Angina pectoris (angina pectoris) is a sharp pain or discomfort in the chest area. The reason for this is a lack of blood supply to certain areas of the heart. Angina pectoris is noted as a leading symptom in coronary heart disease (CHD), which develops due to blockage or narrowing of the blood vessels of the heart. All patients experience approximately the same sensations - pressing or squeezing pain behind the chest, which often radiates to the arm, shoulder, jaw or neck. The pain usually does not last more than 5 minutes and disappears after taking certain medications or relieving tension. However, the duration of the attack is purely individual; some patients experienced pain from 30 seconds to 30 minutes.
Symptoms
When angina occurs, the pain is usually intense and can be relieved by taking nitroglycerin along with stopping physical activity. These pain sensations have characteristic features: a pronounced time of onset and cessation (nature of the attack), occurrence in certain circumstances.
Among the most common conditions for the occurrence of an attack of angina pectoris are active walking (acceleration of movement, climbing a mountain, difficulty in the form of a sharp headwind, heavy load). Also, other physical efforts and significant emotional stress can cause symptoms of angina pectoris. To determine pain arising from physical effort, it is enough to stop the tension. And the discomfort will subside within 5 minutes. The complete elimination of the symptoms of angina pectoris is facilitated by taking nitroglycerin. As a rule, to make a diagnosis, it is enough to take into account the above symptoms and signs: an increase in pain during physical activity, a favorable reaction to nitroglycerin and the nature of the attack.
Publications in the media
Stable angina pectoris is one of the main manifestations of coronary artery disease. The main and most typical manifestation of angina pectoris is chest pain that occurs during physical activity, emotional stress, when going out into the cold, walking against the wind, or at rest after a heavy meal.
Statistical data. Every year, angina pectoris is recorded in 0.2–0.6% of the population, with its predominance in men aged 55–64 years (0.8% of cases). It occurs in 30,000–40,000 adults per 1 million population per year, and its prevalence depends on gender and age • In the age group of the population 45–54 years, angina pectoris is observed in 2–5% of men and 0.5–1% of women , in the group of 65-74 years - in 11-20% of men and 10-14% of women (due to a decrease in the protective effect of estrogens in menopause) • Before MI, angina pectoris is observed in 20% of patients, after MI - in 50% of patients.
Etiology • In most cases, angina pectoris occurs due to atherosclerosis of the coronary arteries. Although the correlation between the degree of atherosclerotic narrowing, its extent and the severity of the clinical manifestations of angina is insignificant, it is believed that the coronary arteries must be narrowed by at least 50–75% before a discrepancy between the myocardial oxygen demand and its delivery appears and the clinical picture of the disease arises • Other causes (relative coronary insufficiency) •• Aortic stenosis •• Hypertrophic cardiomyopathy •• Primary pulmonary arterial hypertension •• Severe arterial hypertension •• Aortic valve insufficiency.
Pathogenesis • As a result of a discrepancy (imbalance) between the myocardial need for oxygen and its delivery through the coronary arteries due to atherosclerotic narrowing of the lumen of the coronary arteries, the following occur: •• Myocardial ischemia (clinically manifested by chest pain) •• Violations of the contractile function of the corresponding part of the heart muscle •• Changes biochemical and electrical processes in the heart muscle. In the absence of a sufficient amount of oxygen, cells switch to an anaerobic type of oxidation: glucose breaks down to lactate, intracellular pH decreases and energy reserves in cardiomyocytes are depleted • Subendocardial layers are primarily affected • The function of cardiomyocyte membranes is disrupted, which leads to a decrease in the intracellular concentration of potassium ions and an increase in intracellular concentration of sodium ions • Depending on the duration of myocardial ischemia, changes can be reversible or irreversible (myocardial necrosis, i.e. infarction) • Sequences of pathological changes during myocardial ischemia: impaired myocardial relaxation (impaired diastolic function) - impaired myocardial contraction (impaired systolic function ) - ECG changes - pain syndrome.
Canadian Cardiovascular Society Classification Pain does not occur when walking or climbing stairs. Seizures occur with severe, rapid or prolonged strain at work • Class II - “mild limitation of usual activities.” Pain occurs when walking or quickly climbing stairs, walking uphill, walking or climbing stairs after eating, in the cold, against the wind, during emotional stress, or within a few hours of waking up. Walking more than 100–200 m on level ground or climbing more than 1 flight of stairs at a normal pace and under normal conditions • Class III - “significant limitation of usual physical activity.” Walking on level ground or climbing one flight of stairs at a normal pace under normal conditions provokes an attack of angina pectoris • Class IV - “impossibility of any physical activity without discomfort.” Seizures may occur at rest
CLINICAL MANIFESTATIONS
Complaints. Characteristics of the pain syndrome • Localization of pain - retrosternal • Conditions for the occurrence of pain - physical activity, strong emotions, large meals, cold, walking against the wind, smoking. Young people often have the so-called phenomenon of “going through pain” (the “warm-up” phenomenon) - a decrease or disappearance of pain while increasing or maintaining the load (due to the opening of vascular collaterals) • Duration of pain - from 1 to 15 minutes, has an increasing character (“ crescendo"). If the pain continues for more than 15 minutes, the development of MI should be assumed • Conditions for stopping pain - stopping physical activity, taking nitroglycerin • The nature of pain during angina (squeezing, pressing, bursting, etc.), as well as the fear of death, are very subjective and not have serious diagnostic significance, since they largely depend on the physical and intellectual perception of the patient • Irradiation of pain - both to the left and right parts of the chest and neck. Classic irradiation - to the left arm, lower jaw.
