Hypotensive effect - what is it? This question is asked by women and men who are faced with the problem of high blood pressure or hypertension for the first time and who have no idea what the hypotensive effect of the drugs prescribed to them by their attending physician means. An antihypertensive effect is a decrease in blood pressure under the influence of a particular drug.
Experienced professional therapists of the highest category at the Yusupov Hospital Therapy Clinic, who are proficient in advanced treatment and diagnostic methods, will provide qualified assistance to patients with arterial hypertension and select an effective treatment regimen that eliminates the development of negative consequences.
Hypotensive syndrome
Hypotensive syndrome is a whole complex of symptoms that reflects a persistent decrease in intracranial pressure in women. It occurs only in pregnant women aged 25 to 29 years. This syndrome significantly reduces the quality of life of the expectant mother and requires qualified medical care.
Make an appointment
Causes
The causes of this pathology are the following factors:
- severe dehydration after undergoing drug therapy;
- head injuries;
- leakage of cerebrospinal fluid due to a violation of the integrity of the skull bones or brain tissue;
- a decrease in blood pressure, leading to a decrease in intracranial pressure.
Every pregnant woman should be doubly attentive to her health, since she is also responsible for the life of the child. Any changes in health should be a reason to consult a doctor. Doctors at the Yusupov Hospital are ready to answer all their patients’ questions at any time, either in person or by phone.
Symptoms of hypotensive syndrome in pregnant women are:
- severe constricting sudden headaches;
- increased headaches when raising the head or in a sitting position;
- reduction in the intensity of headaches when lowering the head;
- prostration;
- feeling drowsy;
- irritability;
- attacks of nausea and vomiting.
Of course, many of the above symptoms occur in pregnant women and are a consequence of changes in the functioning of all organs and systems during the period of bearing a baby. They may have nothing to do with hypotensive syndrome.
But in any case, if the expectant mother’s health worsens, she must inform the doctor about it. Caution and attentiveness to your health will help you avoid the development of complications, identify hypotensive syndrome and undergo an effective course of therapy.
Diagnostics
If symptoms of the disease appear during pregnancy, it is necessary to undergo examinations by a gynecologist, neurologist and neurosurgeon. Doctors conduct examinations, analyze all the patient’s complaints and make a preliminary diagnosis. To confirm or refute it, the pregnant woman is prescribed a number of diagnostic measures, namely:
- general and biochemical blood test;
- general urine analysis;
- X-ray of the skull;
- spinal tap;
- MRI of the brain.
At the Yusupov Hospital, all diagnostic procedures are carried out using modern medical equipment, which allows you to obtain accurate data and promptly begin treatment.
Gestational diabetes mellitus
Author of the article: Baimuradova Seda Mayrabekovna, obstetrician-gynecologist, specialist in the field of hemostasis, MD.
Gestational diabetes is an increase in blood glucose (sugar) levels that was first detected during pregnancy.
Diabetes mellitus during pregnancy can negatively affect the development of the fetus. If it occurs in the early stages of pregnancy, the risk of miscarriage increases, and, even worse, the appearance of congenital malformations in the baby. Most often the most important organs of the baby are affected - the heart and brain.
Gestational diabetes, which begins in the second or third trimesters of pregnancy, causes excessive growth of the fetus. This leads to hyperinsulinemia: after childbirth, when the baby no longer receives as much glucose from the mother, his blood sugar levels drop to very low levels.
If this disease is not identified and treated, it can lead to the development of diabetic fetopathy - a complication in the fetus that develops due to a violation of carbohydrate metabolism in the mother's body.
Signs of diabetic fetopathy in a child:
- large sizes (weight more than 4 kg);
- violation of body proportions (thin limbs, large belly);
- swelling of tissues, excess deposits of subcutaneous fat;
- jaundice;
- respiratory disorders;
- hypoglycemia of newborns, increased blood viscosity and the risk of blood clots, low levels of calcium and magnesium in the blood of the newborn.
During pregnancy, a woman’s body experiences not just a hormonal surge, but a whole hormonal storm, and one of the consequences of such changes is a violation of the body’s tolerance to glucose - in some it is stronger, in others it is weaker. What does this mean? Blood sugar levels are high (above the upper limit of normal), but not high enough to warrant a diagnosis of diabetes.
