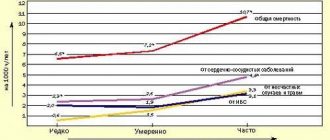
To the question “How does alcohol affect blood pressure?” there are two answers:
- if used rarely in safe dosages - no way;
- Frequent consumption of alcohol always increases blood pressure.
The effect of alcohol on blood pressure is realized through several biochemical mechanisms:
— ethyl alcohol dilutes cell membranes and causes their fluidity. If a person begins to abuse alcohol, the body turns on an adaptation mechanism to protect cell membranes from rapid damage. This is done by increasing the cholesterol content in the membrane, due to which the membranes of the blood vessels become inelastic, and the level of blood pressure increases.
— Excessive alcohol consumption leads to water-electrolyte imbalance and dehydration of the body during intoxication. With frequent drinking, the body is forced to adapt to dehydration and retains fluid even in a state of sobriety. As a result of these changes, blood pressure increases.
— acetaldehyde, an intermediate product of the chemical breakdown of ethyl alcohol, leads to the accumulation of free radicals that oxidize and damage the walls of blood vessels (early aging of blood vessels and the appearance of atherosclerotic plaques).
- drinking beer in large quantities puts a strong strain on the kidneys, disrupts their function, as a result of which fluid is retained in the body, swelling occurs, and blood pressure increases.
— frequent alcohol consumption leads to a compensatory increase in the level of the neurotransmitter glutamate (regulates the processes of neuronal excitation) and a decrease in the activity of the GABAergic system (neurotransmitter of inhibition and relaxation). As a result of overexcitation of neurons and the stimulating effect of glutamate, a person with a hangover after drinking cannot relax, everything is irritating, blood pressure rises after alcohol, heart rate increases, and sleep is disturbed.
River and street
History of microdistricts st. Angarskaya is best tracked through Cold War-era satellite imagery. A photograph from 1964 shows that the area between Angarsk and the Moscow Ring Road was mainly fields, forests and the floodplain of the Trostyanka River. In the northeast within the boundaries of the 1st lane. Artyom, a small part of the Northern Village is visible - a large sector of low-rise buildings for workers of the Minsk Automobile Plant. To the south at that time there was the village of Maloe Stiklevo. Now all that remains is a dead-end street, just over 200 meters long, with a dozen residential buildings. About 60 years ago it was four times longer, only slightly short of the Moscow Ring Road.
The lens of a satellite camera captured the buildings of a psychoneurological boarding home for the elderly and disabled at the address: st. Angarskaya, 46.
In the 1960s, orphans lived and studied there. At the same time, the village of Bolshoye Stiklevo ended here, which is now completely located outside the Moscow Ring Road. Construction on the site of its urban part took place in two stages. At the turn of the 1970s and 1980s, huge 9-story panel “Chinese walls” were erected on the street. Baikalskaya and Gerasimenko. Much later, a 12-story building on Baikalskaya, 37, and a brick house No. 40 on the street appeared on the map. Angarskaya.
Where did Trostyanka, which was mentioned above, take place? Its bed, which already in those years was more of a swamp than a river, was drained in the 1970s during the development of the Angarskaya-2 microdistrict. However, you can still walk along the direction of the winding river bed today. It is almost completely repeated by the tracing of the street. Gerasimenko south of the intersection with Nesterov. These places are distinguished by Siberian and Far Eastern toponymy. Angarskaya is located surrounded by st. Baikal, Khabarovsk, Dezhnev, Ilimsk. A little further west, the street runs away into the private sector. Tomskaya, Irkutskaya, Okhotskaya, Yenisei lanes...
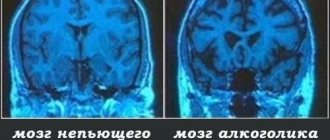
Personality changes
Alcohol degradation is a serious consequence of the chronic form of the disease. In men, it manifests itself later, 7-10 years after the formation of the addiction. In women, the first changes are observed after 3-4 years.
Symptoms of degradation depend on the stage of chronic alcoholism:
- At the first stage, the patient hides her addiction, but tries to find a justified reason for another binge. He justifies drinking alcohol with stress at work, insomnia, increased anxiety, and denies addiction. At the same time, productivity and family relationships are preserved.