Associated symptoms are nausea, vomiting, increased sweating, fatigue, shortness of breath, increased heart rate, increased (sometimes decreased) blood pressure.
Angina equivalents: shortness of breath (due to impaired diastolic relaxation) and severe fatigue during exercise (due to decreased cardiac output due to impaired systolic myocardial function with insufficient oxygen supply to skeletal muscles). In any case, symptoms should decrease when exposure to the provoking factor (physical activity, hypothermia, smoking) or nitroglycerin is stopped.
Physical data • During an attack of angina pectoris - pallor of the skin, immobility (patients “freeze” in one position, since any movement increases the pain), sweating, tachycardia (less often bradycardia), increased blood pressure (less often, its decrease) • Extrasystoles, “rhythm” can be heard gallop”, systolic murmur resulting from mitral valve insufficiency as a result of dysfunction of the papillary muscles • An ECG recorded during an attack of angina can detect changes in the terminal part of the ventricular complex (T wave and ST segment), as well as cardiac arrhythmias.
Laboratory data - supporting value; They can only determine the presence of dyslipidemia, identify concomitant diseases and a number of risk factors (DM), or exclude other causes of pain (inflammatory diseases, blood diseases, thyroid diseases).
Instrumental data
• ECG during an attack of angina: repolarization disturbances in the form of changes in T waves and ST segment displacement up (subendocardial ischemia) or down from the isoline (transmural ischemia) or heart rhythm disturbances.
• Daily ECG monitoring allows you to identify the presence of painful and non-painful episodes of myocardial ischemia in the usual conditions for patients, as well as possible heart rhythm disturbances throughout the day.
• Bicycle ergometry or treadmill (stress test with simultaneous recording of ECG and blood pressure). Sensitivity - 50-80%, specificity - 80-95%. The criterion for a positive stress test during bicycle ergometry is ECG changes in the form of horizontal ST segment depression of more than 1 mm lasting more than 0.08 s. In addition, stress tests can reveal signs associated with an unfavorable prognosis for patients with angina pectoris: •• typical pain syndrome •• ST segment depression of more than 2 mm •• persistence of ST segment depression for more than 6 minutes after cessation of exercise •• appearance of segment depression ST when the heart rate (HR) is less than 120 per minute •• the presence of ST depression in several leads, ST segment elevation in all leads, with the exception of aVR •• absence of a rise in blood pressure or its decrease in response to physical activity •• the occurrence of cardiac arrhythmias ( especially ventricular tachycardia).
• EchoCG at rest allows you to determine the contractility of the myocardium and conduct a differential diagnosis of pain syndrome (heart defects, pulmonary hypertension, cardiomyopathies, pericarditis, mitral valve prolapse, left ventricular hypertrophy in arterial hypertension).
• Stress echocardiography (echocardiography assessment of the mobility of left ventricular segments with an increase in heart rate as a result of dobutamine administration, transesophageal pacemaker or under the influence of physical activity) is a more accurate method for detecting coronary artery insufficiency. Changes in local myocardial contractility precede other manifestations of ischemia (ECG changes, pain). The sensitivity of the method is 65–90%, specificity is 90–95%. Unlike bicycle ergometry, stress echocardiography can detect coronary artery insufficiency when one vessel is affected. Indications for stress echocardiography are: •• atypical angina pectoris (the presence of angina equivalents or an unclear description of the pain syndrome by the patient) •• difficulty or impossibility of performing stress tests •• uninformativeness of bicycle ergometry in a typical clinical picture of angina pectoris •• absence of changes on the ECG during stress tests due to for blocks of the His bundle branches, signs of left ventricular hypertrophy, signs of Wolff–Parkinson–White syndrome in a typical clinical picture of angina pectoris •• positive stress test during bicycle ergometry in young women (since the likelihood of coronary artery disease is low).
