is characterized by surges in systolic blood pressure above 180 mm Hg.
Conclusion
The optimal difference between systolic and diastolic pressure is 70
is 40 mmHg. But a slight deviation of 10 units up or down is also within acceptable limits.
blood pressure prevention
If the pressure changes by 20 more or less, and you feel normal, most likely there was an incorrect pressure measurement. If your health really gets worse, you should immediately consult a doctor.
In case of difference between systolic and diastolic pressure
is sixty or more, this is the risk of developing heart and vascular diseases. In this case, you must constantly consult your doctor. To make an appointment with our specialist, leave a request on the website or call.
What you need to know about diastolic pressure?
The diastolic pressure indicator characterizes the degree of resistance of blood vessels and their permeability to blood. The health of the vascular system is determined by two main factors: the elasticity of their walls and the functioning of the kidneys. The human body contains a large amount of fluid; without its circulation, metabolism is impossible, and blood plays a crucial role in this process. It passes through the kidneys, which act as a kind of filter, regulate water-salt balance and remove toxins from the blood along with urine.
With this mechanism, an increase in diastolic pressure is usually associated with a violation of the removal of fluid from the body, an increase in its volume and an increasing load on the walls of blood vessels. If lower blood pressure exceeds normal levels for a long time, the risk of heart attacks and strokes increases. If it decreases for a long time, problems arise with the supply of oxygen to tissues and organs. Because of this, dizziness and fainting occur, especially during physical activity.
The causes of low diastolic pressure may be bleeding, prolonged hunger and dehydration, allergies with anaphylactic shock. The indicator decreases with insufficient production of the hormone renin, which regulates vascular tone. The decrease also occurs due to stress, fatigue and tuberculosis.
Danger
An increase in lower pressure often has no symptoms, and a person does not even know about it. They may be discovered during a routine examination or when visiting a doctor for other reasons. There is a misconception that only elevated upper blood pressure threatens health and life, but in fact, an increase in lower blood pressure is no less dangerous. The heart in this state is constantly tense and practically does not relax. The blood flow in it is disrupted, the disease progresses, structural changes begin to occur, which ultimately become irreversible.
It is important to know that high lower blood pressure cannot be ignored. It leads to organ dysfunction and, without treatment, can result in death within six months. There is a high risk of developing thrombosis, heart attacks, and strokes.
Treatment
High diastolic pressure can be reduced by eliminating the cause of the disorder. To do this, you should undergo an examination (blood test, ECG, x-ray), which will determine the causes of the condition. It is important to adhere to the treatment regimen drawn up by your attending physician, taking all prescribed medications and constantly monitoring your well-being using a home blood pressure monitor. Help to lower regularly rising blood pressure:
- ACE inhibitors;
- diuretics;
- calcium antagonists;
- alpha blockers;
- beta blockers;
- angiotensin 2 antagonists.
Blood pressure-lowering drugs are selected by a doctor, as they have a large list of contraindications and side effects that must be taken into account when drawing up a treatment regimen. An integrated approach will allow you to increase the effectiveness of therapy: taking medications, correcting your diet, giving up bad habits, and traditional medicine recipes.
Tablets and other potent medications are practically not used in the treatment of low blood pressure. To correct the condition, the disease that led to it is treated. If no deviations in the functioning of the body are found, then doctors recommend using folk remedies. These are healing herbal decoctions, tinctures of ginseng root and eleutherococcus. Treatment is long-term – at least 40 days. Raising your blood pressure to normal levels, you should regularly monitor your condition by visiting a doctor and measuring blood pressure at home.
Reduced upper pressure
Low upper pressure may be associated with lifestyle or illness. In the first case, we are talking about constant overwork and systematic stress, lack of sleep and excessive physical activity. As for pathologies, a decrease in systolic pressure is caused by:
- Thyroid diseases, hormonal imbalances;
- Diabetes;
- Vegetovascular dystonia;
- Arrhythmia;
- Heart failure.