- At the second stage, binges appear, which destroy relationships with a partner, provoke quarrels and domestic conflicts. Addiction takes up a person’s thoughts and time, so there is a risk of losing his job and family. Women often lose interest in raising a child and running a household.
- At the last stage, the social appearance is completely lost, the person abandons his usual environment. Life changes dramatically: the family breaks up, favorite work and hobbies do not bring pleasure. Degradation leads to crimes, theft, and domestic murders.
With social and personal degradation, it is difficult to predict the consequences. A person often goes on long drinking bouts and loses interest in life. His intellectual abilities decrease and his memory is lost.
Typical story
The high-rise buildings of the Angarskaya neighborhoods were built in different eras. Our acquaintance with the development begins from the point where the street makes a turn with the letter “G”. Ilimskaya. In the square formed by Ilimskaya, Nesterova and Gerasimenko, panel high-rise buildings were built. However, architects of the 1980s tried to dilute the development with houses with rotating sections.
Along the territory of school No. 173 I come out to the semicircular house 52/2 on Gerasimenko. There is a commemorative and already rare plaque on it. One of his entrances was recognized as the best in Minsk! But we are only talking about things from long ago - this was in 2004. In the same house there was also a strange emergency exit from one entrance. It leads to a platform that is located more than a meter above the ground, and there are no stairs.
The Angarskaya-4 microdistrict ends here. South of the street Nesterov there is his brother at number 3. The difference between the houses of the two microdistricts is striking. The facades of those south of the street. Nesterov, recently repainted.
“Sometimes you can feel the workload in the clinic; nevertheless, about 60 thousand people are assigned to it. And the area is no longer young,” says local old-timer Victor. - But it's big. But the children's room is small, three-story, from the 1960s. There are enough schools and kindergartens for children, there are no problems with shops.
Along the street Nesterov has an interesting installation. Its center is an airplane made of wood, placed on a conventional wing. The authors were probably inspired by the aerobatics performed by the pilot, after whom both it and the street are named.
In general, the Angarskaya-3 microdistrict left a more interesting impression. In the depths of the block there are three brick houses built in the early 1990s.
The courtyards here are visually smaller than in their northern counterpart. Near house number 82 on Nesterova I found original benches. They are stylized as an apple tree branch with fruits. It’s not surprising, because near Ilimskaya, where the journey began, there is agricultural production. There is also a bicycle garage in this yard. The house opposite the control station "Angarskaya-4" is decorated with a giant image of a stork on top. The only thing is that the silence of the courtyards is disturbed by the hum from the Moscow Ring Road.
“It’s great here,” says a man, hurrying on business through the forest park. — The air is clean, only in summer very faint odors can sometimes be heard from the aeration station. Do you know what the view of the forest is from the 11th floor? Sometimes in the evenings you can hear the sounds of trains going from Shabany to Kolodishchi. I have delicious water at home and go to the complex located here to exercise. There is a large shopping center nearby... The area is suitable for living. And soon the major renovations in the house will be completed, it will be even better.
Consequence groups
The peculiarity of alcoholism is that a person, when faced with the consequences, does not realize how dangerous they are. Often fear for one's life appears only with the first pain or heart attack .
The consequences of chronic alcoholism are divided into several groups:
- Social . An alcoholic destroys connections with family and loved ones. The likelihood of committing a crime and getting injured increases.
- Medical . Ethyl alcohol interferes with the blood circulation of internal organs, causes vasospasm, and increases the risk of developing cancer, heart attack and stroke. Absolutely all systems and organs suffer.
- Mental . Due to central nervous system disorders, alcoholics often experience severe mental disorders. Such consequences can only be eliminated by an experienced specialist, subject to treatment in a hospital.
If you regularly drink alcohol, characteristic external signs will appear. Usually this is swelling, puffiness of the face (especially under the eyes), unstable gait, dull or yellowish skin color. The figure also changes. Men begin to gain weight according to the female type. Fat is deposited in the abdomen, hips, and chest.
The causes of the disease often lie in psychological problems and childhood traumas. A person drinks to forget, but only multiplies his problems. It destroys physical and mental health, family, career, but cannot get rid of depression. Alcohol only increases anxiety and fears, so it is by no means an antidepressant.