In the third trimester of pregnancy, as a result of new hormonal changes, gestational diabetes may develop. The mechanism of its occurrence is as follows: the pancreas of pregnant women produces 3 times more insulin than other people - in order to compensate for the effect of specific hormones on the level of sugar contained in the blood.
If it does not cope with this function with increasing concentrations of hormones, then a phenomenon such as gestational diabetes mellitus occurs during pregnancy.
There are certain risk factors that increase the likelihood that a woman will develop gestational diabetes during pregnancy. However, the presence of even all these factors does not guarantee that diabetes will still occur - just as the absence of these unfavorable factors does not guarantee 100% protection from this disease.
- Excess body weight observed in a woman even before pregnancy (especially if the weight exceeded the norm by 20% or more);
- Nationality. It turns out that there are certain ethnic groups in which gestational diabetes is much more common than in others. These include blacks, Hispanics, Native Americans and Asians;
- High sugar level based on urine test results;
- Impaired body tolerance to glucose (as we have already mentioned, the sugar level is higher than normal, but not so much as to make a diagnosis of diabetes);
- Heredity. Diabetes is one of the most serious hereditary diseases, and your risk increases if someone close to you on your side was diabetic;
- Previous birth of a large (over 4 kg) child;
- Previous birth of a stillborn child;
- You have already been diagnosed with gestational diabetes during a previous pregnancy;
- Polyhydramnios, that is, too much amniotic fluid.
If you find yourself with several signs that are at risk, tell your gynecologist about this - you may be prescribed additional examination. If nothing wrong is found, you will undergo another test along with all the other women. All others are screened for gestational diabetes between 24 and 28 weeks of pregnancy.
How would this happen? You will be asked to do a test called an “oral glucose tolerance test.” You will need to drink a sweetened liquid containing 50 grams of sugar. After 20 minutes there will be a less pleasant stage - taking blood from a vein. The fact is that this sugar is quickly absorbed, within 30-60 minutes, but individual indications vary, and this is what interests doctors. In this way, they find out how well the body is able to metabolize the sweet solution and absorb glucose.
If in the form in the “analysis results” column there is a figure of 140 mg/dL (7.7 mmol/L) or higher, this is already a high level. You will be given another test, but this time after fasting for several hours.
After diagnosis follows treatment:
- Controlling blood sugar levels. This is done 4 times a day - on an empty stomach and 2 hours after each meal. Additional checks may also be needed - before meals;
- Urine tests. Ketone bodies should not appear in it - they indicate that diabetes is not controlled;
- Follow a special diet that your doctor will tell you. We will consider this issue below;
- Reasonable physical activity on the advice of a doctor;
- Body weight control;
- Insulin therapy as needed. At the moment, only insulin is allowed to be used as an antidiabetic drug during pregnancy;
- Blood pressure control.
Diet for gestational diabetes mellitus
If you are diagnosed with gestational diabetes, you will have to reconsider your diet - this is one of the conditions for successful treatment of this disease. It is usually recommended to reduce body weight in diabetes (this contributes to increased insulin resistance), but pregnancy is not the time to lose weight, because the fetus must receive all the nutrients it needs. This means that you should reduce the calorie content of food without reducing its nutritional value.
1. Eat small meals 3 times a day and have another 2-3 snacks at the same time. Don't skip meals! Breakfast should consist of 40-45% carbohydrates, the last evening snack should also contain carbohydrates, approximately 15-30 grams.
2. Avoid fried and fatty foods, as well as foods rich in easily digestible carbohydrates. These include, for example, confectionery, as well as baked goods and some fruits (banana, persimmon, grapes, cherries, figs). All these products are quickly absorbed and cause a rise in blood sugar levels; they contain few nutrients, but are high in calories. In addition, to neutralize their high glycemic effect, too much insulin is required, which is an unaffordable luxury for diabetes.
3. If you feel sick in the morning, keep a cracker or dry salty cookie on your bedside table and eat a few before getting out of bed. If you are treated with insulin and feel sick in the morning, make sure you know how to deal with low blood sugar.
4. Don't eat fast food. They undergo industrial pre-processing to reduce their preparation time, but their effect on increasing the glycemic index is greater than that of their natural counterparts. Therefore, exclude from your diet freeze-dried noodles, “5-minute” soup from a bag, instant porridge, and freeze-dried mashed potatoes.
