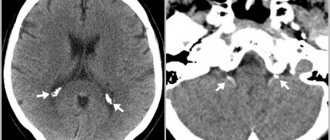
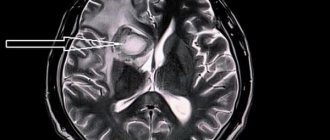
Cerebral infarction or ischemic stroke are both names for a stroke caused by a blockage of a blood vessel in a person's brain.
This is the most common type of stroke among Russians, Ukrainians and Belarusians. A blood clot or fatty plaque forms in the patient's brain and blocks a blood vessel - an embolus.
This is focal necrosis of the brain caused by complete and prolonged ischemia, which affects all tissue elements, neurons, glia and blood vessels.
Ischemic infarctions cause focal neurological deficits in the patient. With embolic infarctions they appear abruptly. In atherothrombotic infarctions, they develop over a period of time, usually several hours. Atherothrombotic infarctions are often preceded by transient ischemic attacks (TIAs).
A TIA is a focal neurological deficit that lasts less than 24 hours and resolves.
Symptoms of cerebral infarction
Symptoms of a cerebral infarction depend on where the lesion is located.
However, general symptoms of this pathological process can be identified, including:
- Headache;
- Loss of consciousness, sometimes coma may develop;
- Dizziness;
- Disturbances in the functioning of the pelvic organs;
- Pain in the eyeballs;
- Feeling hot;
- Dry mouth;
- Nausea and vomiting accompanied by severe headache;
- Convulsions (not always present).
If the focus of a cerebral infarction is localized in the right hemisphere, then the following clinical picture is characteristic:
- Complete immobility (hemiparesis) or significant decrease in strength (hemiplegia) of the left limbs;
- Sensitivity in the left half of the body and face disappears or sharply decreases;
- Speech impairment will be observed in left-handed people. In right-handed people, speech disorders develop exclusively when the left hemisphere is damaged. The patient cannot reproduce words, but conscious gestures and facial expressions are preserved;
- The face becomes asymmetrical: the left corner of the mouth goes down, the nasolabial fold is smoothed out.
Depending on which half of the brain is damaged, symptoms of a cerebral infarction will be observed on the opposite side. That is, if the lesion is located in the left hemisphere, then the right half of the body will suffer.
If a cerebral infarction develops in the vertebrobasilar vascular system, then the patient’s symptoms are as follows:
- Dizziness that increases when you tilt your head back;
- Coordination suffers, static disorders are observed;
- There are disturbances in the movement of the eyeballs, vision deteriorates;
- A person pronounces individual letters with difficulty;
- Problems with swallowing food appear;
- Speech becomes quiet, hoarseness appears in the voice;
- Paralysis, paresis, and loss of sensation in the limbs will be observed on the side opposite to the lesion.
It is worth considering separately the symptoms of cerebral infarction depending on which cerebral artery is damaged:
- Anterior cerebral artery – incomplete paralysis of the legs, the occurrence of grasping reflexes, impaired eye movements, motor aphasia;
- Middle cerebral artery – incomplete paralysis and sensitivity disorder of the hands, as well as the lower half of the face, sensory and motor aphasia, laterofixation of the head;
- Posterior cerebral artery – visual disturbances, the patient understands the speech of another person, can speak himself, but he forgets most words.
In severe cases, consciousness is depressed and the person falls into a coma, which can occur when any part of the brain is damaged.
Artificial nutrition for ischemic stroke
Artificial nutrition is carried out enterally (while maintaining, to one degree or another, the movement of nutrients through the gastrointestinal tract) and parenterally.
The main elements of parenteral nutrition are water, sources of nitrogen and energy. As sources of nitrogen, specialists at the Yusupov Hospital use synthetic amino acid mixtures containing adequate and balanced amounts of nonessential and essential amino acids. Of the synthetic amino acid mixtures, the following drugs are most often used:
- azonutril;
- aminosteryl;
- Vamin;
- polyamine;
- Freamin.