• Coronary angiography is the “gold standard” in the diagnosis of coronary artery disease, since it allows us to identify the presence, location and degree of narrowing of the coronary arteries. Indications (recommendations of the European Society of Cardiology; 1997): •• exertional angina pectoris above functional class III in the absence of the effect of drug therapy •• exertional angina pectoris I–II functional class after MI •• exertional angina pectoris with His bundle branch block in combination with signs of ischemia according to data myocardial scintigraphy •• severe ventricular arrhythmias •• stable angina in patients undergoing vascular surgery (aorta, femoral, carotid arteries) •• myocardial revascularization (balloon dilatation, coronary artery bypass grafting) •• clarification of the diagnosis based on clinical or professional (for example, pilots) considerations.
• Myocardial scintigraphy is a method of visualizing the myocardium that allows identifying areas of ischemia. The method is very informative when it is impossible to evaluate the ECG due to blockades of the His bundle branches.
Diagnostics. In typical cases, stable angina pectoris is diagnosed based on a detailed history, a detailed physical examination of the patient, a resting ECG recording, and subsequent critical analysis of the data obtained. It is believed that these types of examinations (history, examination, auscultation, ECG) are sufficient to diagnose angina pectoris with its classic manifestation in 75% of cases. If there is any doubt about the diagnosis, 24-hour ECG monitoring, stress tests (veloergometry, stress echocardiography) are performed consistently, and if appropriate conditions are present, myocardial scintigraphy is performed. At the final stage of diagnosis, coronary angiography is necessary.
Differential diagnosis. It should be borne in mind that chest pain syndrome can be a manifestation of a number of diseases. We should not forget that there may be several causes of chest pain at the same time • Cardiovascular disease •• MI •• Angina pectoris •• Other causes ••• possibly of ischemic origin: aortic stenosis, aortic valve insufficiency, hypertrophic cardiomyopathy, arterial hypertension, pulmonary hypertension , severe anemia ••• non-ischemic: aortic dissection, pericarditis, mitral valve prolapse • Gastrointestinal diseases •• Esophageal diseases - esophageal spasm, esophageal reflux, esophageal rupture •• Stomach diseases - peptic ulcer • Diseases of the chest wall and spine •• Anterior thoracic syndrome walls •• Syndrome of the anterior scalene muscle •• Costal chondritis (Tietze syndrome) •• Damage to the ribs •• Herpes zoster • Lung diseases •• Pneumothorax •• Pneumonia involving the pleura •• PE with or without pulmonary infarction • Pleural diseases.
TREATMENT. The goals are to improve the prognosis (prevention of MI and sudden cardiac death) and reduce the severity (elimination) of symptoms of the disease. Non-drug, medicinal (drug) and surgical treatment methods are used.
• Non-drug treatment - impact on risk factors for coronary artery disease: dietary measures to reduce dyslipidemia and reduce body weight, smoking cessation, sufficient physical activity in the absence of contraindications. Normalization of blood pressure levels and correction of carbohydrate metabolism disorders are also necessary.
• Drug therapy - three main groups of drugs are used: nitrates, b-blockers and slow calcium channel blockers. Additionally, antiplatelet agents are prescribed.
Nitrates. When nitrates are administered, systemic venodilation occurs, leading to a decrease in blood flow to the heart (reduction in preload), a decrease in pressure in the chambers of the heart and a decrease in myocardial tension. Nitrates also cause a decrease in blood pressure, reduce resistance to blood flow and afterload. In addition, the expansion of large coronary arteries and an increase in collateral blood flow are important. This group of drugs is divided into short-acting nitrates (nitroglycerin) and long-acting nitrates (isosorbide dinitrate and isosorbide mononitrate).
• To relieve an attack of angina, nitroglycerin is used (tablet forms sublingually in a dose of 0.3–0.6 mg and aerosol forms - spray - are also used in a dose of 0.4 mg sublingually). Short-acting nitrates relieve pain in 1–5 minutes. Repeated doses of nitroglycerin to relieve an attack of angina can be used at 5-minute intervals. Nitroglycerin in tablets for sublingual use loses its activity after 2 months from the moment the tube is opened due to the volatility of nitroglycerin, so regular replacement of the drug is necessary.
• To prevent angina attacks that occur more often than once a week, long-acting nitrates are used (isosorbide dinitrate and isosorbide mononitrate) • Isosorbide dinitrate at a dose of 10-20 mg 2-4 times a day (sometimes up to 6) 30-40 minutes before expected physical activity. Retard forms of isosorbide dinitrate - at a dose of 40-120 mg 1-2 times / day before the expected physical activity • Isosorbide mononitrate at a dose of 10-40 mg 2-4 times / day, and retard forms - at a dose of 40-120 mg 1-2 r/day also 30–40 minutes before the expected physical activity.