5. Pay attention to foods rich in fiber: porridge, rice, pasta, vegetables, fruits, whole grain bread. This is true not only for women with gestational diabetes - every pregnant woman should eat 20-35 grams of fiber per day. Why is fiber so good for diabetics? It stimulates the intestines and slows down the absorption of excess fat and sugar into the blood. Fiber-rich foods also contain many essential vitamins and minerals.
6. Saturated fats in the daily diet should not exceed 10%. And in general, eat less foods containing “hidden” and “visible” fats. Eliminate sausages, sausages, sausages, bacon, smoked meats, pork, and lamb. Lean meats are much preferable: turkey, beef, chicken, and fish. Remove all visible fat from meat: lard from meat, and skin from poultry. Prepare everything in a gentle way: boil, bake, steam.
7. Cook food not in fat, but in vegetable oil, but there should not be too much of it.
8. Drink at least 1.5 liters of liquid per day (8 glasses).
9. Your body does not need fats such as margarine, butter, mayonnaise, sour cream, nuts, seeds, cream cheese, sauces.
10. Tired of prohibitions? There are also foods that you can eat without restrictions - they contain few calories and carbohydrates. These are cucumbers, tomatoes, zucchini, mushrooms, radishes, zucchini, celery, lettuce, green beans, cabbage. Eat them in main meals or as snacks, preferably in the form of salads or boiled (boiled in the usual way or steamed).
11. Make sure your body is provided with all the vitamins and minerals needed during pregnancy: ask your doctor if you need additional vitamins and minerals.
If diet therapy does not help, and blood sugar remains high, or if ketone bodies are constantly detected in the urine at normal sugar levels, you will be prescribed insulin therapy.
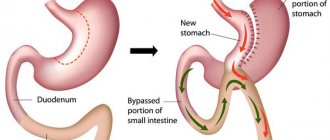
Insulin is only injected because it is a protein, and if you try to put it into tablets, it will be completely destroyed by our digestive enzymes.
Disinfectants are added to insulin preparations, so do not wipe the skin with alcohol before injection - alcohol destroys insulin. Naturally, you need to use disposable syringes and observe personal hygiene rules. Your doctor will tell you all the other details of insulin therapy.
Engage in familiar types of active activities that you like and bring pleasure: walking, gymnastics, exercises in the water.
After childbirth, gestational diabetes usually goes away - it develops into diabetes mellitus only in 20-25% of cases. True, the birth itself may be complicated due to this diagnosis. For example, due to the already mentioned overfeeding of the fetus, the child may be born very large.
Many might want a “hero,” but the large size of the child can be a problem during labor and childbirth: in most such cases, a cesarean section is performed, and in the case of natural delivery there is a risk of injury to the child’s shoulders.
With gestational diabetes, babies are born with low blood sugar, but this can be corrected simply by feeding. If there is no milk yet, and the child does not have enough colostrum, the child is fed with special formulas to raise the sugar level to normal. Moreover, the medical staff constantly monitors this indicator, measuring glucose levels quite often, before feeding and 2 hours after.
As a rule, no special measures are needed to normalize the blood sugar level of the mother and child: in the child, as we have already said, sugar returns to normal thanks to feeding, and in the mother - with the release of the placenta, which is an “irritating factor”, since produces hormones. The first time after giving birth, you will still have to monitor your diet and periodically measure your sugar levels, but over time everything should return to normal.
There is no 100% guarantee that you will never encounter gestational diabetes - it happens that women who, by most indicators, fall into the risk group, do not get sick when they become pregnant, and vice versa, this disease happens to women who, it would seem, did not have no prerequisites.
If you already had gestational diabetes during a previous pregnancy, it is very likely to return. However, you can reduce your risk of developing gestational diabetes during pregnancy by maintaining a healthy weight and not gaining too much during those 9 months. Physical activity will also help maintain your blood sugar at a safe level, provided that it is regular and does not cause you discomfort.
You also remain at risk of developing a permanent form of diabetes, type 2 diabetes. You will have to be more careful after childbirth. Therefore, it is not advisable for you to take drugs that increase insulin resistance: nicotinic acid, glucocorticoid drugs (these include, for example, dexamethasone and prednisolone).
Antihypertensive therapy for diabetes mellitus
Diabetes mellitus is a chronic disease, the development of which is associated with an absolute or relative deficiency of the hormone insulin. Lack of insulin or lack of sensitivity to it leads to an increase in blood glucose levels. This condition has a negative impact on all systems and organs of the human body, including the cardiovascular system.