The cause may be prolonged depression. In any case, to normalize the pressure, you need to consult a doctor and identify the factors that contributed to the decrease in pressure. Usually the doctor recommends mainly preventive measures such as strong tea, contrast showers, and healthy sleep. But in some cases, drug treatment is required.
High bottom pressure
The cause of high lower pressure is usually impaired elasticity of blood vessels, their spasms or narrowing of the lumen due to accumulated cholesterol. An increased rate is recorded when:
- Kidney pathologies;
- Malfunctions of the adrenal glands;
- Vascular diseases;
- Impaired blood flow;
- Metabolic disorders;
- Overfatigue (physical or mental).
The cause may also be long-term use of certain medications. The doctor’s primary task is to identify the cause of the changes, and only then prescribe treatment. By the way, lower pressure can increase under the influence of external factors, for example, frequent stress, which causes the release of adrenaline and constriction of blood vessels, bad habits that deplete the heart muscle, poor nutrition, which contributes to the accumulation of cholesterol in the blood vessels and the accumulation of excess weight.
Diagnostics
Systolic blood pressure can be determined using a special device - a tonometer.
In addition, the patient may be recommended the following types of diagnostic studies:
- Vascular Dopplerography;
- Cardiogram of the heart;
- General and biochemical blood test;
- ECHO.
It is important to learn how to independently determine systolic pressure in order to prevent the development of a pathological process and promptly seek help from qualified specialists!
Blood Pressure Tablets: Part I
High blood pressure is one of the most common health problems in Russia. This disease is especially common in older people who have to “take pills” to feel good and relieve stress on the heart. What is blood pressure, why does it rise too much, how diuretic medications help normalize it and how to take them correctly - read about all this in our article.
What is blood pressure
When the heart muscle contracts, it forcefully pushes out a large volume of blood, putting pressure on the walls of the blood vessels. Depending on the location, this pressure is called arterial (BP), venous and capillary. Pushing a fluid as thick as blood through 100 billion capillaries is no easy task. Due to the natural resistance of this complex network of microscopic vessels, the blood pressure “at the entrance” to the heart is much lower than “at the exit” from it.
The blood pressure “at the exit” of blood from the heart (that is, at the moment of its contraction) is called systolic, and the blood pressure “at the entrance” to the heart at the moment of its relaxation is called diastolic.
The average norm for an adult is considered to be 120/80 mm. rt. Art.; The first number in this case means systolic blood pressure, and the second number means diastolic. Thus, normally, the resistance of the capillary network “eats” 34% of the initial “power” of the blood flow.
In practice, the ratio of the two blood pressure readings varies greatly among different people and even within the same person at different points in time. It depends on a number of factors: heart rate, condition of blood vessels, elasticity of their walls (this parameter is skillfully regulated by the brain), etc.
Why is blood pressure rising?
Arterial hypertension (AH), also known as hypertension, is one of the most common diseases in the world. According to the latest WHO data, about 1.13 billion people worldwide suffer from high blood pressure. Blood pressure readings of 140/90 mm are considered elevated. rt. Art. and higher at rest.
The most common symptoms of a hypertensive crisis (a sharp increase in blood pressure in patients with hypertension) are headache, shortness of breath, chest pain and fatigue. Some patients experience dizziness, hear ringing in the ears, or notice redness on the face and chest.
The main cause of hypertension is excessive activity of the renin-angiotensin system (RAS). It is a cascade of chemical reactions that occur in the body in response to a decrease in blood pressure: the enzyme renin contained in the kidneys is converted into the enzyme angiotensin I, and then into angiotensin II. The latter is a powerful vasoconstrictor. The narrower the vessels, the higher the pressure. Angiotensin II also reduces the excretion of sodium and water by the kidneys. The more water in the tissues of the vessels, the smaller their diameter, which means the higher the pressure.
Arterial hypertension is also associated with an excess of calcium in the cells of blood vessels, as well as with an increased concentration of sodium in the vessels and in the blood. Many people know that calcium is good for bones and teeth, but not everyone realizes how important it is for the body as a whole. In fact, calcium is necessary for the transmission of nerve impulses, muscle contraction, blood clotting, the immune response, and so on. Without this metal we would not be able to think, move, or even live.