• Tolerance to nitrates (loss of sensitivity, addiction). Regular daily use of nitrates for 1–2 weeks or more can lead to a decrease or disappearance of the antianginal effect •• The reason is a decrease in the formation of nitric oxide, acceleration of its inactivation due to increased activity of phosphodiesterases and increased formation of endothelin-1, which has a vasoconstrictor effect •• Prevention - asymmetric (eccentric) administration of nitrates (for example, 8 a.m. and 3 p.m. for isosorbide dinitrate or only 8 a.m. for isosorbide mononitrate). In this way, a nitrate-free period lasting more than 6–8 hours is provided to restore the sensitivity of the SMC of the vascular wall to the action of nitrates. As a rule, a nitrate-free period is recommended for patients during periods of minimal physical activity and a minimal number of painful attacks (individually in each case) •• Other methods of preventing nitrate tolerance include the use of sulfhydryl group donors (acetylcysteine, methionine), ACE inhibitors (captopril, etc. ), angiotensin II receptor blockers, diuretics, hydralazine, however, the incidence of tolerance to nitrates with their use decreases to a small extent.
Molsidomine is similar in action to nitrates (a nitrocontaining vasodilator). After absorption, molsidomine is converted into an active substance that is converted into nitric oxide, which ultimately leads to relaxation of vascular smooth muscle. Molsidomine is used in a dose of 2–4 mg 2–3 times/day or 8 mg 1–2 times/day (long-acting forms).
b-Adrenergic blockers. The antianginal effect is due to a decrease in myocardial oxygen demand due to a decrease in heart rate and a decrease in myocardial contractility. For the treatment of angina pectoris the following is used:
• non-selective b-adrenergic blockers (act on b1- and b2-adrenergic receptors) - for the treatment of angina, propranolol is used in a dose of 10-40 mg 4 times / day, nadolol in a dose of 20-160 mg 1 time / day;
• cardioselective b-adrenergic blockers (act primarily on b1-adrenergic receptors of the heart) - atenolol at a dose of 25–200 mg/day, metoprolol 25–200 mg/day (in 2 doses), betaxolol (10–20 mg/day), bisoprolol ( 5–20 mg/day).
• Recently, b-blockers have been used that cause peripheral vasodilation, such as carvedilol.
Slow calcium channel blockers. The antianginal effect consists of moderate vasodilation (including coronary arteries), reducing myocardial oxygen demand (in representatives of the verapamil and diltiazem subgroups). Used: verapamil - 80-120 mg 2-3 times / day, diltiazem - 30-90 mg 2-3 times / day.
Prevention of MI and sudden cardiac death
• Clinical studies have shown that the use of acetylsalicylic acid at a dose of 75–325 mg/day significantly reduces the risk of developing MI and sudden cardiac death. Patients with angina pectoris should be prescribed acetylsalicylic acid in the absence of contraindications - peptic ulcer, liver disease, increased bleeding, intolerance to the drug.
• The prognosis of patients with stable angina pectoris is also positively influenced by reducing the concentration of total cholesterol and LDL cholesterol using lipid-lowering drugs (simvastatin, pravastatin). Currently, optimal levels are considered to be no more than 5 mmol/l (190 mg%) for total cholesterol and no more than 3 mmol/l (115 mg%) for LDL cholesterol.
Surgery. When determining the tactics of surgical treatment of stable angina pectoris, it is necessary to take into account a number of factors: the number of affected coronary arteries, left ventricular ejection fraction, and the presence of concomitant diabetes. Thus, with one or two vessel lesions with a normal left ventricular ejection fraction, myocardial revascularization is usually started with percutaneous transluminal coronary angioplasty and stenting. In the presence of two or three-vessel disease and a decrease in the left ventricular ejection fraction of less than 45% or the presence of concomitant diabetes, it is more advisable to perform coronary artery bypass grafting (see also Atherosclerosis of the coronary arteries).
• Percutaneous angioplasty (balloon dilatation) - expansion of a section of the coronary artery narrowed by an atherosclerotic process with a miniature balloon under high pressure under visual control during angiography. The success of the procedure is achieved in 95% of cases. Complications are possible during angioplasty: •• mortality is 0.2% with single-vessel disease and 0.5% with multi-vessel disease, MI occurs in 1% of cases, the need for coronary artery bypass grafting appears in 1% of cases; •• late complications include restenosis (in 35–40% of patients within 6 months after dilatation), as well as the appearance of angina (in 25% of patients within 6–12 months).
• In parallel with the expansion of the lumen of the coronary artery, stenting has recently been used - implantation of stents (thin wire frames that prevent restenosis) at the site of narrowing.
• Coronary artery bypass grafting is the creation of an anastomosis between the aorta (or internal mammary artery) and the coronary artery below (distal) the site of narrowing to restore effective blood supply to the myocardium. A section of the saphenous vein of the thigh, the left and right internal mammary arteries, the right gastroepiploic artery, and the inferior epigastric artery are used as a graft. Indications for coronary artery bypass grafting (recommendations of the European Society of Cardiology; 1997) •• Left ventricular ejection fraction less than 30% •• Lesion of the trunk of the left coronary artery •• The only unaffected coronary artery •• Left ventricular dysfunction in combination with three-vessel disease, especially with damage to the anterior interventricular branches of the left coronary artery in the proximal part •• When performing coronary bypass surgery, complications are also possible - MI in 4-5% of cases (up to 10%). Mortality is 1% for single-vessel disease and 4–5% for multi-vessel disease. Late complications of coronary artery bypass grafting include restenosis (with the use of vein grafts in 10–20% of cases during the first year and 2% each year for 5–7 years). When arterial grafts are used, shunts remain open in 90% of patients for 10 years. Within 3 years, angina returns in 25% of patients.