Almost all patients suffering from diabetes complain of high blood pressure, which can be reduced with great difficulty without the help of a doctor.
Hypertension and diabetes mellitus
Hypertension in patients with diabetes is an integral and very dangerous component, which can several times increase the risk of developing the following diseases:
- 3-5 times - heart attack;
- 3-4 times - stroke:
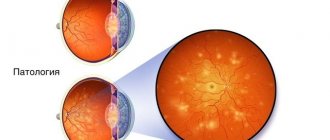
- 10-20 times - blindness;
- 20-25 times – renal failure;
- 20 times - gangrene, requiring limb amputation.
If blood pressure readings exceed 140/90, there is no need to hesitate to contact a specialist, since hypertension that occurs against the background of diabetes mellitus can lead to the development of irreversible consequences, often incompatible with life.
Hypertension in type 1 diabetes mellitus
The main and most dangerous cause of arterial hypertension in type 1 diabetes mellitus is the presence of diabetic nephropathy in patients with this disease. The development of this complication is observed in almost 40% of people suffering from type 1 diabetes. Increased blood pressure is directly related to the amount of protein excreted in the urine.
Hypertension due to renal failure also develops due to poor excretion of sodium in the urine. As sodium increases in the blood, fluid accumulates to dilute it. Due to the increase in circulating blood volume, blood pressure increases. This process may also be associated with an increase in glucose concentration, which occurs in diabetes mellitus. As a result, to reduce blood density, the body produces even more fluid and the volume of circulating blood further increases for this reason.
Hypertension in type 2 diabetes mellitus
One of the factors that provokes the development of type 2 diabetes mellitus is insulin resistance, i.e. decreased sensitivity of tissues to the action of insulin.
To compensate for insulin resistance, excessive amounts of insulin circulate in the blood, which itself causes an increase in blood pressure. Over time, a narrowing of the lumen of blood vessels occurs, caused by atherosclerosis, which also contributes to the occurrence of hypertension. In parallel, patients experience the development of abdominal obesity, and, as is known, it is from adipose tissue that substances that increase blood pressure are released into the blood.
Hypertension in diabetes: features
In patients with diabetes mellitus, there is a disturbance in the natural daily rhythm of blood pressure fluctuations. In a healthy person, blood pressure levels in the morning and at night are usually 10-20% lower than in the daytime. In patients with diabetes, there is no decrease in blood pressure at night. Moreover, their nighttime pressure readings may be even higher than their daytime ones. According to experts, this phenomenon is caused by diabetic neuropathy. An increased concentration of sugar in the blood leads to damage to the autonomic nervous system, which is responsible for regulating the body's vital functions. There is a deterioration in the ability of blood vessels to regulate their tone - narrowing and relaxing depending on the load.
Antihypertensive drugs for diabetes mellitus
To date, eight groups of antihypertensive drugs are known, of which five are considered primary, and three are considered additional. Antihypertensive therapy for diabetes mellitus involves taking the following medications:
- diuretics;
- calcium channel blockers;
- beta blockers;
- centrally acting drugs;
- ACE inhibitors;
- angiotensin II receptor blockers;
- alpha-blockers;
- renin inhibitor (racillosis).
Medicines that make up additional groups are prescribed, most often, as components of combination treatment.
Cardiac problems of patients with diabetes mellitus
Report by Professor Drapkina O.M., read at the II International Internet Congress of Internal Medicine Specialists (February 15, 2013).
Professor Drapkina O.M.: – I’ll move on to my report.
(00:03) Screensaver: Cardiac problems in a patient with diabetes.
Professor Drapkina O.M.: – And I’ll try to highlight a cardiologist’s view of the problem in patients with diabetes. And I want to say right away that, almost without exaggeration, we can state that this is a cardiovascular disease. And the statistics confirm this.
It should be noted that everything we know in general about cardiovascular risks and cardiovascular outcomes: heart attack, stroke, sudden death, coronary heart disease - is many times higher in patients with diabetes.
There is a very interesting study that says that if a patient has already had a myocardial infarction, but does not have diabetes, then the rate of recurrent myocardial infarction will be 18.8%. And if we have a patient diagnosed with diabetes mellitus and no myocardial infarction, then his risk of recurrent myocardial infarction will be even higher. This means that we can logically come to the conclusion that the presence of diabetes mellitus is more significant for recurrent myocardial infarction than a previous cardiovascular accident. And the risk doubles in cases where the patient already has diabetes mellitus and has already had a myocardial infarction. We can say that type 2 diabetes mellitus takes days to form, then years and decades. But still, the patient goes through several of these fundamental points.