But in the body, as in life, everything is good in moderation. Calcium overload in vascular cells leads to hypertrophy of their muscle tissue. And this, in turn, means a thickening of the vessel wall and a decrease in its lumen. The “tube” becomes narrower, and, as a result, the pressure on its walls increases.
Why does calcium overload occur? Calcium metabolism in the body is regulated by hormones, and their level, in turn, depends on the concentration of other important substances. Thus, risk factors for hypertension are: obesity, sedentary lifestyle and hyperlipidemia (fat concentration), diabetes, smoking and alcoholism. In addition, old age is a key risk factor.
In the case of sodium, the risk factor is the abuse of salty foods and hormonal disorders that slow down the removal of this element from tissues. Sodium can accumulate in the blood, increasing its volume by binding water molecules. The more blood passes through the vessels per unit time, the greater the pressure on the walls of the vessels. In addition, the accumulation of sodium in the endothelium (a thin layer of cells lining the inside of blood vessels) leads to its swelling (essentially, edema) and, as a consequence, to a narrowing of the lumen of the vessel.
How do diuretics work?
In this article, we will look at only one class of drugs that are used to treat hypertension - diuretics. These medications are designed to “correct the situation” with sodium, while calcium metabolism and the functioning of the RAS are corrected by other drugs, which we will talk about in the following materials.
Diuretics improve the excretion of urine from the body, and along with it, water. Excess sodium and water leave the blood, its volume decreases and blood pressure decreases.
Diuretics act on the nephron, a structural unit of the kidney that performs filtration, reabsorption (reabsorption) and secretion of various substances. They reduce the return of previously “filtered” sodium and potassium ions into the blood. The lower the sodium reabsorption, the lower the water reabsorption. Instead of entering the blood, the water leaves in the urine.
Three types of diuretics are used to treat arterial hypertension: loop, thiazide and potassium-sparing. Loop diuretics are so called because they act on a special part of the nephron - the loop of Henle. Potassium-sparing ones differ from others in their ability to influence only sodium ions. And all thiazide diuretics are derivatives of the substance benzothiadiazine.
The latter are also capable of acting directly on the walls of blood vessels. They reduce the concentration of sodium ions in the endothelium, which reduces its swelling.
Examples of loop diuretics are torasemide and furosemide. Thiazide diuretics include indapamide. Potassium-sparing diuretics include spironolactone and triamterene.
How to take diuretics?
When taking a number of diuretics, especially loop diuretics as the most “powerful” ones, you should remember the risk of hypokalemia (potassium deficiency). It leads to serious problems with various muscle tissues - myalgia, paralysis, breathing problems and intestinal obstruction.
This is a relatively rare condition because potassium is a very common element in food. However, such risks can be caused by a combination of the action of diuretics, which “expel” potassium into the urine and, say, the consequences of prolonged diarrhea or laxative abuse. Also, medications called beta-agonists (salbutamol, fenoterol, etc.) can affect potassium concentration.
In this regard, we recommend that you begin treatment with diuretics only under the supervision of a doctor who will not prescribe incompatible drugs. Obviously, this problem does not apply to potassium-sparing diuretics.
Diuretics do not have strict guidelines for when to take oral forms, however, as is the case with many other drugs, it is better to take them before meals or a couple of hours after. Any medicine is unlikely to benefit from unnecessary interactions with food.
We wish you health, eternal 120/80 and a rational approach to treatment, including professional help from doctors!
Mark Volkov, editor of the online magazine for pharmacists and medical workers “Katren-Style”
Photo depositphotos.com The author’s opinion may not coincide with the opinion of the editors
How to quickly normalize blood pressure
A gap in the pulse difference of 50 units in the upward direction requires contacting specialists.
