Low-density lipoproteins are the main carriers of cholesterol (cholesterol) in the body. The cholesterol they contain is considered “harmful”, since its excess increases the risk of plaques appearing in the arteries, which can lead to blockage and cause a heart attack or stroke.
Synonyms Russian
LDL, low-density lipoprotein, LDL, LDL-C, low-density lipoprotein cholesterol, beta-lipoprotein cholesterol, beta-lipoprotein, beta-LP.
English synonyms
LDL, LDL-C, low-density lipoprotein cholesterol, Low-density lipoprotein.
Research method
Colorimetric photometric method.
Units
mmol/l (millimoles per liter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress and do not smoke for 30 minutes before the test.
General information about the study
Cholesterol (CH, cholesterol) is a fat-like substance vital to the body. The correct scientific name for this substance is “cholesterol” (the ending -ol indicates that it belongs to alcohols), however, the name “cholesterol” has become widespread in the popular literature, which we will use later in this article. Cholesterol is involved in the formation of cell membranes of all organs and tissues of the body. Cholesterol is used to create hormones that are necessary for the development of the body and the reproduction function. Bile acids are formed from cholesterol, with the help of which fats are absorbed in the intestines.
Cholesterol is insoluble in water, so to move around the body it is “packed” into a protein shell consisting of apolipoproteins. The resulting complex (cholesterol + apolipoprotein) is called lipoprotein. Several types of lipoproteins circulate in the blood, differing in the proportions of their components:
- very low density lipoproteins (VLDL),
- low density lipoproteins (LDL),
- high density lipoproteins (HDL).
LDL cholesterol is considered “bad” because when it is in excess, plaques appear in the walls of blood vessels, which can restrict the movement of blood through the vessel, which threatens atherosclerosis and significantly increases the risk of heart disease (coronary artery disease, heart attack) and stroke.
The liver produces enough cholesterol for the body's needs, but some of it comes from food, mainly fatty meat and fatty dairy products. If a person has a genetic predisposition to high cholesterol or eats too much animal fat, LDL levels in the blood can rise to dangerous levels.
What is the research used for?
- To assess the likelihood of atherosclerosis and heart problems (this is the most important indicator of the risk of developing coronary disease).
- To monitor the effectiveness of a diet with a reduced amount of animal fats.
- To monitor lipid levels after taking cholesterol-lowering medications.
When is the study scheduled?
An LDL test is usually part of a lipid profile, which also includes the determination of total cholesterol, VLDL cholesterol, HDL cholesterol, triglycerides and atherogenicity coefficient. A lipidogram may be prescribed during routine preventive examinations or when the concentration of total cholesterol increases, in order to find out which fraction is responsible for the increase.
In general, a lipid profile is recommended for all people over 20 years of age at least once every 5 years, but in some cases even more often (several times a year). First, if the patient is prescribed a diet limited in animal fats and/or is taking cholesterol-lowering medications, then it is checked whether he achieves the target level of LDL and total cholesterol and, accordingly, whether his risk of cardiovascular disease is reduced diseases. And, secondly, if the patient has one or more risk factors for developing cardiovascular diseases in his life:
- smoking,
- certain age (men over 45, women over 55),
- high blood pressure (from 140/90 mm Hg),
- high cholesterol or cardiovascular disease in family members (heart attack or stroke in a close male relative under 55 years of age or a female relative under 65 years of age),
- coronary heart disease, previous myocardial infarction or stroke,
- diabetes,
- excess body weight,
- alcohol abuse,
- eating large amounts of food containing animal fats,
- low physical activity.
If a child in the family had cases of high cholesterol or heart disease at a young age, then it is recommended that he take a lipid profile for the first time between the ages of 2 and 10 years.
What do the results mean?
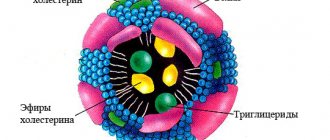
Reference values:
The concept of “normal” is not entirely applicable to the level of LDL cholesterol. Different people with different numbers of risk factors in their lives will have different LDL levels. LDL cholesterol testing is used to determine the risk of cardiovascular disease, but to accurately determine it for any person, all factors must be taken into account.
Elevated LDL cholesterol levels may be the result of a hereditary predisposition (familial hypercholesterolemia) or excess dietary intake of animal fats. In most people with high cholesterol, both factors are involved to some extent.