The prognosis for stable angina pectoris with adequate treatment and monitoring of patients is relatively favorable: mortality is 2–3% per year, fatal MI develops in 2–3% of patients. A less favorable prognosis is for patients with a decrease in the ejection fraction of the left ventricle, a high functional class of stable angina pectoris, elderly patients, patients with multivessel disease of the coronary arteries, stenosis of the main trunk of the left coronary artery, proximal stenosis of the anterior interventricular branch of the left coronary artery.
Age characteristics • Children. The most common cause of symptoms of angina pectoris in children is hereditary dyslipidemia • Elderly - high sensitivity to the side effects of drugs (for example, severe depression when prescribing b-blockers) • Pregnancy - after clarifying the diagnosis, careful observation by an obstetrician and cardiologist is necessary, an increase in the need for oxygen during pregnancy increases the symptoms of angina pectoris.
Prevention • Stop smoking, diet low in cholesterol and fat, regularly perform a set of special exercises • Lipid-lowering drugs.
Synonyms • Angina pectoris • Angina pectoris • Heberden's disease.
ICD-10 • I20.8 Other forms of angina
Causes
The main phenomenon characterizing the symptoms of angina pectoris is an imbalance between the heart's need for oxygen and its direct supply. Due to lack of nutrition of the muscle, its necrosis can develop.
Thus, among the reasons for the lack of oxygen supply to the heart, local disturbances in blood flow are often identified. It can be triggered by chronic narrowing of the lumen of the artery supplying the heart due to atherosclerotic plaque. Angina also occurs due to a sharp and prolonged spasm of the heart vessels. As a result, one part of the heart receives less oxygen than it needs to function properly. During physical activity, this deficiency is felt especially strongly. This is the reason why the vast majority of acute attacks of angina are the result of exhausting and difficult work or stress.
Diagnostics
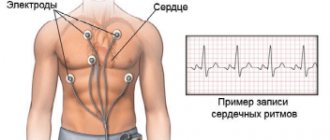
Not all pain in the chest or heart can be called angina. If it lasts less than 30–40 seconds and is eliminated by taking a deep breath or changing body position, there is no need to worry about angina. To make such a diagnosis, the doctor must analyze your complaints, find out the symptoms and the circumstances of their manifestation. In order to exclude concomitant diseases when diagnosing angina, a number of medical tests are carried out, including an electrocardiogram (ECG) in two states (rest and stress), a stress test, blood pressure measurements and x-rays of the coronary arteries.
Thanks to an ECG, the doctor can determine the electrical impulses of the heart, and with them the symptoms of angina pectoris. They show the absence or presence of ischemia (lack of blood supply), characteristics of changes in heart rate and some other parameters. To get a complete picture of cardiac activity, the specialist compares the ECG readings after exercise and at rest, and then decides on the need to treat angina pectoris.
A comprehensive stress test makes it possible to diagnose angina pectoris and assess blood flow in the heart muscle. A small amount of a radioisotope (usually thallium) is used, which is injected into a vein by microinjection during physical activity. Using a special device, the doctor monitors the distribution of thallium in the heart. Uneven concentration or absence of this element in one or another part of the muscle reveals areas of insufficient blood supply.
The most accurate way to determine angina pectoris (angina pectoris) is an angiogram, or x-ray of the coronary artery. The catheter is placed in an artery in the groin or forearm, and then it moves along the bloodstream to one of the heart arteries. Next, a radiopaque liquid is injected, which makes it possible to observe changes in the arteries under study, diagnosing angina pectoris.
ethnoscience
To treat angina pectoris at home, mainly decoctions and mixtures are used. They should include agents with an anticoagulant effect, that is, those that prevent rapid blood clotting, as well as cardiotonic agents, which improve blood circulation.
The list of such drugs includes: hawthorn, rose hips, motherwort, fruits and herbs of dill, roots and herbs of chicory, rhizomes and shoots of asparagus.
Recipes
- Take seven tablespoons of a mixture of hawthorn berries and rose hips, pour two liters of boiling water, wrap in a warm cloth and leave for a day. Strain, squeeze out the swollen berries and put the infusion in the refrigerator. Drink a glass a day with meals for 2-3 weeks.