At first this is the norm, then it is a very important moment when we can already determine impaired glucose tolerance. And, in the end, everything turns into type 2 diabetes. In this case, insulin secretion can be compensated for a long time, and only at the stage of impaired glucose tolerance can we see and “grasp” increased insulin secretion. And then comes the stage of so-called insulin insensitivity, when sensitivity to insulin decreases somewhat. This increases glucose tolerance in the same way as fasting glucose. And the patient demonstrates hyperglycemia, decreased glucose tolerance, decreased sensitivity to insulin, or, let’s say, it is not the receptor that is actually to blame for insulin resistance, but a violation of the intracellular signal, and hyperinsulinemia, and then a lack of pancreatic beta cells.
But we, as practicing doctors, of course, need to know the basic criteria for diabetes mellitus: fasting plasma glucose - more than 7 mmol/l. If there is any doubt, a glucose tolerance test should be performed. And after it, glucose should be within the range of more than and equal to 11.1 mmol/l. If plasma glucose is detected more than 11.1 mmol/l at any time, then patients have symptoms of diabetes mellitus and, finally, an increase in the level of glycosylated hemoglobin - more than 6.5%.
I would like to say a few words about the normal physiology of glucose metabolism. We understand that food, especially carbohydrates, when absorbed, causes blood glucose to increase. All this mediates a signal to the pancreas, which is responsible for normal insulin production. And normally produced insulin will cause blood glucose levels to instantly normalize.
If insulin resistance occurs - the very first part with which diabetes mellitus begins, then not only the production of insulin changes first - this is indeed the case, and then other processes also change. For example, excess fat breakdown occurs, which leads to an increase in free fatty acid levels.
And this is where the cascade of reactions begins, which Tatyana Evgenievna already spoke about today. Free fatty acids rush through the portal vein directly to the liver, and there the formation of, as we say, primary insulin resistance occurs. In addition, insulin-dependent glucose uptake into muscles is reduced. And it is at the muscle level, as some experts believe, that secondary insulin resistance occurs.
Thus, we can say that insulin resistance is the body's response to maintain insulin levels above its normal values to ensure normoglycemia. Consider the insulin receptor, which consists of two alpha subunits and two beta subunits. We can see that these subunits are connected using special bonds. And, in principle, if this receptor functions normally, then intracellular signal transmission mechanisms occur. And if suddenly at some stage, and most often the stage of implementing metabolic effects suffers by reducing the activity of phosphatidylinositol 3-kinase, which makes it impossible to activate the GLUT4 transporter, then the situation turns out that there is a lot of glucose and insulin in the cell. But at the same time, the signal that will ensure the transport of glucose directly into the cell does not fully occur.
Insulin resistance and non-alcoholic fatty liver disease is a “chicken or the egg – which comes first” situation? If you look at the insulin receptor, consisting of two subunits, then visceral fat: lipolysis, pro-inflammatory cytokines lead to the production of a large amount, for example, tumor necrotizing factor alpha (TNF-?), of free fatty acids, the processes of serine phosphorylation change insulin receptor residues (IRS1). And we see that the phosphatidylinositol 3-kinase pathway is blocked, which makes it impossible for the production and normal activity of the GLUT4 transporter. Today I am faced with the task of looking at the problem of diabetes mellitus from the cardiological “window”. And we see that everything that a cardiologist encounters: hypertension, dyslipidemia, the risk of thrombosis or thrombophilic status, renal dysfunction, microalbuminuria - these are all logical consequences of insulin resistance, and all of these are processes that do not just increase cardiovascular risk, and this is a patient with cardiovascular risk.
Thus, to summarize the first part of my message, I want to say that diabetes mellitus and the risk of cardiovascular diseases are inexorably linked - this is both macrovascular risk and microvascular risk. Speaking about macrovascular risks, we see a patient with a spectrum of problems: heart failure, myocardial infarction, stroke, arterial hypertension. Such a patient is also at risk of microvascular risks: retinopathy, nephropathy, neuropathy and erectile dysfunction.