According to clinical guidelines1, the level
“Diagnostics and correction of lipid metabolism disorders for the purpose of prevention and treatment of atherosclerosis. Russian recommendations, VII revision. 2020".
"2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk."
Possible causes of elevated LDL cholesterol levels:
- cholestasis - stagnation of bile, which can be caused by liver disease (hepatitis, cirrhosis) or gallstones,
- chronic inflammation of the kidneys leading to nephrotic syndrome,
- chronic renal failure,
- decreased thyroid function (hypothyroidism),
- poorly treated diabetes mellitus,
- alcoholism,
- obesity,
- prostate or pancreatic cancer.
Reduced LDL cholesterol levels are not used in diagnosis due to low specificity. However, its reasons may be:
- hereditary hypocholesterolemia,
- severe liver disease,
- oncological diseases of the bone marrow,
- increased thyroid function (hyperthyroidism),
- inflammatory joint diseases,
- B12 or folate deficiency anemia,
- common burns,
- acute diseases, acute infections,
- chronic obstructive pulmonary disease.
What can influence the result?
Cholesterol concentrations may change from time to time, this is normal. A single measurement does not always reflect normal levels, so sometimes it may be necessary to retake the test after 1-3 months.
Increases very low-density lipoprotein cholesterol levels (VLDL cholesterol):
- pregnancy (lipid profile should be done at least 6 weeks after birth),
- long fasting,
- donate blood while standing,
- anabolic steroids, androgens, corticosteroids,
- smoking,
- eating food containing animal fats.
Reduce VLDL cholesterol levels:
- being in a lying position,
- allopurinol, clofibrate, colchicine, antifungal drugs, statins, cholestyramine, erythromycin, estrogens,
- intense physical activity,
- a diet low in cholesterol and saturated fatty acids and, conversely, high in polyunsaturated fatty acids.
Cholesterol-VLDL (calculated value: total cholesterol, HDL, LDL, triglycerides)
Cholesterol is a fat-like substance vital to the body. With its help, the formation of cell membranes of all organs and tissues of the body occurs. Hormones are created on the basis of cholesterol, which are involved in the growth, development of the body and the implementation of the reproduction function. In addition, bile acids, which are part of bile, are formed from cholesterol, thanks to which fats are absorbed in the intestines. Cholesterol is insoluble in water, so in order to move around the body it is “packed” into a shell consisting of special proteins - apolipoproteins. The resulting complex (cholesterol + apolipoprotein) is called lipoprotein. Several types of lipoproteins circulate in the blood, differing in the proportions of their components:
- very low density lipoproteins (VLDL),
- low density lipoproteins (LDL),
- high density lipoproteins (HDL).
Very low-density lipoprotein cholesterol is one of the most aggressive types of cholesterol. When there is an excess of VLDL cholesterol, it is deposited on the walls of blood vessels in the form of plaques, which can restrict the movement of blood through the vessel. In addition, they make blood vessels more rigid (atherosclerosis), which significantly increases the risk of heart disease (coronary artery disease, heart attack) and stroke. In addition, VLDL is the main carrier in the body of another type of fat - triglycerides. Elevated triglyceride levels also contribute to the development of atherosclerosis. The liver produces enough cholesterol and triglycerides for the body's needs, but some of these fats come from food, mainly meat and dairy products. If a person has a family history of high cholesterol and triglycerides or eats too much cholesterol-containing food, cholesterol levels in the blood can rise and cause harm to the body. What is analysis used for? A VLDL cholesterol test, along with other tests included in the lipid profile, is necessary in order to assess the risk of developing atherosclerosis and heart problems. Atherosclerosis is the process of plaque growth inside blood vessels, which can limit blood flow through the vessel or completely block its lumen. In addition, this study can be conducted to monitor the effectiveness of a diet with a reduced amount of animal fats and monitor blood lipid levels after the prescription of cholesterol-lowering drugs. When is the test scheduled? VLDL is usually included in the lipid profile, along with the determination of total cholesterol, LDL cholesterol, HDL cholesterol, triglycerides and atherogenicity coefficient. A lipidogram can be prescribed during routine preventive examinations or when total cholesterol is increased in order to find out what type of cholesterol is increasing. A lipidogram is recommended for all adults over 20 at least once every 5 years. It may be prescribed more often (several times a year) if a person is prescribed a diet limiting animal fats and/or is taking medications that lower cholesterol levels. In these cases, it is checked whether the patient has achieved the target level of lipid values and, accordingly, whether his risk of cardiovascular diseases is reduced.
