If, during the period of bearing a child, a woman periodically notices an increased heart rate and discomfort, this is nothing more than tachycardia.
The normal rhythm of the heart is 60-90 beats per minute. With tachycardia this figure is exceeded. This is often observed during pregnancy - the woman’s body is overloaded, the cardiovascular system and all other organs work for two. In such a difficult and responsible period in life, it is important to carefully take care of your health. An increased heart rate is a warning sign.
Tachycardia during pregnancy is a pathology that can negatively affect not only the health of the expectant mother, but also interfere with the proper development of the baby in the womb. Therefore, when the first signs of palpitations appear, you should immediately consult a doctor.
Services and prices
CTG: (Multiple pregnancy)
1500 ₽
Sign up
CTG: (Fetal cardiotocography)
1300 ₽
Sign up
Cardiotocography (CTG) is a functional diagnostic method based on recording the fetal heart rate and uterine contractility during pregnancy and childbirth. Cardiotocography is based on the Doppler effect and the principle of ultrasound. An ultrasonic wave emanates from the sensor, which is reflected from the pulsating heart of the fetus, changes the frequency and is sent back. The monitor's electronic system registers and converts the signal. This recording is called a cardiotocogram.
Two sensors are attached to the pregnant woman's belly. For better contact with the skin of the anterior abdominal wall, a special hypoallergenic gel is applied. At the point of best audibility of the heartbeat (usually in the navel area), a cardiac sensor is applied, which records the fetal heartbeat. If the patient is pregnant with twins, then use two sensors at once or take measurements one by one. The strain gauge records the contractile activity of the uterus and the motor activity of the fetus.
Sometimes the baby's movements are recorded using an additional sensor. During the examination, the device makes loud sounds, which should not be alarmed. This is the baby's heartbeat. The fetus may change its position during the examination, which will lead to incorrect recording. However, thanks to the sound component of the procedure, the doctor can control the correct location of the sensors and rearrange them in time to follow the child.
Cardiotocography, together with the results of other studies, makes it possible to recognize serious disorders, including fetoplacental insufficiency, intrauterine fetal hypoxia, various anomalies in the development of the fetal cardiovascular system, indirect signs of intrauterine infections, and the threat of premature birth.
Increased heart rate in the third trimester of pregnancy
Periodic increases in heart rate in the third trimester are quite possible; more often they do not pose a danger to either the fetus or the mother. The reasons for this increase in heart rate may be:
- dynamic lifestyle and excessive stress in a pregnant woman;
- various stresses, psycho-emotional stress, depression;
- too much weight gain;
- consumption of caffeine-containing products;
- long periods of lying on your back;
Short-term increases in heart rate (5-10 minutes) are usually harmless. Women usually feel slight discomfort, sometimes accompanied by palpitations
- weakness, malaise;
- cardialgia;
- dizziness;
- frequent urination.
In these cases, it is better for the pregnant woman to inform her doctor, who will prescribe an examination and, if necessary, a consultation with a cardiologist.
When is the examination done and how often?
The study is carried out no earlier than 32 weeks. It is by this time that the nervous and cardiovascular systems reach a certain maturity. By 8 months, the myocardial reflex is formed - the relationship between cardiac activity and motor activity of the fetus. At the same time, the activity-rest cycle is established. Rhythmic changes in fetal sleep and wakefulness follow each other throughout the remaining period of pregnancy.
Cardiotocography must be performed 2 times during the 3rd semester. However, the frequency of the study is determined by the doctor based on the mother’s medical history, pregnancy history, results of other examinations and risk factors.
Indications for the study
The purpose of cardiotocography is timely diagnosis and detection of fetal disorders. Based on data from a number of functional diagnostic studies, such as ultrasound, CTG, Doppler measurements, anamnesis, the obstetrician-gynecologist chooses pregnancy management tactics, treatment, the optimal date and method of delivery.
Indications for additional cardiotocography may include:
- Rhesus conflict
- Preeclampsia in the second half of pregnancy
- Maternal diseases
- Post-term pregnancy
- History of premature birth
- Fetal growth restriction
- Pregnancy pathologies and fetal development abnormalities identified by ultrasound
- Oligohydramnios or polyhydramnios
- Multiple pregnancy
- Complicated obstetric and gynecological history (previous abortions, miscarriages, premature births)
- Changes in the nature of fetal movements (complaints about a decrease or increase in the number of fetal movements per day)
Treatment
The feasibility of treating tachycardia is assessed based on the results of an examination of the pregnant woman. If palpitations are physiological and transient, the doctor may recommend lifestyle changes and eliminate psycho-emotional stress. According to indications, sedatives approved for use during pregnancy may be prescribed. If tachycardia is associated with cardiac or endocrine pathology, drug treatment is selected by the appropriate specialist.