Like in the forest
I cross the street. Gerasimenko and find myself in the most unusual microdistrict - Angarskaya-2. In its center is a forest park. Just imagine: you can find yourself in a pine forest, leaving the entrance of a high-rise building. I found a numbering incident here. Two 12-story buildings at the intersection of Angarskaya and Nesterov belong to Gerasimenko with numbers 41 and 45. Although the desired street is over 200 m...
One of the points of attraction in Angarskaya-2 is the local supermarket. As it turned out, not only for this area, but also for the neighboring one.
— I came here for shopping by bus. I live at the beginning of the street. Baikalskaya. We have a hard time with convenience stores. It’s no less than a stop to get to any of them,” sighs pensioner Lyudmila Mikhailovna. — And this has been since 1989, when we first moved in. We got used to transport not only here, but also to the hairdresser, and to the post office, and to pick up garden utensils...
But located south of the street. The Baikal microdistrict Angarskaya-1 stands out for its more contrasting buildings. If on the side of the Minsk Ring Road its courtyards are closed with 9-story buildings mainly from the early 1980s, then on the opposite side near the street. The buildings in Angarsk are predominantly 5-storey. Numerous Brezhnevkas grew on the site of the field about half a century ago. These courtyards are familiar to many capital conscripts, since the city military registration and enlistment office is located here. The rest of the area is also easily recognizable thanks to the complex of four 12-story dormitories on the hill from Partizansky Ave. They were built for workers of factories located in the area.
All interlocutors noted good transport links on Angarskaya. The area is not very far from the metro; ten bus and four trolleybus routes reach here. Without transfers from here you can go not only to Shabany or Chizhovka, but also to the area of the Academy of Sciences, Green Meadow, Uruchye, Kurasovshchina, to the station, the market in Zhdanovichi... The only thing is that it seems that the fastest way to get to neighboring Stepyanka is through the forest.
Diagnosis and treatment of emergency conditions associated with alcohol abuse
Chronic alcohol intoxication leads to the development of a number of specific diseases of internal organs and the nervous system, united by the general concept of “somatic equivalents of alcoholism” and the term “alcoholic polyvisceropathy”.
As is known, alcoholic polyvisceropathy is characterized by a relative “benign” course and the potential reversibility of pathological changes if regular intake of alcoholic beverages is stopped. Otherwise, as the degeneration of organs and tissues specific to chronic alcohol intoxication worsens, alcoholic polyvisceropathy leads to multiple organ failure, which often becomes both the cause and background for the development of emergency conditions and death.
Emergency conditions and acute lesions of the digestive organs, as a rule, develop against the background of severe alcohol excess or due to sudden withdrawal of alcohol and the development of alcohol withdrawal syndrome.
Unfortunately, in practice the close cause-and-effect relationship between these events is often underestimated. This is to a certain extent facilitated by the fact that in the international classification of diseases (ICD-10) these diseases are included in various headings.
Let's list the ICD-10 sections related to alcoholic liver disease and emergency conditions due to alcohol abuse.
Alcoholic liver diseases: K70.0 - alcoholic fatty liver disease; K70.1 - alcoholic hepatitis; K70.2 - alcoholic fibrosis/sclerosis of the liver; K72.0 - acute and subacute liver failure; K71.1 - chronic liver failure; K76.6 - portal hypertension.
Alcoholic diseases of the nervous system: G31.2 - degeneration of the central nervous system caused by alcohol; G62.1 - alcoholic polyneuropathy.
Mental disorders: F10.0 - acute poisoning caused by alcohol consumption; F10.3 - withdrawal state caused by alcohol consumption; F10.04 - withdrawal state with delirium caused by alcohol consumption; F10.2 - chronic alcoholism (alcohol dependence).
The risk of death is highest in acute alcohol poisoning. Thus, more than 2 thousand cases of acute alcohol poisoning are recorded annually in Moscow. In 2002, it caused the death of more than 3 thousand residents of the Moscow region. In 2004, 22 thousand people died from acute alcohol poisoning in Russia.
Despite the fact that about 80% of all deaths from acute alcohol and drug poisoning develop outside the clinical setting, emergency conditions associated with alcohol abuse are quite rare in the practice of an outpatient healthcare provider. However, specialists from mobile teams and emergency hospitals (EMS) encounter this pathology almost every day. For example, the number of these patients exceeds 10% of the total number of patients daily in the intensive care units of emergency hospitals. In multidisciplinary emergency hospitals, diseases associated with alcohol abuse are the cause of 10-13% of deaths.