Increased levels of VLDL cholesterol Increased concentrations of VLDL cholesterol may be the result of a hereditary predisposition (familial hypercholesterolemia) or excess dietary intake of animal fats. For most people with high cholesterol, both causes are involved to some extent. Other possible causes of increased VLDL:
- cholestasis - stagnation of bile, which can be caused by liver disease (hepatitis, cirrhosis) or gallstones,
- chronic inflammation of the kidneys leading to nephrotic syndrome,
- chronic renal failure,
- decreased thyroid function (hypothyroidism),
- poorly treated diabetes mellitus,
- alcoholism,
- obesity,
- prostate or pancreatic cancer.
Decrease in VLDL cholesterol levels
- A reduced level of LDL cholesterol has no particular clinical significance; it can be observed in the following conditions:
- hereditary hypocholesterolemia,
- severe liver disease,
- oncological diseases of the bone marrow,
- increased thyroid function (hyperthyroidism),
- inflammatory joint diseases,
- B12 or folate deficiency anemia,
- common burns,
- acute diseases, acute infections,
- chronic obstructive pulmonary disease.
What can influence the result? The amount of VLDL cholesterol can change from time to time, so a one-time measurement does not always reflect the “usual” cholesterol level. In this regard, it is sometimes necessary to re-take the test after 1-3 months. It happens that the level of VLDL cholesterol increases or decreases over a short period of time. This phenomenon is called biological variation and reflects normal fluctuations in cholesterol metabolism in the body. Increases VLDL cholesterol levels:
- pregnancy (lipid profile should be done at least 6 weeks after birth),
- long fasting,
- donate blood while standing,
- anabolic steroids, androgens, corticosteroids,
- smoking,
- eating food containing animal fats.
Reduce VLDL cholesterol levels:
- being in a lying position,
- allopurinol, clofibrate, colchicine, antifungal drugs, statins, cholestyramine, erythromycin, estrogens,
- intense physical activity,
- a diet low in cholesterol and saturated fatty acids and, conversely, high in polyunsaturated fatty acids.
The following contribute to an increased risk of developing cardiovascular diseases:
- smoking,
- age (men over 45 years old, women over 55 years old)
- increased blood pressure (140/90 mmHg and above),
- increased cholesterol or cardiovascular disease in other family members (heart attack or stroke in the closest male relative under 55 years of age, female under 65),
- coronary heart disease, previous myocardial infarction or stroke,
- diabetes,
- excess body weight,
- alcohol abuse,
- eating large amounts of food containing animal fats,
- low physical activity.
Low density lipoproteins
| Low-density lipoprotein (adapted from Encyclopedia Britanica) |
Low-density lipoproteins
(common abbreviations:
LDL
and
LNP
; English
low-density lipoprotein
, LDL) are a class of blood lipoproteins (also called lipoproteins), complex proteins consisting of apolipoproteins and lipids. They have a size from 18 to 25 nm and a density from 1.019 to 1.063 g/ml. LDL contains a single apolipoprotein molecule, apolipoprotein B-100, which stabilizes the structure of the LDL particle. The main function of LDL is to transport cholesterol (C) in the blood. Low-density lipoproteins are beta lipoproteins, which are the so-called “bad” lipoproteins. LDL is small enough to penetrate the artery wall. After oxidation, they easily linger in the walls of arteries, thus participating in the formation of atherosclerotic plaques, which narrow the lumen of blood vessels and promote thrombus formation.
Classification of levels and reference values of serum LDL cholesterol
The value of the target level of LDL cholesterol in the blood serum is currently debated.
The European Society of Cardiology (ESC) currently recommends a target LDL cholesterol level of less than 70 mg/dL (=1.8 mmol/L) for statin treatment in patients with coronary artery disease, but there are studies* suggesting that the target LDL cholesterol level is < 100 mg/dL provides the same degree of cardiovascular risk reduction as more aggressive target levels and reduces the risk of adverse events from lipid-lowering drugs. Recommendations of the third report of the expert group of the National Cholesterol Education Program, NCEP (Adult Treatment Panel III, ATP III):
| LDL cholesterol level | mg/dl | mmol/l |
| optimal | <100 | <2,6 |
| above optimal | 100-129 | 2,6-3,35 |
| borderline high | 130-159 | 3,36-4,13 |
| high | 160-189 | 4,14-4,94 |
| very tall | ≥190 | >4,95 |
Note.
