Causes of esophageal varicose veins
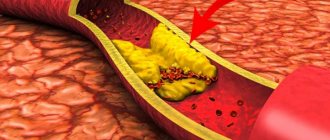
The disease develops against the background of increased pressure in the portal vein (also known as the portal vein), but other pathologies (hypertension, congenital anomalies, and so on) can contribute to its occurrence. Esophageal varicose veins, the causes of which lie in pathological changes in the portal vein, often begin to progress with previously diagnosed severe diseases of the liver or pancreas - cirrhosis, tumors, insufficiency. The disease often develops against the background of severe diseases of the thyroid gland, in which case we will be talking about pathological disorders of the vena cava.
According to statistics, esophageal varicose veins are more often diagnosed in men aged 50 years and older.
How is the disease diagnosed?
Esophageal varicose veins are diagnosed by:
- Studying anamnesis.
- Medical examination. During it, you can note such signs of varicose veins as swelling, changes in the color of the skin and mucous membranes.
- Laboratory research. To study varicose pathology, the patient undergoes general and biochemical blood tests. Specialists count the number of platelets, examine liver enzymes, serum iron, protein, and lipid spectrum.
- Instrumental research. If varicose veins of the esophagus are suspected, ultrasound, esophagoscopy and x-ray diagnostics are performed. These studies are aimed at studying a specific area of the esophagus. The remaining organs of the peritoneum are also studied.
Esophageal varicose veins: symptoms
Depending on the degree of development, the following signs are distinguished:
- First degree. The diameter of the veins is increased by no more than 3 mm, the formation of single nodes is possible. Diagnosis of the disease is possible only by the endoscopic method; there are no clinical signs.
- Second degree. A rather dangerous period of varicose veins of the esophagus - there are no symptoms (even the mucous membrane of the organ still remains unchanged), but at the same time the contour of the veins already becomes unclear, and X-ray diagnostics reveal thickenings on the veins (harbingers of nodules). Already at this stage, bleeding is possible, which in the absence of immediate medical attention often leads to death.
- The third and fourth degrees of varicose veins of the esophagus are characterized by severe symptoms - the patient is often bothered by heartburn, pain occurs in the sternum, shortness of breath is possible, not only during physical activity, but also at rest. Often the disease is diagnosed only in the later stages of its development, when the first bleeding appears; blood is released directly from the esophagus or found in the vomit.
Key features of the intervention!
The advantages of vein embolization include:
- High speed of intervention. The operation takes 30-60 minutes. Complex procedures may take longer.
- No significant discomfort. Pain and any discomfort during vein embolization are relieved with special modern medications.
- Speed of recovery after intervention. The patient will have to stay in the clinic for only 1-2 days. Note! In some cases, the length of hospitalization after vein embolization increases. In any case, the patient can return to normal life in the near future.
What recommendations do doctors give to patients?
- Strengthening the drinking regime. In the first 7 days after surgery, you need to drink plenty of clean water.
- Elimination of water procedures for 3-5 days. After this, you can take both a shower and a bath.
- Physical peace. It is usually prescribed for 2-3 weeks. Patients are prohibited from lifting heavy objects or playing sports. Bed rest is not prescribed for this period. Slow walks are even beneficial.
What lifestyle should I lead after embolization of esophageal vessels?
Patients should:
- Follow a specially prescribed diet that includes a large number of foods that help reduce total cholesterol levels.
- Avoid heavy exertion.
- Take various medications. They will be prescribed by your attending physician.
- Eat food often enough, but in as small portions as possible. The daily dose is best divided into 5-6 doses. Eating food is undesirable 2-3 hours before bedtime.
- Give preference to boiled dishes. Food can also be steamed. This way it retains a lot of useful substances, is easily digestible and does not become a source of additional harmful cholesterol.
It is forbidden to eat too hot or cold food. This can damage the esophagus and its veins.
Treatment
Treatment of varicose veins of the esophagus begins with finding out the true causes of the development of the disease. If a pathology of the liver, thyroid or pancreas is diagnosed, then it must be treated - the provoking factor must be eliminated or its influence must be weakened. Medications include vitamin complexes, antacids and astringents. If bleeding is diagnosed, there is always a risk of its reoccurrence. In this case, the following is prescribed:
- blood transfusion;
- hemostatic drugs;
- introduction of a special probe that can compress the vessels.