- Place seven tablespoons of hawthorn berries (whole or chopped) and seven glasses of boiling water in a jar. Then close the jar and wrap it, put it in a warm place for a day. After infusion, strain the medicine, place it in the refrigerator and take three glasses a day with meals. You can add 1-2 tablespoons of rose hips to the preparation for sweetness and increasing the vitamin C content. At the beginning of treatment, you can mix hawthorn berries with motherwort herb in equal proportions, and then you can use only hawthorn berries.
- Hawthorn fruits, sweet clover herb, wild strawberry - two parts each, calendula flowers, meadowsweet herb, lemon balm herb, rue herb, yarrow herb, dill fruits, immortelle flowers - one part at a time (8 g of collection) pour 300 ml of boiling water, heat over water bath without boiling for 15 minutes, leave in a warm place for two hours, strain. Take everything 4-5 times warm an hour before meals and the last time an hour before bedtime. For night attacks, take half a glass hot.
- Take two parts of caraway fruits, periwinkle leaves, three parts of rhizomes with valerian roots, lemon balm leaves, four parts of hawthorn flowers, six parts of mistletoe leaves. Pour a tablespoon of the mixture into a glass of boiling water, leave for two hours and strain. Take two glasses a day for angina pectoris.
- Mix two parts of wild strawberries and one part each of lingonberry leaf, yarrow herb and dog violet herb. Pour a tablespoon of this mixture into a glass of boiling water, leave for an hour and strain. Drink half a glass three times a day.
- Take two parts of canine violet herb and one part of the rhizome with valerian roots. Pour a tablespoon of the mixture into a glass of boiling water, leave for an hour, strain. Take half a glass of the folk remedy three times a day.
Treatment
Successful treatment of angina is usually associated with a reduction in risk factors that can cause cardiovascular problems. These include: high blood pressure, excess cholesterol, excess weight, smoking. The doctor will prescribe you all the necessary medications to bring your blood pressure back to normal, suggest the right diet and help you create a physical exercise program for the treatment of angina pectoris.
Currently, mononitrates, dinitrates and trinitrates are used to relieve the symptoms of angina pectoris. Their mechanism of action is dilation of the blood vessels of the heart, which increases the flow of oxygen and reduces tension in the myocardial wall. Undesirable effects of nitrates in the treatment of angina include headache, decreased blood pressure, facial flushing, dizziness, and insensitivity to certain doses of the drug. Beta blockers, which reduce the strength and frequency of the heartbeat, and calcium channel blockers, which prevent vasospasm, are also used.
In cases where the symptoms of angina are severe and medications are not able to help, surgery (in the form of coronary artery bypass grafting) and balloon angioplasty are prescribed. Coronary artery bypass grafting involves the implantation of a blood vessel into a blocked section of the coronary artery. In this way, blood flow in this part of the heart is restored using a bypass. Angioplasty is an operation to treat angina using a catheter with a small balloon at the end. It is injected into the axillary or femoral artery and then advanced to the site of narrowing of the coronary vessel. Here it quickly inflates or stretches, eliminating the spasm.
Particular attention needs to be paid to the treatment of unstable angina, which can occur even in the absence of strain. Such chest pain does not have predictable boundaries of onset, unlike stable angina, and does not need a reason for its occurrence.
Angina pectoris symptoms and treatment with folk remedies
Angina pectoris (angina) is a spasm of the artery that does not allow blood to pass through, causing the patient to be deprived of the flow of oxygen and can die very quickly. This disease can appear as a result of severe physical or mental stress, especially with a diseased heart. The presence of diabetes predisposes you to angina pectoris. During an attack, the patient feels severe pain, a burning sensation in the pit of the stomach, and excruciating fear. Read more about the symptoms of angina here.
Emergency care for angina and acute myocardial infarction
1. Calm the patient and those around him, sit or lay the patient down (ensure physical and mental peace).
2. Give 1-2 tablets of nitroglycerin under the tongue. If necessary, give nitroglycerin again every 15 minutes. Headaches and noise in the head may occur.
3. Introduce analgin 50% - 2 ml or Tramal - 2 ml intramuscularly, or better yet immediately intravenously with 10-20 ml of 0.9% sodium chloride solution.
4. If the pain is not relieved, narcotic analgesics should be administered intravenously: morphine hydrochloride 1% - 1 ml, omnopon 1-2% - 1 ml, or promedol 1-2% - 1 ml per 10-20 ml 0.9% sodium chloride solution.
5. If the pain remains severe, fentanyl 0.005% - 2 ml (with sodium chloride) is administered intravenously. Fentanyl has the most powerful, but short-term (with intravenous administration - up to 30 minutes) analgesic effect.
6. Simultaneously with narcotic or non-narcotic analgesics, diphenhydramine 1% - 1 ml or seduxen (Relanium) - 2 ml can be administered intramuscularly or intravenously. They enhance the effect of analgesics and have a sedative effect.