The solutions ensure the synthesis of proteins from the administered amino acids, have a pronounced positive effect on protein metabolism, lead to a positive nitrogen balance and stabilization of the patient’s body weight. Amino acid mixtures remove toxins from the body by reducing the concentration of ammonia, which binds to the formation of non-toxic breakdown products.
Doctors at the Yusupov Hospital provide the amount of energy needed by patients with ischemic stroke through carbohydrates or a combination of fat emulsions and monosaccharide solutions (lipofundin, intralipid). For enteral nutrition of patients with ischemic stroke at the Yusupov Hospital, polymer or elemental mixtures are used. Polymer mixtures contain fats, proteins and carbohydrates in proportions typical of a normal human diet. They consist of the following ingredients:
- whole protein isolates (milk, soy, meat, eggs);
- partially hydrolyzed starch;
- triglycerides;
- the necessary set of vitamins, micro- and macroelements.
Before absorption, these mixtures undergo enzymatic treatment in the intestines. Elemental mixtures contain:
- amino acids or short peptides;
- dextrose and oligosaccharides;
- essential fatty acids and medium chain triglycerides.
They are administered to patients if it is impossible to use polymer mixtures due to a pronounced decrease in the absorption and digestive functions of the intestine. The Yusupov Hospital also widely uses specific biologically significant elements that purposefully correct metabolic disorders such as:
- glutamine;
- branched amino acids;
- arginine;
- taurine;
- nucleic acids;
- microelements;
- antioxidants;
- vitamins.
In severe ischemic stroke, the inclusion of antioxidants in the enteral nutrition regimen provides better control over the increase in metabolism and reduces the time required for compensation of internal toxicosis. Doctors at the Yusupov Hospital for stroke prefer early enteral nutrition as it is more physiological and easier to administer. Early enteral nutrition can solve the problem of “empty intestines.”
The movement of food through the gastrointestinal tract maintains the normal state and composition of the intestinal microflora. By prescribing artificial enteral nutrition to a patient with an ischemic stroke who is unable to feed on his own, doctors at the Yusupov Hospital prevent the occurrence of septic complications associated with the penetration of microorganisms from the intestines into the blood.
Causes of cerebral infarction
The following causes of cerebral infarction are distinguished:
- Atherosclerosis. It develops in men earlier than in women, since at a young age female blood vessels are protected from atherosclerotic lesions by sex hormones. The coronary arteries are the first to be affected, then the carotid ones, and subsequently the cerebral blood supply system;
- Hypertension. Mild hypertension (pressure up to 150/100 mm Hg), which is the most dangerous, enhances atherosclerosis and disrupts the adaptive reactions of the arteries;
- Heart diseases. Thus, people who have had a myocardial infarction have a high risk of developing a cerebral infarction. In 8% of patients after myocardial infarction, ischemic stroke will develop within the first month, and in 25% of patients - within six months. Coronary heart disease and heart failure are also dangerous;
- High blood viscosity;
- Atrial fibrillation. They cause blood clots to form in the left atrial appendage, which are subsequently transported to the brain;
- Disorders of the endocrine system, primarily diabetes mellitus;
- Vascular diseases (pathologies of their development, Takayasu's disease, anemia, leukemia, malignant tumors).
In addition, do not forget about risk factors that increase the likelihood of a cerebral infarction, including:
- Age (every ten years of life increases the risk of developing cerebral infarction by 5-8 times);
- Hereditary predisposition;
- Physical inactivity;
- Excess weight;
- Smoking (if this bad habit is supplemented by taking oral contraceptives, then smoking becomes a leading risk factor for the development of cerebral infarction);
- Alcohol abuse;
- Acute stress or prolonged psycho-emotional stress.
Features of the clinical picture of brainstem ischemic stroke
Brainstem ischemic stroke is the most severe localization of acute cerebrovascular accident, which is due to the presence of nearby vital nerve centers. Brainstem ischemia is not always fatal, and the likelihood of full recovery and return to your previous life depends on many factors:
- size of the stroke focus;
- patient's age;
- presence of concomitant diseases.