Draw your attention to! This article is not a call for self-medication. It is written and published to improve the reader's knowledge about his own health and understanding of the treatment regimen prescribed by the doctor. If you experience similar symptoms, be sure to seek help from a doctor. Remember: self-medication can harm you.
Preparation for the procedure
The study does not require special preparation. However, it is worth considering the duration of the procedure. It will be important for mom to relax and be calm. On the eve of the procedure, the pregnant woman is recommended to get a good night's sleep and rest. On the day of the study, you should take care of a light meal 1-2 hours before. And immediately before the procedure, go to the toilet. During CTG, the expectant mother should not be distracted or disturbed by anything. You can take a book or magazine with you, but electronic devices, including your phone, will have to be turned off, as the equipment creates interference with the recording.
What sports can you do during pregnancy?
What activities are allowed for pregnant women:
First of all, when starting to exercise during pregnancy, it is necessary to take into account the level of physical fitness before conception . If a woman has been regularly involved in sports for many years, received intense exercise, naturally, and during pregnancy in the absence of contraindications, she can afford more intense exercise, albeit with some control. So, in particular, the heart rate 5 minutes after completing the exercise should not exceed 100 beats per minute, and blood pressure should normalize on its own after the same period of time. During training, you should try to limit the time of intense physical work to 15 minutes (intensive work is understood as one during which the heart rate exceeds 150 beats per minute). It is better to increase the time allotted for warming up and warming up. The training time itself should ideally not exceed 1.5 hours.
Women who do not engage in intensive fitness before pregnancy need to carefully approach the start of exercise during pregnancy, start small and gradually, within reasonable limits, increase the load.
Hiking
One of the simplest, accessible to every woman, but very effective physical activity, allowed for absolutely all pregnant women, regardless of their preparation and well-being, is walking. Such exercises tone the muscles of the legs, buttocks and back, prevent the appearance of varicose veins and hemorrhoids, and fight venous congestion in the pelvis. Regular walks improve uteroplacental blood flow, resulting in the fetus receiving more oxygen and nutrients.
Cross country skiing
In winter, you can regularly go for cross-country skiing - this sport is considered safe. After 24-25 weeks, you must wear a support bandage for pregnant women while hiking or skiing.
Walking up the stairs
Walking up the stairs is also useful for pregnant women. The main condition is to take your time, breathe evenly and calmly.
Swimming
Swimming is perhaps the most optimal sport for pregnant women. Swimming has a very beneficial effect on both mother and baby. Exercises in water relieve the spine, strengthen the muscles of the back and chest, massage tissues, improve blood circulation in organs and tissues, swelling and flatulence disappear. In addition, swimming eliminates the possibility of overheating, dehydration and injury to a woman, as well as excessive stress on the joints. Swimming is a great way to keep your body in good shape and a great opportunity to get it in order after the baby is born. Water is an excellent shock absorber, allowing you to optimally distribute the load on the body during any type of movement. You can simply float on the water, walk in the water, swim, or do water aerobics for pregnant women. Fitness centers have special water aerobics programs for expectant mothers under the guidance of instructors. The only points that you need to remember when going to the pool are that the swimsuit is well-fitted and does not squeeze your stomach; you must take a bottle of clean drinking water with you to replenish fluids after class, and evaluate the cleanliness of the pool in which the classes are taking place. swimming.
Yoga
Yoga is also an excellent exercise option while pregnant. Almost all of its varieties are suitable for this, but it is still better, especially for beginners, to practice yoga specially adapted for pregnant women, under the guidance of an experienced instructor. This type of yoga will not harm either mother or baby; there are no inverted poses or exercises that must be performed while lying on your back. Another argument in favor of yoga is that when performing the exercises, a lot of time is devoted to breathing and relaxation. This has a very beneficial effect on the development of the baby (proper breathing improves blood circulation and he receives more oxygen), and also prepares the mother for childbirth.