Varicose veins of the esophagus, bleeding in which occurs too often, require surgical treatment.
Surgery is also performed if there is no effect from therapeutic treatment. Can esophageal varicose veins be stopped in this case? The prognosis is more favorable - the survival rate of patients increases 3 times. After any treatment, you must follow the dietary recommendations of doctors, undergo regular examinations and avoid excessive physical activity.
You can find out more about what esophageal varicose veins are and which doctor you should contact on the pages of our website Dobrobut.com.
Literature
- Conn HO Vasopressin and nitroglycerin in the treatment of bleeding varices: the bottomline. Hepatology 1986;6:523–5.
- Corley DA, Cello JP, Adkisson W., Ko WF, Kerlikowske K. Octreotide for acute esophageal variceal bleeding: a meta-analysis. Gastroenterology. 2001 Mar;120(4):946-54.
- Feneyrou B., Hanana J., Daures JP, Prioton JB Initial control of bleeding from esophageal varices with the Sengstaken-Blakemore tube: experience in 82 patients. Am J Surg 1988;155:509–11.
- Feu F., Ruiz del Arbol L., Banares R., et al. Double-blind randomized controlled trial comparing terlipressin and somatostatin for acute variceal hemorrhage. Variceal Bleeding Study Group. Gastroenterology. 1997 May;112(5):1777.
- de Franchis R. Somatostatin, somatostatin analogues and other vasoactive drugs in the treatment of bleeding oesophageal varices. Dig Liver Dis. 2004 Feb;36 Suppl 1:S93-100.
- Grace ND Prevention of initial variceal hemorrhage. Gastroenterol Clin North Am 1992;21:149–61.
- Graham DY, Smith JL The course of patients after variceal hemorrhage. Gastroenterology 1981;80:800–9.
- Hartigan PM, Gehbard RL, Gregorty PB, et al. Sclerotherapy for actively bleeding esophageal varices in male alcoholics with cirrhosis. Veterans Affairs Cooperative Variceal Sclerotherapy Group. Gastrointest Endosc 1997; 46.
- Imperiale TF, Teran JC, McCullough AJ A meta-analysis of somatostatin versus vasopressin in the management of acute esophageal variceal hemorrhage. Gastroenterology 1995; 109:1289–1294.
- Jalan R., Hayes PC UK guidelines on the management of variceal haemorrhage in cirrhotic patients, 2000.
- Jenkins SA, Shields R, Davies M, et al. A multicentre randomized trial comparing octreotide and injection sclerotherapy in the management and outcome of acute variceal haemorrhage Gut 1997;41;526-533.
- Laine L., Cook D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding: a meta-analysis. Ann Intern Med 1995; 123:280–7.
- Laine L., Stein C., Sharma V. Randomized comparison of ligation versus ligation plus sclerotherapy in patients with bleeding esophageal varices. Gastroenterology 1996;110:529–33.
- Lo GH, Lai KH, Cheng JS, et al. A prospective, randomized trial of sclerotherapy versus ligation in the management of bleeding esophageal varices. Hepatology 1995;22:466–71.
- Sanyal AJ, Freedman AM, Luketic VA, et al. Transjugular intrahepatic portosystemic shunts for patients with active variceal hemorrhage unresponsive to sclerotherapy. Gastroenterology 1996;111:138-146.
- Silva G., Quera R., Fluxa F., et al. Octreotide administration and/or endoscopic treatment in cirrhotic patients with acute variceal bleeding: a multicentric study Rev Med Chil. 2004 Mar;132(3):285-94.
- Silvain C., Carpentier S., Sautereau S., et al. A randomized trial of glypressin plus transdermal nitroglycerin versus octreotide in the control of acute variceal haemorrhage. Hepatology 1991; 14:1339.
- Stiegmann GV, Goff JS, Sun JH, Wilborn S. Endoscopic elastic band ligation for active variceal hemorrhage. Am Surg 1989;55:124–8.