I would like to briefly discuss the three main problems of a patient with diabetes mellitus: atherosclerosis, arterial hypertension and heart failure. Of course, the discussion about how to normalize glycemic levels is very attractive, since now, after all, the hypothesis of ultra-tight control of blood glucose levels has not lived up to the expectations that were placed on it, especially after the ACCORD study. However, I will not touch on this issue.
So, atherosclerosis. It is absolutely clear that a patient with diabetes has an increased level of low-density lipoproteins and an increased level of total cholesterol. But not only the increase in low-density lipoprotein levels in itself has prognostic significance. These lipids definitely change their properties - they are small, under-oxidized low-density lipoproteins, which are extremely virulent and which very quickly penetrate the subendothelial space and form a plaque. What type of plaque it will be: stable or unstable depends on many factors. But the presence of high LDL, high triglycerides and total cholesterol makes the atherosclerotic changes that a patient with diabetes exhibits very recognizable.
Postulating, we can say that the main features of atherosclerosis in diabetes mellitus are the following signs. This atherosclerosis begins early - about 8-10 years earlier compared to those who, for example, do not have diabetes. It is recognized even at the stage of impaired glucose tolerance. It progresses quickly and is polysegmental in nature. And as always, atherosclerosis is localized not only in large vessels, but also in vessels of medium diameter.
Depending on the level of low-density lipoproteins, high-density lipoproteins and triglycerides, we can say that patients with diabetes will also have a different risk of coronary heart disease. And, naturally, it will be higher in those with LDL levels more than 130 mg/dL, and HDL levels less than 35-45 mg/dL in men and in women who meet this risk.
Please note that triglyceride levels may be more than 400 mg/dL. And in this case, of course, we always keep in mind the possibility of developing so-called pancreatogenic pancreatitis. We can probably be relatively calm if our patient with diabetes has an LDL level of less than 100 mg/dL, an HDL level of more than 45-50 mg/dL and triglycerides of less than 200 mg/dL.
There are recommendations from the American Diabetes Association that were released in 2012. And I would like to say a few words about them, because, in my opinion, they are very convenient and well remembered. And, besides, dear colleagues, you will always have the opportunity to watch the lectures and once again refresh your memory of everything we talked about today.
Experts recommend that, regardless of baseline lipid levels, statins should be prescribed to patients with overt coronary heart disease. Regardless of baseline lipid levels, statins should be prescribed to patients over 40 years of age without CAD who have one or more risk factors for CAD.
For patients at lower risk, statins are prescribed when LDL levels are more than 2.6 mmol/L. And in patients without coronary artery disease, LDL levels should be below 2.6 mmol/L. In high-risk patients with coronary heart disease (and we say that most often patients with diabetes mellitus are already very high-risk patients), here, of course, the target figure is somewhat different - it is less than 1.8 mmol/l.
We continue to follow these recommendations. The next point in them is the following postulate: an alternative goal of reducing LDL, if we cannot achieve these “magic” numbers - 2.6 and 1.8 mmol/l, then we must try to reduce low lipoprotein levels by at least 40% from the initial level density. The target triglyceride level is below 1.7 mmol/L. The target level for high-density lipoproteins is more than 1.0 mmol/L in men and more than 1.3 mmol/L in women.
Finally, the combination of statins with other lipid-lowering drugs is being considered. There isn't much choice here at all. There was such a very attractive hypothesis, which, of course, has a right to exist - these are statins plus fibrates. Indeed, when hypertriglyceridemia is severe, fibrates are the drugs of choice in patients with diabetes mellitus. But again, after the ACCORD study, this concept did not show an impact on the prognosis of these patients. Therefore, the medical community is now looking for new combinations.
The hypothesis of combining statins with certain “hepatoprotectors”, which essential phospholipids can show themselves to be, is very attractive. Statins should be prescribed, as evidenced by large, large randomized studies.
But let's summarize what the analysis of the problem of atherosclerosis gives us. So our goal: LDL is less than 70 g/dL, diabetes is equivalent to CAD, and aggressive LDL control is needed, which will influence morbidity and mortality.
I would like to say a few more words about arterial hypertension. Arterial hypertension has a number of features in patients with diabetes mellitus. And, of course, hyperinsulinemia, which occurs in response to insulin resistance, contributes to this feature. This hyperinsulinemia is extremely aggressive because it leads to overactivation of the sympathoadrenal system, activation of the renin-angiotensin-aldosterone system, and sodium retention.