The pathogenetic mechanisms of acute alcohol poisoning are nonspecific and are similar to the mechanisms of development of any exogenous intoxication, including: disruption of the energy supply to the cells of vital organs and systems when overloaded with toxin (alcohol itself and acetaldehyde); introduction into the body of a large amount of “non-electrolytes” (intermediate products of alcohol metabolism); formation of “lethal synthesis” products of certain toxins (acetaldehyde); introduction into the body of a large amount or accumulation of “membranotoxins” (lactic acid, peroxides); direct potentiation of lipid peroxidation, development of deficiency of antioxidant systems.
The strategy for prehospital medical care for acute alcohol poisoning is also based on the well-known methodology for providing emergency care for exogenous intoxication and includes the following stages: identification of the leading pathological syndrome; diagnosis of the severity of the condition and the risk of death of the disease; identification of the etiological factor; differential diagnosis; determining the prognosis of the condition; determination of indications and scope of emergency therapy; determination of indications and choice of direction for emergency hospitalization.
However, from a tactical point of view, when providing prehospital care to a patient with acute alcohol poisoning, it is fundamentally important to remember that this emergency condition develops in the patient against the background of pre-existing, more or less pronounced multiple organ failure, which significantly affects both the severity of the patient’s condition and the prognosis of the disease. In this regard, the severity of damage to internal organs in acute alcohol poisoning is also largely determined by the premorbid background. In patients without clinically significant alcoholic liver disease, symptoms such as jaundice, as well as signs of chronic portal hypertension (hepatomegaly, splenomegaly, varicose veins of the anterior abdominal wall, edema, ascites, etc.) may be completely absent. As a rule, diagnosing acute ethanol poisoning does not cause significant difficulties. Nevertheless, when examining a patient at the prehospital stage, it is advisable to adhere to certain sequences and principles of emergency care for acute alcohol poisoning.
- Establish the fact of recent alcohol intake and determine its characteristics (date of last intake, binge drinking or one-time use, quantity and quality of alcohol consumed, total duration of regular alcohol intake). It is possible to adjust for the social status of the patient.
- Establish the fact of chronic alcohol intoxication and nutritional level.
- Determine the risk of developing withdrawal syndrome.
- As part of toxic visceropathy, determine: the state of consciousness and mental functions, identify gross neurological disorders; stage of alcoholic liver disease, degree of liver failure; identify damage to other target organs and the degree of their functional usefulness.
- Determine the prognosis of the condition and develop a plan for observation and pharmacotherapy.
Obviously, clarifying the patient’s “alcohol” history is aimed at determining the severity of the current acute alcohol poisoning, as well as the risk of developing alcohol withdrawal syndrome (on the 3-5th day after the last intake of alcohol).
The leading clinical syndrome in patients with acute alcohol poisoning is severe exogenous intoxication with predominant dysfunction of the central nervous system and depression of consciousness, development of hepatic-renal failure. The patient emits a distinct odor of alcohol. The condition is severe, consciousness is impaired from stupor to coma (10-0 points on the Glasgow scale). There is severe facial hyperemia, shortness of breath and shallow breathing, acidosis, tachycardia, and oliguria. Patients retain a normal oculocephalic reflex, the eyes look straight, the pupils are not constricted and react to light. At the onset of the disease, a rise in blood pressure and hyperthermia are possible. As the disease progresses, as the patient's condition worsens, a tendency toward the development of hypotension and anuria is determined.
To predict the outcome of acute poisoning, it is also fundamentally important not only to assess the severity of all manifestations of alcoholic visceropathy, but also to determine the degree of preservation of the patient’s personality and social adaptation. The worst prognosis for acute alcohol poisoning will be in patients with alcoholic liver disease and liver failure, convulsive syndrome, alcoholic encephalopathy, severe weight loss and the development of purulent-septic complications.