Gymnastics for pregnant women
There are several options for specially designed gymnastics for pregnant women. It is designed taking into account all the physiologies and needs of pregnant women. Exercises in these complexes are aimed at strengthening the cardiovascular and respiratory systems, the muscles that are involved in the process of childbirth - at strengthening the abdominal press and pelvic floor. Gymnastics for pregnant women has a positive effect on maintaining posture and strengthening the spine. You can do gymnastics for pregnant women at home yourself, picking up basic exercises from special magazines or from the Internet. Many fitness clubs create special groups for expectant mothers. In the group, pregnant women engage in physical exercises under the guidance of experienced instructors, who will show the necessary exercises, point out possible mistakes, and in addition, by exercising in the group, women can communicate with other expectant mothers. In fitness clubs, classes for pregnant women are also carried out using inflatable sports balls - fitballs. Fitball exercises are also aimed at strengthening the back muscles, preparing muscles and ligaments directly or indirectly involved in the birth process, and improving blood supply to organs and tissues.
Pilates
Pilates classes are encouraged during pregnancy. It helps not only to strengthen the muscles actively involved in childbirth, in particular the pelvic floor muscles, but also to master the skills of proper breathing and relaxation. These skills will be useful during childbirth to reduce pain during contractions.
In the first trimester of pregnancy, fitness helps fight mild toxicosis, pain in the lumbar region that occurs due to pressure from the growing uterus, and helps normalize intestinal function. During this period, the formation of all the baby’s organs and systems occurs and its connection with the mother’s body is still weak. It is recommended to refrain from sharp bends and bending of the body, sudden lifting of the body from a lying position, and raising straight legs. Since during this period the need of body tissues for oxygen increases, and the expectant mother is often worried about toxicosis or increased sensitivity to odors, it is best during this period to pay more attention to quiet walking or skiing and not to visit the stuffy halls of a fitness club with their special aromas.
the most favorable for physical exercise . In the second trimester of pregnancy, the active formation of the placenta and the mother-fetus circulation occurs, the pressure of the uterus on the vessels increases, which leads to edema and the appearance of varicose veins. Metabolism includes placental hormones, which enhance the growth of the uterus and mammary glands; an enlarged abdomen leads to a change in posture, and possibly flattening of the foot. Exercising in the second trimester of pregnancy helps maintain flexibility and mobility of joints, and also prevents varicose veins and edema. In the second trimester, it is recommended to do gymnastics for pregnant women, Pilates and especially swimming. Swimming, like no other sport, helps to “unload” the spine and for some time feel your body the way it was before pregnancy.
In the third trimester , the uterus enlarges, the load on the heart increases, diaphragmatic breathing is difficult, venous outflow from the legs and pelvis worsens, and the load on the spine and arch of the foot increases. Classes during this period are aimed at improving blood circulation in all organs and systems. The overall load must be reduced. Relaxation exercises are of great importance. Swimming also brings significant benefits during this period.
How long does CTG last?
The procedure lasts from 30 to 60 minutes depending on the baby’s activity. After 32 weeks, the fetus is characterized by periods of sleep and wakefulness. The active state lasts 50-60 minutes, while the calm state lasts 20-30 minutes. When assessing cardiotocography, the leading period is the period of fetal wakefulness. Therefore, the duration of the study may vary.
CTG indicators
When analyzing CTG, a number of indicators are taken into account.
- Basal rhythm.
The cardiac sensor records the heart rate, and the cardiotocograph calculates the average fetal heart rate, which remains unchanged over 10 minutes or more. This indicator is called the basal rhythm. Normally, the fetal heart rate is subject to slight changes. - Rhythm variability.
Rhythm variability is indicated by the number and amplitude of deviations from the basal rhythm. - Acceleration periods.
Acceleration is a period of increase in fetal heart rate by 15 or more beats per minute for 15 or more seconds compared to the basal rhythm. - Periods of deceleration.
Decelerations are episodes of heart rate slowing by 15 heart beats per minute or more, lasting 15 seconds or more. Decelerations usually occur in response to uterine contractions or fetal movements. - basal rhythm within 110-150 beats/min
- amplitude of heart rate variability - 5-25 beats/min
- decelerations are absent or sporadic, shallow and very short
- 2 or more accelerations are recorded during 10 minutes of recording. If this type of CTG is detected within a short period of study, recording may not be continued.
WHO recommendations criteria for a normal cardiotocogram are the following indicators:
If the results of your CTG do not match the WHO criteria, then this does not indicate pathology. Cardiotocography is a very sensitive method to external influences. Correct interpretation of the examination results is possible only by a specialist in conjunction with other data.
conclusions
The pulse rate in pregnant women in the third trimester differs most greatly from the average values in the population, exceeding them by 15-20 beats per minute. But this is a small price to pay for the coexistence of two organisms in one body. Such changes are physiological and explainable from a scientific point of view.