Converting values in mg/dL to values in mmol/L: Y (in mg/dL) = Y (in mmol/L) x 0.0259. Reference values of LDL in blood plasma according to the INVITRO laboratory:
| Age, years | Floor | LDL cholesterol level, mmol/l |
| 5-10 | M | 1,63 — 3,34 |
| AND | 1,76 — 3,63 | |
| 10-15 | M | 1,66 — 3,44 |
| AND | 1,76 — 3,52 | |
| 15-20 | M | 1,61 — 3,37 |
| AND | 1,53 — 3,55 | |
| 20-25 | M | 1,71 — 3,81 |
| AND | 1,48 — 4,12 | |
| 25-30 | M | 1,81 — 4,27 |
| AND | 1,84 — 4,25 | |
| 30-35 | M | 2,02 — 4,79 |
| AND | 1,81 — 4,04 | |
| 35-40 | M | 2,10 — 4,90 |
| AND | 1,94 — 4,45 | |
| 40-45 | M | 2,25 — 4,82 |
| AND | 1,92 — 4,51 | |
| 45-50 | M | 2,51 — 5,23 |
| AND | 2,05 — 4,82 | |
| 50-55 | M | 2,31 — 5,10 |
| AND | 2,28 — 5,21 | |
| 55-60 | M | 2,28 — 5,26 |
| AND | 2,31 — 5,44 | |
| 60-65 | M | 2,15 — 5,44 |
| AND | 2,59 — 5,80 | |
| 65-70 | M | 2,54 — 5,44 |
| AND | 2,38 — 5,72 | |
| > 70 | M | 2,28 — 4,82 |
| AND | 2,49 — 5,34 |
* Leibowitz M. et al. Association Between Achieved Low-Density Lipoprotein Levels and Major Adverse Cardiac Events in Patients With Stable Ischemic Heart Disease Taking Statin Treatment // JAMA Intern Med. doi:10.1001/jamainternmed.2016.2751.
Methods for reducing the amount of LDL in the blood
To reduce LDL levels, a diet may be recommended aimed at reducing the intake of cholesterol and saturated fat and increasing the intake of high-protein foods, polyunsaturated and monounsaturated fats, fiber, as well as therapy with lipid-lowering drugs.
Currently, the main hypolipidemic drugs used to reduce con lipoproteins in the blood are considered to be structural inhibitors of the enzyme 3-hydroxy-3-methylglutaryl-acetyl-coenzyme A reductase, briefly “statins” (atorvastatin, cerivastatin, rosuvastatin, pitavastatin, etc.), ATX code C10AA. Statin therapy, among all possible methods for correcting lipid metabolism disorders, remains the only effective method for the primary prevention of ischemic stroke. The main goal of lipid-lowering therapy is to achieve target values of LDL cholesterol or the degree of reduction in its level.
If the patient does not respond to statin therapy, bile acid sequestrants (cholestyramine, etc.) may be prescribed, ATC code C10AC. In addition, fibrates (ATC code C10AB), nicotinic acid and its derivatives (ATC code C10AD), as well as other agents such as omega-3 triglycerides, policosanol, ezetimibe and others can be used. These drugs are prescribed as part of combination therapy or as monotherapy.
Long-term statin therapy lowers LDL but does not prolong life in elderly patients?
There are studies showing that when treated with statins (pravastatin, 40 mg per day) for 6 years in a large group of elderly patients with dyslipidemia and hypertension, but without clinical manifestations of cardiovascular disease (CVD), despite lowering LDL levels, There was no significant reduction in mortality compared with patients not taking statins, nor a reduction in the number of fatal and non-fatal cases of coronary heart disease.
Moreover, there was a trend towards increased all-cause mortality rates with statin use in the oldest age group. This study does not refute the fact that statins reduce the risk of CAD.** ** Han BH, et al. Effect of Statin Treatment vs Usual Care on Primary Cardiovascular Prevention Among Older Adults // JAMA Internal Medicine, 2021, doi:10.1001/jamainternmed.2017.1442.