But the first steps to normalize blood pressure are usually taken independently. Recommend:
- take a horizontal position;
- restore breathing;
- open the window for oxygen access;
- if blood pressure is high, raise your head; if blood pressure is low, raise your legs;
- provide freedom to the neck;
- high blood pressure involves hot foot baths to improve blood flow from the brain;
- acupressure and breathing exercises are acceptable: hypotension requires rubbing the earlobes, hypertension requires circular movements from the ears to the back of the head.
Deviations in indicators
The heart is a four-chamber pump that pumps biological fluid enriched with oxygen to the periphery. Its work is recorded in several quantities. The upper one is a bioindicator of myocardial contractile potential. Bottom – components of the blood supply system.
Systolic pressure
Its ideal values are considered to be 120 units, the acceptable norm is 130, excess is 140, minimal hypertension is up to 170, high blood pressure is from 180. Any fluctuations in the indicator indicate an imbalance in the work of the myocardium.
Provoking moments of lowering the upper level are:
- overstrain: physical, mental;
- pregnancy;
- bradycardia of any origin;
- head bruises;
- insomnia;
- incorrect insulin production;
- imbalance of the heart valve apparatus.
Some triggers are physiological in nature. Indicators of the indicator of myocardial contractility are normalized without additional effort when the cause that caused their decrease is eliminated. An example is pregnancy, associated with a restructuring of the blood supply, when the upper level of pressure drops by approximately 10 units due to adaptation to the new conditions of the body’s existence. After childbirth, everything falls into place.
Athletes, through regular training, acquire the ability to work, saving energy during high loads, which automatically reduces the heart rate, causing a decrease in systolic blood pressure. The rest period normalizes myocardial contractions.
Pathological bradycardia or slow heart rate is characteristic of heart disease and atherosclerosis. It warns of the possible development of acute cerebrovascular accident - stroke or acute myocardial infarction - AMI.
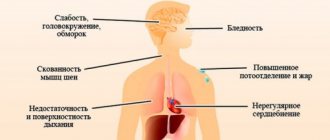
Diabetes mellitus provokes blood hyperviscosity, which reduces the upper limit. Regardless of the reason that caused the decrease in pressure, the patient feels:
- apathy, drowsiness;
- hyperhidrosis;
- migraine pain;
- pre-fainting states;
- forgetfulness, irritability.
All this is a reason to seek medical advice.
The question is extremely important, since often fluctuations in blood pressure occur with virtually no symptoms. AMI and stroke develop against the background of apparent well-being. Therefore, clinical examination or preventive examinations at least once a year are normal practice for patients who care about their health. Only a doctor can give a correct assessment of the condition of the heart and blood vessels; he also prescribes additional examinations if necessary and corrects the pathology.
Causes of increased systolic pressure:
- diseases of the cardiovascular system;
- nervous tension;
- alcohol abuse, nicotine addiction;
- physical inactivity, obesity;
- aortic defects;
- high cholesterol with the formation of atherosclerotic plaques;
- pathology of the kidneys, thyroid gland;
- age.
Clinically, a high upper bioindicator is manifested by nausea, nervousness, insomnia, ringing in the ears, constant palpitations, swelling of the legs, and loss of sensitivity in the fingers.
Such symptoms should force the patient to seek medical help.
Diastolic pressure
The rest period of the myocardium is diastole. This is an indicator of capillary strength. Its optimal value is considered to be 80 units, the acceptable norm is 90, elevated is 95, mini-hypertension is 110, high is everything above 110.
A low diastolic limit requires diagnosing the functional integrity of the kidneys. In addition, it correlates with menstruation in women: blood loss leads to a minimization of its volume, that is, a decrease in the indicator. The following are considered triggers for low blood pressure: prolonged fasting, sensitization of the body, infection with Koch's bacillus, stressful situations, climate change.
Signs of low diastolic pressure:
- fainting;
- a sharp decrease in working capacity;
- dyspnea;
- chest pain;
- visual disturbances;
- cardiopalmus;
- vomiting - up to hypotonic crisis, coma.