And this means that in the combination (necessarily combined) therapy of a patient with diabetes mellitus and arterial hypertension there will be diuretics, because this is volume-dependent arterial hypertension, there will be drugs that reduce sympathoadrenal activity and the activity of the renin-angiotensin-aldosterone system. The important thing is that there are some peculiarities here too.
The HOT study demonstrated that at the same level of diastolic blood pressure, the risk of developing cardiovascular accidents is greater in patients with diabetes, although the level of diastolic pressure is exactly the same. This suggests that we should probably be more skeptical or more aggressive in reducing diastolic and systolic blood pressure in patients with diabetes.
Let us turn to the recommendations of experts, who tell us that it is necessary to mentally change the lifestyle of a patient with a systolic blood pressure of up to 139 mm Hg. and diastolic – up to 89 mm Hg. All this happens over the course of three months. If lifestyle changes do not help within three months, you should resort to antihypertensive drugs. Well, if the systolic blood pressure when the patient comes to you is 140 and 90 mm Hg or more, then antihypertensive therapy is immediately indicated. In this case, the appointment of either an ACE inhibitor or an ARA is indicated. If one class is intolerable, another is prescribed. Combination therapy is usually needed to achieve target levels. And you definitely need to monitor kidney function, that is, look at the glomerular filtration rate, potassium level and creatinine level.
Another feature of arterial hypertension in such patients is the rigidity of the vascular wall. Vascular wall stiffness is an independent predictor of overall and cardiovascular mortality. In order to say that the rigidity of the vascular wall is the process from which arterial hypertension may begin, I want to say that the speed of the pulse wave is of great importance.
Our vessels are tubes, and if they are more rigid, then the wave of blood that left the left ventricle and hit the walls of the aorta or small vessels will return back at a higher speed. And we see that if the return wave is superimposed on the wave of blood exiting the aorta into the left ventricle, this leads to an increase in pulse pressure. An increase in pulse pressure, in turn, leads to a very unpleasant phenomenon - augmentation of pulse waves. If the patient has diabetes - and, as a rule, this is combined with non-alcoholic fatty liver disease - expect endothelial dysfunction. And it statistically significantly more often affects patients with diabetes.
We did a lot of research. We had many patients with obesity, insulin resistance, and diabetes. And it turned out that even if your patient is not yet hypertensive, then by conducting daily blood pressure monitoring (ABPM), you will identify a circadian disorder in him, a violation of the daily blood pressure profile. At night there will not be a sufficient reduction in blood pressure, which means that this not yet hypertensive patient will become hypertensive, which will naturally require drug therapy. Thus, another study proving that the stiffness of the vascular wall, which was measured by increasing pulse wave speed, has its place.
Why do blood vessels become stiff? Yes, because there is fibrosis. Remember, this is where we started today: the renin-angiotensin-aldosterone system and fibrosis are inextricably linked. And if we remember those observations that explain the pathogenesis of arterial hypertension in patients with diabetes mellitus, then we will also remember the activity of the sympathoadrenal system and the activity of the renin-angiotensin-aldosterone system. This means that this also needs to be addressed. There are parallels in the development of fibrosis of the liver and heart.
If we look at the clinical predictors of the development of fibrosis and cirrhosis, the cardiologist will exclaim: “Oh my God, these are known risk factors for the development of cardiovascular diseases: age, body weight, diabetes mellitus, nonspecific inflammation!” And we are looking at clinical predictors of the development of liver fibrosis and cirrhosis. “What is good for the heart is also good for the liver” - this postulate is becoming more and more firmly established in our lives.
It is guided by these reflections that we are now conducting research called “Result”. These are patients with arterial hypertension, with a high risk according to SCORE - more than 5%. And, it is clear that we treat them as expected. And it is necessary to treat arterial hypertension, and it is necessary to treat their atherosclerosis.
But in one case we added Rezalut to atorvastatin, and in the other case we did not, that is, we divided all patients into two groups. And according to these preliminary data, it turned out that before and after therapy, of course, the results of cholesterol and low-density lipoprotein levels differ significantly - atorvastatin did its job. Together with Rezalut he made it a little better. But this did not reach statistical significance, but the augmentation index decreased statistically significantly. That is, the vascular wall of these patients became a little more elastic. And this is statistically significant in the group of atorvastatin with Rezalut.