ICD-10 and high levels of low-density lipoprotein
High levels of low-density lipoproteins in human blood in ICD-10 are classified as “Class IV. Diseases of the endocrine system, nutritional disorders and metabolic disorders (E00-E90)", block "E70-E90 Metabolic disorders", codes "E78.0 Pure hypercholesterolemia" and "E78.2 Mixed hyperlipidemia"
Medical service related to determining the level of low-density lipoproteins in human blood
Order of the Ministry of Health and Social Development of Russia No. 1664n dated December 27, 2011 approved the Nomenclature of Medical Services.
Section 9 of the Nomenclature provides for a medical service related to determining the level of low-density lipoproteins in human blood: “Study of the level of low-density lipoproteins,” service code A09.05.028. On the website GastroScan.ru in the “Literature” section there are subsections “Eating disorders and metabolic disorders, obesity, metabolic syndrome” and “Cardiovascular diseases associated with gastrointestinal diseases”, containing articles for healthcare professionals addressing these issues.
The results of studies of the level of low-density lipoproteins in the blood provide important information for the attending physician, but are not a diagnosis! Back to section
Blood lipid composition: interpretation and diagnosis
The content of various fats and their ratios in the blood is an important indicator of a person’s health. In some cases, it needs close monitoring, and sometimes correction. Let's figure out where the fats in the blood come from and how to keep track of them.
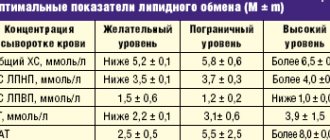
The role of fats in the body
The membranes of all cells in our body are a double lipid layer. Nerve fibers covered with a layer of myelin (a substance consisting of 75% fat) conduct impulses hundreds of times faster than “naked” fibers.
Without fats, fat-soluble vitamins D, E, K, A do not work (therefore, it is better to season carrot salad with vegetable oil). Hormones are built on the basis of the cholesterol molecule - sex hormones and glucocorticosteroids. And even the folds of fat on the body, from the point of view of nature, have a deep meaning: they are a shock absorber, insulation, and a reserve in case of hunger.
And at the same time, excess fat is a recognized risk factor for many diseases, from atherosclerosis to diabetes. Physical deposits of fat around and inside organs make them difficult to function. In addition, fat is a hormonally active substance, and its excess interferes with the functioning of the endocrine system, disrupting the balance.
The main fats that enter the body from the outside are triglycerides (neutral fats) and cholesterol. Triglycerides are used primarily as a storage substance and substrate for energy production. Cholesterol is the basis for the synthesis of steroid hormones, bile acids and vitamin D.
Types of lipoproteins in the blood
Fat cannot travel in the blood in the form of an ordinary drop, like in soup. Fats are transported in the body in the form of lipoproteins (LP) - compounds of fats and proteins. After absorption, fat molecules form conglomerates with protein molecules, and some of the proteins are a kind of label - the address to which fats must be delivered. The more protein there is in a lipoprotein, the higher its density will be.
If you take a blood test for a lipid profile (lipid spectrum), you will see the following names there:
- LDL
- low density lipoproteins. There are few proteins, a lot of fats, the direction of movement is from the liver to the tissues in which lipids should be used. - VLDL
is very low density lipoprotein. The ratio is shifted even more towards lipids, mainly “spare” ones, and these particles are sent to adipose tissue to replenish it. - HDL
is high density lipoprotein. These particles contain a lot of proteins, and they carry cholesterol “out” from the body - its excess will be eliminated through the liver. - TC
is total cholesterol, i.e. contained in all types of drugs in total. Every day, cholesterol comes from food, is produced by the body itself, and is excreted in bile. Therefore, there is the term “cholesterol balance” - 5.2–5.5 mmol/l in the blood. At this level, the risk of atherosclerosis is minimal, and there will be enough cholesterol to build all the necessary substances. - TG
is the sum of triglycerides in all medications.
Good, bad and too good
It seems that we need to fight to ensure that there are many PAPs and fewer of everyone else. Then cholesterol and triglycerides will move towards exit through the bile, and not towards accumulation in the form of atherosclerotic plaques and fat folds. In popular literature, HDL is often called “good cholesterol,” and LDL and VLDL are “bad” (although, strictly speaking, this is not exactly cholesterol).
Total cholesterol
The most important indicator of lipid metabolism.