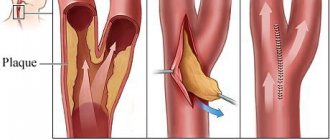
An increase in the diastolic biomarker confirms the preservation of the tone of the peripheral capillaries due to the thickening of their membrane, narrowing of the lumen - the main trigger of hypertension.
The diagnosis of the disease is made on the basis of long-term blood pressure values greater than 140/90. The causes of the pathology are recognized:
- heredity;
- alcoholism, nicotine addiction;
- gaining extra pounds;
- diuretics;
- osteochondrosis, other pathologies of the spinal column;
- depression.
Fluctuations in blood pressure are a sufficient reason for complete clinical and laboratory testing. Self-medication is unacceptable, as it can provoke complications leading to death.
Increased systolic pressure
High upper pressure is a sign of:
- Overactive thyroid gland (thyrotoxicosis);
- Severe anemia;
- Bradycardia (decreased heart rate);
- Aortic valve insufficiency;
- Reduced elasticity and increased density of the vascular wall (for example, atherosclerosis of the aorta).
This condition is called isolated systolic hypertension or systolic hypertension. Upper blood pressure often increases during adolescence. This is due to hormonal changes in the body and is not considered a deviation. With the completion of puberty, the indicators return to normal. True, such changes increase the chances of developing hypertension in adulthood.
Treatment of systolic hypertension is generally similar to those taken for normal hypertension. This also applies to prevention. The main thing is to identify the disease in time, regularly monitor your blood pressure and take medications prescribed by your doctor, including those that help lower blood pressure. In addition, you need a diet, adequate physical activity, and protection from stress.
Features of treatment
A set of measures to relieve a pathological condition is aimed at eliminating the cause.
- Atherosclerosis requires drug therapy or surgery. Among the medications used are: statins and fibrates, which reduce the concentration of blood cholesterol (Rosuvastatin, Fenofibrate); unsaturated fatty acids that stimulate the removal of toxic fats from the body (Linetol); vitamins that nourish the endothelium and block the formation of atherosclerotic plaques. Among the surgical methods that deserve attention are laser angioplasty, vascular stenting, bypass surgery - creating a bypass blood flow, endarterectomy - excision of part of the inner layer of an artery with an atherosclerotic plaque.
- Aneurysms are treated only with surgery.
- Pericarditis involves pericardiectomy of the affected area with recovery in 60% of cases.
- Aortic stenosis requires replacement of the valve with an artificial one, which lasts from 8 to 25 years, taking into account the properties of the selected material.
- Heart rhythm disturbances are treated with antiarrhythmic drugs, sometimes with the help of a defibrillator or the installation of a pacemaker.
- Chronic kidney pathology is treated with anti-inflammatory therapy, antibiotics, anticoagulants, and physiotherapy.
- Tumors are corrected with cytostatics and other antitumor drugs. Failure requires a decision on the operation.
- Left ventricular failure requires either surgery or a combination of medications:
- ACE inhibitors – reduce diastolic pressure;
- cardiac glycosides improve myocardial contractility;
- nitrates to improve oxygen supply to the heart;
- diuretics to relieve swelling.
Acute left ventricular failure requires emergency hospitalization in a specialized hospital.
ISH therapy is prescribed by a cardiologist or therapist after a full clinical and laboratory examination and requires compliance with several rules: the force of the blood hitting the vascular wall is gradually reduced so that adaptation to new conditions occurs and ischemia does not develop; medications are required to affect only the upper blood pressure reading; There should be no negative impact on the kidneys or brain. For this purpose the following are appointed:
- antihypertensive drugs: calcium antagonists, beta blockers, ACE inhibitors, angiotensin blockers;
- diuretics: a small blood volume reduces the upper limit, cardiac output;
- drugs that stimulate blood flow in the kidneys, brain, heart;
- neuro-, cerebroprotectors – improve the nutrition of nerve cells, prevent stroke.
To increase efficiency, various combinations of drugs are used under medical supervision.