And in conclusion, I want to say that heart failure in these patients is also special, and it is again associated with fibrosis. They may also have unaffected coronary arteries, and pain may be caused by extravasal compression of the coronary arteries. These patients usually have microangiopathic changes in the venules and capillaries of the heart. And, in addition, these patients have supraventricular rhythm disturbances in both men and women. And this suggests that atrial fibrillation occurs much more often in patients with diabetes.
So, we have a very specific treatment goal: glycosylated hemoglobin - less than 6.5%, blood pressure - less than 130/80 mmHg, low-density lipoprotein level - less than 1.7 mmol/l and high-density lipoprotein level - more 1.2 mmol/l. I think the goals have been set. And we will wait for that “beautiful distant future” when we will be able to influence the processes of fibrosis.
Antihypertensive therapy: general rules
Both symptomatic hypertension and hypertension require correction with drugs that have a hypotensive effect. Antihypertensive therapy can be carried out with drugs that differ in their mechanism of action: antiadrenergic agents, vasodilators, calcium antagonists, angiotensin antagonists, and diuretics.
You can obtain information about the hypotensive effect of the drug and what medications to take for high blood pressure not only from your doctor, but also from your pharmacist.
Arterial hypertension is a chronic disease that requires constant drug support, daily monitoring and regular use of prescribed medications. Not only the state of health, but also the life of a person depends on compliance with these rules.
Despite the general availability of treatment rules for reducing blood pressure, many patients have to be reminded what a treatment regimen for hypertension should look like:
- Antihypertensive medications should be taken regularly, regardless of the patient’s well-being and blood pressure level. This allows you to increase the effectiveness of blood pressure control, as well as prevent cardiovascular complications and target organ damage;
- It is necessary to strictly adhere to the dosage and use the form of the drug prescribed by the attending physician. Independently changing the recommended dose or replacing the drug may distort the hypotensive effect;
- even if you are constantly taking antihypertensive drugs, it is necessary to systematically measure blood pressure, which will allow you to evaluate the effectiveness of therapy, timely identify certain changes and adjust treatment;
- in the case of an increase in blood pressure against the background of constant antihypertensive treatment - the development of an uncomplicated hypertensive crisis, an additional dose of a previously taken long-acting drug is not recommended. Blood pressure can be quickly reduced using short-acting antihypertensive drugs.
Antihypertensive therapy: drugs to lower blood pressure
During antihypertensive therapy, several main groups of drugs that help lower blood pressure are currently used:
- beta blockers;
- ACE inhibitors;
- calcium antagonists;
- diuretics;
- angiotensin II receptor blockers.
All of the above groups have comparable effectiveness and their own characteristics that determine their use in a given situation.
Beta blockers
Drugs in this group reduce the likelihood of developing coronary complications in patients suffering from angina pectoris, prevent cardiovascular accidents in patients with myocardial infarction, tachyarrhythmia, and are used in patients with chronic heart failure. Beta-blockers are not recommended for patients with diabetes mellitus, lipid metabolism disorders and metabolic syndrome.
ACE inhibitors
Angiotensin-converting enzyme inhibitors have pronounced hypotensive properties, they have organoprotective effects: their use reduces the risk of complications of atherosclerosis, reduces left ventricular hypertrophy, and slows the decline in renal function. ACE inhibitors are well tolerated and have no negative effects on lipid metabolism and glucose levels.
Calcium antagonists
In addition to antihypertensive properties, drugs in this group have antianginal and organoprotective effects, help reduce the risk of strokes, atherosclerotic lesions of the carotid arteries and left ventricular hypertrophy. Calcium antagonists may be used alone or in combination with other drugs that have antihypertensive properties.
Diuretics
Diuretic drugs are usually used in combination with other antihypertensive drugs in order to enhance the therapeutic effect.
Diuretics are also prescribed to persons suffering from pathologies such as refractory hypertension and chronic heart failure. To avoid the development of side effects, when taking these drugs continuously, minimal dosages are prescribed.
Angiotensin II receptor blockers
Drugs in this group, which have neuro- and cardioprotective effects, are used to improve control of blood glucose levels. They can increase the life expectancy of patients suffering from chronic heart failure. Antihypertensive therapy using angiotensin II receptor blockers can be prescribed to patients who have had a myocardial infarction, suffer from renal failure, gout, metabolic syndrome and diabetes mellitus.