7. Antispasmodics and antihypertensive drugs (papaverine, no-shpu, dibazol, magnesium sulfate, etc.) should be administered only if blood pressure significantly exceeds the patient’s working blood pressure, since most drugs used in the treatment of angina and myocardial infarction have hypotensive effect. A sharp and significant decrease in blood pressure can aggravate the patient's condition.
8. It is advisable to carry out oxygen therapy using oxygen devices.
9. Hospitalization of patients with angina pectoris should be carried out on a stretcher in the therapeutic department of the hospital, and patients with new and progressive angina pectoris should be hospitalized in the cardiology department.
10. To hospitalize a patient with acute myocardial infarction without complications, you should call a medical team, and if this is not possible, hospitalize him in the cardiology department (on a stretcher).
11. Hospitalization of patients with acute myocardial infarction with complications (cardiogenic shock, pulmonary edema) is carried out only by a cardiology or medical team.
12. If the patient refuses hospitalization, an active call should be transmitted:
• in the case of stable angina in a chronic patient - to the local doctor of the clinic;
• in case of progressive or new angina and myocardial infarction - to the cardiology ambulance team, which should wait at the patient’s bedside.
13. In all doubtful cases, the principle of overdiagnosis should be observed in the interests of the patient.
14. Drugs that increase myocardial oxygen demand (aminophylline, platyphylline) are contraindicated, and cardiac glycosides (stofantin, corglycone, digoxin) are also contraindicated in patients with acute myocardial infarction or suspected of it.
The following forms of cardiogenic shock are distinguished:
• reflex – occurs at the height of a painful attack and passes after its relief;
• arrhythmic - occurs as a result of a sharp decrease in cardiac output due to acute cardiac arrhythmias (see the corresponding section);
• true cardiogenic shock - caused by a sharp decrease in myocardial contractility as a result of the extensive spread of the necrosis zone, and is the most dangerous complication.
• if you have a seizure, you should put mustard plaster on your heart and dry jars on your back.
If possible, lie still, then the pain will subside and the attack will lose its threatening character.
It is good to take vitamin B15,
as well as
eat plenty of ox liver and drink fresh ox blood.
Such patients should not smoke, as nicotine narrows the arteries.
These are the recommendations of Dr. O. Morozova,
summarizing the experience of old healers and healers.
Traditional medicine recipes:
1. Hawthorn tincture - 20-30 drops 3-4 times a day before meals. Prepared with 70% alcohol concentration 1:10.
2. Liquid extract of hawthorn - 20-30 drops 3-4 times a day.
5 g of hawthorn flowers are poured into 200 ml of hot boiling water, covered with a lid, heated in a water bath for 15 minutes, cooled for 45 minutes. Strain, squeeze and
bring the volume to 200 ml. Drink this infusion 1/2 cup 2-3 times a day for 30 minutes. before meals.
The infusion of fruits is prepared in the same way, but instead of flowers, 15 g of crushed fruits are taken per glass of water. Take 1/2-1/3 cup 2-3 times a day for 30 minutes. before meals.
3. For metabolic disorders, hypertension, angina pectoris, heart attack, stroke, the Tibetan manuscript recommends 1
Once every 3-5 years, carry out a course of treatment as follows.
Prepare a collection of 100 g of each: chamomile flowers, St. John's wort herb, immortelle flowers, birch buds.
Mix everything and chop finely, store in a glass jar with a lid. Prepare the daily dose in the evening, for which 1 tablespoon of the mixture is brewed with 0.5 liters of boiling water and left for 20 minutes. Then filter through linen and squeeze out the remainder. Immediately drink half of the infusion with 1 teaspoon of honey. In the morning, heat the remainder to 30-40 degrees and drink within 20 minutes. before meals. Treatment is carried out daily until the mixture is completely used.
Taking this collection cleanses the body of fat and lime deposits, headaches disappear, and the body rejuvenates.
4. For angina pectoris, menthol with valerian tincture is used to dilate blood vessels.
5. Pumpkin seeds relieve pain from angina pectoris and other cardiovascular diseases.
6. Copper has a good effect on the cardiovascular system .
If the heart hurts, then coins or disks are placed in the subclavian fossa
and
secured there. Usually the pain goes away after 10 days.
Russian doctor P. M. Kurennoye
for angina pectoris recommends:
A very valuable Russian folk recipe for shortness of breath and angina pectoris
This recipe often cures such decrepit old people who cannot walk 50 steps without stopping to rest.
Recipe. Take one liter of honey, squeeze 10 lemons, 10 heads of garlic
peel (whole heads, not cloves) and grind the garlic in a meat grinder. Mix all this together and leave it in a closed jar for a week. Drink 4 teaspoons every day, once a day. Exactly 4 spoons, but do not swallow everything at once, and take your time, slowly consume one spoon after another. Don't miss a day. This amount should be enough for two months.
Treatment with cupping
Treatment requires special jars with a rounded bottom and thick edges.