- Sung JJY, Chung S, Lai CW, et al. Octreotide infusion or emergency sclerotherapy for variceal haemorrhage. Lancet 1993; 342:637–41.
- Terblanche J., Bornman PC, Kahn D., Kirsh RE Sclerotherapy in acute variceal bleeding: technique and results. Endoscopy 1986 May;18 Suppl 2:23-7.
- Tsai YT, Lay CS, Lai KH, et al. Controlled trial of vasopressin plus nitroglycerin vs. vasopressin alone in the treatment of bleeding esophageal varices. Hepatology. 1986 May-Jun;6(3):406-9.
- Westaby D, Hayes PC, Gimson AE, et al. Controlled clinical trial of injection sclerotherapy for active variceal bleeding. Hepatology 1989;9:274–7.
The main advantages of the vein embolization method used in the center of Professor Kapranov
Endovascular embolization in our center is a low-traumatic procedure. It is fundamentally different from standard surgical interventions in the absence of large incisions in the vein and tissue. In addition, embolization does not require the patient to be put under general anesthesia. This reduces numerous risks and makes intervention possible in the presence of general contraindications to standard surgery.
The advantages of carrying out the intervention at the center of Professor Kapranov also include:
- Experience of professionals. All doctors performed a lot of interventions to restore the functionality of the esophagus. They are ready to help you too.
- Comfortable conditions of stay in any clinic. Embolization of the esophageal vessels will not cause pain or severe discomfort.
- Reducing the likelihood of relapse. The technique used to block the vessel allows you to quickly and reliably stop the blood flow of the vein (vessel) of the esophagus.
- No discomfort when restoring the functionality of the esophagus. During vein embolization, the patient does not experience pain. All unpleasant sensations are eliminated with the help of special medications.
- Short recovery period after intervention for varicose veins of the esophagus. For minor vascular interventions, the patient may be discharged on the day of the procedure. In this case, special care, complex treatment, and regular dressings are not required.
- Minimal number of contraindications and complications. The success of an operation for embolization of esophageal vessels largely depends on the professionalism of the doctor. That is why it is important to choose a surgeon wisely.
- Opportunities for organ preservation. Esophageal embolization, for example, avoids a number of serious problems.
Varicose veins in older people
Why varicose veins more common in older people, and especially common in women?
1. To answer briefly - because their vascular system wears out with age and, sooner or later, fails. However, there are still many objective reasons why older women suffer from varicose veins more often than younger men and women. Firstly, since women generally live somewhat longer than men, there are correspondingly more elderly women than elderly men, and their veins have been working harder for a longer period of time.
2. Men don't get pregnant. Even if varicose veins that appeared in a woman during pregnancy disappear soon after the birth of the child, these veins were still abnormally enlarged within a few months. And with age, all the muscles of the human body, including the smooth muscles of the vascular walls, become less elastic than in youth. And the veins, which had already expanded once, during pregnancy, in old age again become a little wider than normal.
3. Nowadays, many women over the age of 30 are resorting to hormone replacement therapy, which was originally intended to relieve the unpleasant symptoms of menopause. There is no doubt that hormone replacement therapy helps women look younger, feel better, and generally cope with the menopause years more easily. Doctors' observations also confirm that hormone replacement therapy to some extent reduces the frequency of angina attacks and prevents a decrease in bone strength due to osteoporosis.
However, hormonal supplements at the same time soften the vein walls in the same way as increased levels of estrogen and progesterone during pregnancy. This side effect of hormonal pills is all the more dangerous because the walls of the veins are already becoming weaker - due to natural age-related changes in the muscle layer. So, additional clinical studies are needed to definitively clarify this issue.
Is varicose veins inherited?
Varicose veins are definitely hereditary. Scientists even believe that they have been able to isolate a separate gene responsible for the development of varicose veins. It is not yet clear whether this gene causes malformations of the venous valves or malformations of the vein walls themselves.
There is no doubt that these studies will help develop a gene therapy technique - perhaps the most promising way to prevent and treat varicose veins. Unfortunately, this is still a matter of the rather distant future, and gene therapy is not yet available to patients with varicose veins.