Cholesterol (cholesterol)
- secondary monohydric cyclic alcohol. It is found in the blood and tissues of the body in free and esterified forms.
Free cholesterol
- a component of cellular plasma membranes, as well as membranes of mitochondria and the endoplasmic reticulum (in smaller quantities). Its esters predominate in blood serum. Cholesterol is a precursor to sex hormones, corticosteroids, bile acids, and vitamin D.
Up to 80% of cholesterol is synthesized in the liver, and the rest enters the body with products of animal origin (fatty meat, butter, eggs). Cholesterol is insoluble in water; its transport between tissues and organs occurs due to the formation of lipoprotein complexes.
Cholesterol fractions of low-density lipoproteins (LDL) and high-density lipoproteins (HDL) are isolated
, differing in composition and functions.
Cholesterol level
at birth below 3.0 mmol/l. With age, its level in the blood increases, and gender differences in concentration appear. In men, cholesterol levels increase in early and middle age and decrease in old age. In women, the concentration of cholesterol increases more slowly with age, until menopause, and can subsequently exceed the level of men. This is due to the action of sex hormones. Estrogens reduce, and androgens increase, total cholesterol levels.
Cholesterol accumulation is a risk factor for the development of atherosclerosis and coronary heart disease (CHD). A high risk of developing coronary artery disease in adults is a cholesterol concentration in the blood above 6.22 mmol/l. When the concentration of total cholesterol is in the range of borderline values and above, it is advisable to study cholesterol in combination with the determination of triglycerides, HDL and LDL cholesterol.
Cholesterol-HDL (High Density Lipoprotein Cholesterol)
A fraction of lipoproteins responsible for the transfer of cholesterol from peripheral cells to the liver.
Lipoproteins in the blood
transport lipids, including cholesterol, from one cell population to another. Unlike other lipoproteins, HDL transports cholesterol from cells of peripheral organs (including heart vessels, brain arteries, etc.) to the liver, where cholesterol is converted into bile acids and excreted from the body.
On average, women have higher HDL levels than men. A decrease in HDL cholesterol concentrations below 0.90 mmol/L for men and below 1.15 mmol/L for women, as well as a ratio of low-density lipoprotein cholesterol to high-density lipoprotein cholesterol greater than 3:1 are associated with an increased risk of atherosclerosis.
Elevated levels of HDL cholesterol are considered to be an antiatherogenic factor.
Triglycerides
The main blood lipids, which are the main source of energy for cells.
They enter the body with food and are also synthesized by cells of adipose tissue, liver, and intestines. They do not circulate freely, but are bound to proteins and transported in the form of macromolecular complexes - lipoproteins. They are the main lipids of fatty deposits and food products. The triglyceride molecule contains triatomic glycerol and 3 residues of higher fatty acids, mainly palmitic, stearic, linoleic and oleic.
The main source of energy for cells. Triglycerides accumulate in fat cells, from where, after hydrolysis, they are broken down into glycerol and fatty acids and released into the circulation system.
The level of this indicator in the blood changes with age.
Hyperlipoproteinemia - symptoms and treatment
Diet
If the patient has no symptoms, then treatment begins with a special diet.
Correction of nutrition can reduce cholesterol levels by 5–10%. Recommended:
- Eat less animal fat (up to 30% of daily calories).
- Include vegetable oils in your diet: sunflower, olive and cottonseed (up to 25–30 mg per day). They are a source of polyunsaturated fatty acids, which normalize cholesterol metabolism.
- Eat fewer foods rich in cholesterol: liver, kidneys, brains, fatty meats, egg yolks, mayonnaise, fatty sauces.
- Do not fry the meat, but boil it, but avoid very rich broths.
- Eat no more than 40–50 g of sugar per day, limit consumption of sweets, cakes, pastries, sugary drinks and fruit nectars. Excess sugar contributes to the development of atherosclerosis.
- Drink freshly squeezed juices from apples, oranges and carrots 1-2 times a week.
- Do not indulge in strong tea and coffee, as they can increase blood pressure, cause palpitations and insomnia.
- Eat no more than 3–5 g of salt per day.
- There are more vegetables, fruits, cereals (especially rolled oats) and wholemeal products.
- Eat fish twice a week, steaming or grilling it.
- Season salads with olive oil, lemon juice, herbs and spices [3].
It is important to remember that cholesterol not only comes from outside, but is also formed in the body. Therefore, you should not completely give up foods containing fats.