Often, an ischemic brainstem stroke develops suddenly and is accompanied by “locked-in man” syndrome, that is, paralysis of the entire body. The patient retains intellectual qualities and understands what is happening. 60% of patients with a stroke in the brain stem die within two days. A more favorable prognosis with timely medical care and in young patients. Doctors at the Yusupov Hospital often manage to preserve lost functions, but restoring motor functions requires a lot of effort and time.
Consequences of cerebral infarction
The consequences of a cerebral infarction can be very serious and often pose a direct threat to human life, among them are:
- Brain swelling. It is this complication that develops more often than others and is the most common cause of death of a patient in the first week after an ischemic stroke;
- Congestive pneumonia is the result of the patient being in a horizontal position for a long time. It most often develops 3-4 weeks after a cerebral infarction;
- Pulmonary embolism;
- Acute heart failure;
- Bedsores due to the patient lying motionless in bed for a long time.
In addition to the listed consequences of cerebral infarction, which develop in the early stages, long-term complications can also be identified, including:
- Impaired motor function of the limbs;
- Decreased sensation in the arms, legs and face;
- Speech problems;
- Deterioration of mental abilities;
- Mental disorders;
- Difficulty swallowing food;
- Coordination problems when walking and turning;
- Epileptic seizures (up to 10% of people who have had a cerebral infarction are susceptible to them);
- Malfunctions of the pelvic organs (bladder, kidneys, intestines, reproductive organs suffer).
Signs of ischemic stroke of the brain stem
Main symptoms of brainstem ischemic stroke
- coordination of movements is impaired;
- dizziness (a feeling of movement or spinning);
- 30% of patients experience speech impairment, it becomes slurred and quiet;
- 65% of patients have problems swallowing;
- spontaneous uncontrolled movements of the legs and arms, mobility of the limbs is significantly reduced;
- breathing slows down, often patients cannot breathe on their own;
- blood pressure increases;
- the pulse becomes too rare or frequent,
- thermoregulation is disrupted - body temperature either sharply decreases or increases;
- control over spontaneous eye movements is lost, which leads to the development of strabismus and loss of the ability to focus on an object.
At the onset of brainstem ischemic stroke, its first manifestations may be impaired coordination of movements and unsteadiness when walking. Patients can move around and complain that they are suddenly forced to walk while holding onto the wall. After suffering a brainstem ischemic stroke, they still have consequences in the form of impaired swallowing - patients can only swallow soft food.
What is the difference between a cerebral infarction and a stroke?
When a cerebral infarction occurs, the blood supply to the brain is disrupted, as a result of which the tissues of the affected area begin to die. Insufficient blood flow to the brain occurs due to atherosclerotic plaques that prevent its normal flow, due to heart rhythm disturbances, or due to problems with the blood coagulation system.
With a hemorrhagic stroke of the brain, on the contrary, the blood flow to it increases, which causes an artery rupture. The cause is vascular pathologies or hypertensive crisis.
There are differences in the course of the disease. Thus, cerebral infarction develops gradually, over several hours or even days, and hemorrhagic stroke occurs almost instantly.
Causes of changes in metabolism during ischemic stroke
In patients with ischemic stroke, the digestive, respiratory, cardiovascular and urinary systems are most quickly involved in the pathological process, and multiple organ failure develops. During a stroke, the central regulatory organ suffers, which leads to a breakdown of central neurogenic control over the processes occurring in the internal organs.
Metabolic changes during stroke occur both as a result of powerful sympathetic stimulation of hormone release (glucagon, catecholamines, corticosteroids) and under the influence of local mediators. As a result of this reaction, the metabolism changes so that the body can absorb nutrients in the face of severe illness. This allows the mobilization of energy and substrates to support inflammatory and immune responses, as well as tissue regeneration. With ischemic stroke, protein deficiency develops, which ultimately leads to disruption of cell function and structure, as well as organ function.
In conditions of increased metabolism, an important role in the complex intensive care of ischemic stroke belongs to ensuring adequate nutrition using a number of methods other than regular food intake. A significant proportion of patients with ischemic cerebral stroke are unable to eat on their own, which is associated with a decreased level of consciousness or impaired swallowing function. Often the only possible way to deliver nutrients to these patients is artificial nutrition.