Banks are placed in areas with a well-developed muscle and fat layer. First, the place where the jars are placed should be smeared with Vaseline, a burning alcohol cotton wool should be placed in each jar for 2 seconds and quickly applied to the back for 5 minutes. You can remove the jar by lightly pressing on the skin around it.
Mud therapy
Take therapeutic mud baths with water temperature from 34 to 37 °C for 10 minutes.
Treatment with oils
Rub 5-6 drops of fir oil onto the area of the coronary vessels (below the nipple) 3-4 times a day.
This recipe is in the form of a letter from an intelligent person.
Preface to the letter.
Among hundreds of thousands of Russian emigrants, unfortunate sufferers of angina pectoris and some other heart diseases, consuming nitroglycerin, there was one person “with a brain” who showed the fallacy of using nitroglycerin and recommending the old, but ever new method of treatment with drugs from medicinal herbs...
Here is the content of this wonderful letter:
“All my life I was a gymnast, a falcon, an athlete and as such I had one hundred percent health. Have you ever wondered what makes me sick?
Three years ago, I was suddenly attacked by angina pectoris, attacked in such a way, with such inhuman pain that I was paralyzed, afraid to move! The doctors assured that this was incurable, and advised to quit work, refuse any activity and... live on nitroglycerin!
I didn’t believe this, I turned to herbs, found hawthorn crategus and began drinking its infusion three glasses a day. After six months of gradual improvement, I completely forgot about nitroglycerin, and now I am as healthy as ever, and at 73 years old I work a full eight hours a day in a factory and do community service in the evenings. I drive a car, sometimes a hundred miles a day without stopping, and walk freely on stairs. Now you know why I need hawthorn, and I need rose hips as vitamin C, as a seasoning for hawthorn, to make it more pleasant to drink.
I prepare the hawthorn infusion like this: I have a saucepan for 7 glasses, I put 7 tablespoons of berries in it (spoons with a “hump”) and pour boiling water over it, put the pan on a non-heat-conducting stand (not a heat-conducting stand - an asbestos sheet of any thickness) , I wrap the pan warmly and keep it like that for about 20 or 24 hours. Then I strain the contents through a cloth, squeeze out the swollen berries and put the juice in the refrigerator. I drink a glass three times a day, with meals... When I began to be treated with herbs, I used hawthorn and core (motherwort) in equal proportions by weight, and six months ago I started using only hawthorn and, frankly speaking, there is not much difference I see.
At my age, vitamin C is necessary, and, of course, you can just buy tablets, but I am a fan of natural remedies and therefore I prefer to brew hawthorn with rose hips, and it’s more pleasant to drink.
Very valuable note, comparison and difference.
Nitroglycerin only calms, and herbs treat... At the first sign of palpitations (even before the attack), you should switch to treatment with hawthorn infusion or hawthorn in half with the core. “Prevention is better than cure,” says Eastern wisdom. With nitroglycerin, after the first attack, a second, and often a third, soon occurs... With herbal treatment (if treatment began before the first attack), this initial attack does not occur for many years. If treatment is started after the first seizure, the second one is delayed for many years. Remember and do not forget that with nitroglycerin, doctors prescribe to give up all physical activity, and with herbal treatment, a person of 70-75 years old can engage in physical labor for eight or more hours a day and not have any heartbeat for many years and can walk up the stairs freely...
Reading a letter from an intelligent person, many will not notice an element of colossal value, that is, the fact that an intelligent person decided to rise, as if on an air carpet, on two elements: on a long rest and... the best medicine in the world for angina pectoris - an infusion of hawthorn berries. Let's take a whole group of patients with angina pectoris. Out of 100 people, 99 would not follow the principle of an intelligent person, since they would turn out to be “people with ... hot livers” and after two to three weeks, feeling a noticeable improvement in their health.
Updated: 2019-07-09 21:34:48
- Treatment with folk remedies for stomach and duodenal ulcers
- Radiculitis treatment with folk remedies
- Polycystic ovary syndrome treatment with folk remedies
- Asthma treatment with folk remedies
- Whooping cough treatment with folk remedies
- Osteoporosis treatment with folk remedies
Prevention
Basic methods of prevention and treatment of angina:
- absolute cessation of smoking and alcohol;
- long walks in a relaxed manner, physical activity within reasonable limits in accordance with doctor’s prescriptions;
- blood pressure control;
- You should follow the diet prescribed by your doctor, limit the consumption of animal fats and salt, increase the use of vegetables, vegetable fats and fruits in your diet;
- detection and appropriate treatment of diabetes mellitus, control of blood glucose levels;
- absence of unnecessary emotional stress.
If you are bothered by regular pain in the chest area during physical activity, this may be a manifestation of stable or unstable angina, which is treated by specialists at our clinics. You should consult a doctor, as each attack of angina inevitably worsens the condition of the heart muscle. You can get professional help at one of our clinics in Moscow. Make an appointment with us by phone +7.