Drug treatment
For cardiovascular diseases, diabetes mellitus, chronic kidney disease and a high risk on the SCORE scale, cholesterol-lowering medications are indicated. However, in some cases, patients even at moderate risk may require drug therapy. It will help reduce the likelihood of developing atherosclerosis.
To correct the level of atherogenic lipids, drugs are taken for a long time, most often for life. When LDL levels are reduced, the risk of cardiovascular disease decreases by 30–40% [9].
Groups of drugs for the treatment of hyperlipoproteinemia:
- statins;
- fibrates;
- inhibitors of cholesterol absorption in the intestine;
- bile acid sequestrants;
- PCSK9 enzyme inhibitors;
- n-3 fatty acids [8].
Statins
Statins (Atorvastatin, Rosuvastatin, Pitavastatin) are the most effective drugs for lowering cholesterol. They block the enzyme that is involved in its formation and thereby suppress the production of cholesterol in the liver. Statins reduce low-density lipoprotein (LDL) and triglycerides (TG).
Statins prevent the development of atherosclerosis of the coronary and cerebral arteries, and with long-term use they reduce the size of plaques in the vessels. These drugs are necessary for patients with hyperlipoproteinemia and atherosclerosis for the prevention of myocardial infarction and stroke.
Before you start taking statins, it is necessary to determine the lipid profile, and also check the condition of the liver based on the content of liver enzymes (ASAT, ALAT) in the blood. Statins are used in safe dosages until target LDL levels are achieved. The dosage depends on the patient's cardiovascular risk.
To assess the safety and effectiveness of the prescribed dose, a month after starting treatment, it is necessary to re-test the lipid profile, AST and ALAT. The effect appears within the first week from the start of treatment. After two weeks it is 90% of the maximum effect. The greatest effect is achieved by the fourth week and then remains constant.
If the target LDL level is reached and the drug does not adversely affect the liver, then the statin at this dosage is used for a long time. The lipid profile, ASAT and ALAT are monitored every 3–6 months. When liver enzymes increase above three norms, the drug is no longer used.
Target levels for lowering LDL cholesterol depend on cardiovascular risk [7].
| Cardiovascular risk | Lower LDL |
| High | ≥ 50% of baseline to 1.4 mmol/l |
| Moderate | 2.6 mmol/l |
| Short | 3.0 mmol/l |
In addition to lowering cholesterol, statins have a positive effect on the condition of the inner lining of the arteries, stabilize atherosclerotic plaques and improve blood flow.
Statins are generally well tolerated, but some patients experience side effects such as muscle pain. The drugs should be taken under the constant supervision of a doctor, their dose should be adjusted in a timely manner or used in combination with other medications.
Fibrates
Fibrates (Fenofibrate) stimulate the activity of the enzyme lipoprotein lipase and thereby accelerate the breakdown of lipoproteins. They reduce not only cholesterol, but also triglycerides (TG). These are the drugs of choice for patients with diabetes, who most often have elevated TG.
Inhibitors of cholesterol absorption in the intestine
Cholesterol absorption inhibitors (Ezetimibe) are used as second-line therapy in combination with statins. They are prescribed if it is not possible to reduce lipoprotein levels to target levels, as well as if it is impossible to take statins [5].
Bile acid sequestrants
Sequestrants (Cholestyramine, Colestipol) are ion exchange resins that prevent bile acids from being absorbed in the intestine. Depletion of these acids activates their synthesis from cholesterol in the liver. Used in patients with cholestasis.
Taking drugs in this group often causes side effects: flatulence, stool retention, nausea, pain or discomfort in the upper abdomen, which limits their use.
Monoclonal antibodies
PCSK9 inhibitors (Alirocumab, Evolocumab) are monoclonal antibodies that bind to LDL receptors in the liver and stimulate the breakdown of lipoproteins. They are administered subcutaneously, usually once every 2 weeks or once a month, depending on the drug. Prescribed to patients with a very high risk of cardiovascular disease and when it is impossible to take statins [7].
N-3 fatty acids
To reduce the level of triglycerides and lipoproteins (especially VLDL), you can take eicosapentaenoic acid and docosahexaenoic acid. The exact dosage is determined by the doctor [8].
It is important to prescribe lipid-lowering therapy on time to prevent the development of atherosclerosis and its complications.