You should be concerned when your heart rate changes suddenly and for no apparent reason. If an expectant mother in the eighth month of pregnancy climbed the stairs on foot to the fifth floor, and at the same time her pulse jumped to 100 and dropped to 75 after a short rest, this is the norm. And if it’s up to 115, she has a headache, the patient is lying in bed, they go to the doctor.
Decoding the results
CTG interpretation should be done only by a specialist. This is a complex process that requires knowledge and experience. The cardiotocogram consists of two types of graphs - tachogram and hysterogram. The tachogram reflects changes in the fetal heart rate. The time is measured horizontally, and the number of beats per minute is measured vertically. Thus, the graph deviates downwards when the heart rate decreases, and upwards when it increases. When measuring fetal motor activity, the indicators are displayed under the tachogram. The second graph, usually located at the bottom of the cardiotocogram, displays the force of uterine contraction.
The first step is visual interpretation of the CTG. However, to reduce the subjectivity of the assessment, it is customary to use rating scales. There are two methods: the Gauthier scale and mathematical analysis.
The ten-point Gauthier scale is a questionnaire where the doctor is asked to evaluate the basal rhythm, variability, number of accelerations, decelerations and fetal movements. Each indicator is given a score from 0 to 2 points.
Based on the sum of points, a conclusion and recommendations for further observation are formed. This scale has many modifications.
The second assessment method is mathematical. When interpreting computer-processed data, the fetal condition indicator (FSI) is used.
- 1-2 - signs of initial violations
- 2-3 - pronounced violations
- >3 – critical condition.
Scores above 2 indicate a dangerous condition that requires hospitalization in a maternity hospital.
The CTG method, like any other, has its disadvantages and errors. In some cases, fetal oxygen consumption may decrease regardless of the presence of pathology. For example, fetal compression of the umbilical cord causes short-term disruption of blood flow. In this case, cardiotocography will register fetal hypoxia. However, these changes are temporary and when the position of the fetus changes, blood flow will be restored. Therefore, the conclusion based on the results of CTG is not a diagnosis, and only a doctor should evaluate and interpret the cardiotocogram data.
What affects heart rate in pregnant women?
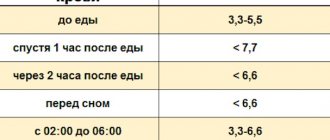
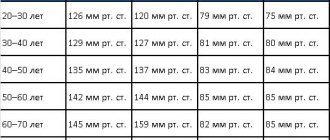
From the very beginning of pregnancy, a woman's hormonal background changes significantly. Hormones produced during gestation have a huge impact on cardiac activity, and, consequently, the speed of the heartbeat. It is important to note that pulse is determined together with blood pressure, since these indicators are interrelated. In most cases, not only a change in pulse is observed, but also pressure surges.
Fluctuations in heart rate during pregnancy are caused by the following factors:
- Gestation period. For the 1st, 2nd, 3rd trimesters, as well as just before childbirth, normal values may vary.
- Multiple pregnancy. If a woman is expecting not one, but two babies, then the heart pumps double the amount of blood necessary for their life support. As a result, the heart rate increases significantly.
- Changes in the position of the heart. Starting from the 2nd trimester, the enlarged uterus begins to put pressure on the diaphragm, thereby forcing the heart to work intensively.
- An increase in blood volume, which increases by a maximum of 1.5 liters. As a result, the heart pumps more blood, which explains the high load on it.
- Decreased lung capacity. In the later stages, the rise of the diaphragm leads to their compression, so in order for the body to have enough oxygen, the blood begins to release it in larger quantities.
- Excess body weight.
- Anemia. When the level of hemoglobin in the blood decreases, anemia develops, which often provokes tachycardia.
- Stress. If a woman is subject to psycho-emotional stress and is regularly under tension, then she may develop a rapid heartbeat.
- Drinking strong tea, coffee, alcohol. Smoking can also provoke attacks of tachycardia.
- Lying on your back for a long time. With this position of the body, the uterus compresses the abdominal aorta, the blood flow becomes worse, and the heart beats faster.
- Diseases that may worsen or develop during pregnancy. Among them are infections, heart disease, thyroid disorders, hyper- or hypotension, pathologies of the kidneys, liver, etc.