A reliable laboratory diagnostic marker of acute alcohol poisoning is persistent hypoglycemia. Prehospital blood glucose levels can be easily determined using a strip test or a portable glucometer. For glycemia <3.5 mmol/L, patients with acute ethanol poisoning should receive a single bolus of 40 ml of glucose 40%. It is important to remember that in patients with chronic alcohol intoxication, rapid administration of glucose can accelerate the development of Wernicke encephalopathy. To prevent the development of acute encephalopathy, immediately after the administration of glucose, it is necessary to administer a single intravenous bolus of 100 mg of thiamine. In general, the task of prehospital medical care for acute alcohol poisoning is to organize timely resuscitation and transport the patient to the intensive care unit of a toxicology hospital or emergency hospital. In this regard, prehospital pharmacotherapy is only symptomatic. Directed detoxification therapy with a large amount of isotonic crystalloid solutions in preclinical conditions and in the absence of the possibility of differential diagnosis of acute alcohol poisoning with other causes of impairment of consciousness in patients with chronic alcohol intoxication is inappropriate.
Alcohol-induced withdrawal symptoms
Studying the epidemiology of alcohol withdrawal states caused by alcohol consumption appears to be a much more difficult task. In practice, this section of ICD-10 is taken into account extremely rarely when preparing medical documentation, despite the fact that it is severe withdrawal syndrome that is the most common direct cause of decompensation of alcoholic visceropathy. In 2003, according to the Moscow City Center for Pathological Research, diseases from the spectrum of alcoholic polyvisceropathy were recognized as the cause of death in more than 7% of autopsies performed in hospitals in Moscow. Without a doubt, in the vast majority of these cases, the immediate cause of death was the development of severe withdrawal syndrome in patients with chronic alcohol intoxication. It should be noted that patients with mild to moderate withdrawal are usually treated on an outpatient basis or without the use of medical care or pharmacotherapy.
Withdrawal syndrome is most severe in people who have just suffered acute alcohol poisoning. However, even withdrawal syndrome not complicated by delirium always leads to exacerbation of alcoholic visceropathy. In this case, specific withdrawal symptoms: nausea, vomiting, headache, tremor, severe autonomic disorders, agitation, confusion, behavioral disturbances and hallucinations - may manifest against the background of acute damage or decompensation of the liver, pancreas, heart and blood vessels or the development of purulent -septic complications (most often pneumonia). According to various data, in 30-68% of patients as a result of acute ethanol poisoning against the background of withdrawal syndrome, acute alcoholic hepatitis or decompensation of liver cirrhosis occurs with the development of liver failure - the main cause of severe nausea and vomiting in patients with alcohol withdrawal syndrome. The purpose of this article is not to discuss methods for diagnosing and treating alcoholic liver disease at the prehospital stage. Nevertheless, it should be noted that preclinical diagnosis of alcoholic liver disease is a completely solvable problem, since it is based on questioning and examination of the patient, which allows us to identify most of the specific symptoms of hepatitis and cirrhosis of the liver.
Nausea and vomiting, complicating the course of withdrawal and exacerbation of alcoholic liver disease, are one of the most painful and potentially dangerous syndromes. However, in syndromes associated with alcohol abuse and impairment of consciousness, the main danger of vomiting is the development of potentially fatal emetic complications such as dehydration, hypokalemia, aspiration of vomit and Mallory-Weiss syndrome. To prevent vomiting in patients with nausea, 10 mg of metoclopramide is administered intramuscularly every 6-8 hours as a means of pathogenetic therapy. Simultaneous administration of higher doses of metoclopramide is inappropriate, since it does not lead to a significant increase in the antiemetic effect and is associated with the risk of developing convulsions and central respiratory disorders . As already mentioned, the use of the main means of etiotropic treatment of nausea and vomiting - massive infusion, detoxification therapy - at the prehospital stage is categorically unacceptable. In patients with alcohol withdrawal syndrome, this is especially dangerous, since the administration of large quantities of isotonic crystalloid solutions is fraught with the development of cerebral edema. Against the background of withdrawal syndrome, indications for prehospital infusion therapy with hypertonic glucose solution or rheopolyglucin are dehydration and hypovolemia.
The most dangerous cause of hypovolemia in a patient with alcohol withdrawal syndrome is gastrointestinal bleeding (GIB). As already mentioned, the cause of gastrointestinal tract in the background of abstinence with vomiting is often Mallory-Weiss syndrome - bleeding from an acute fissure in the mucous membrane of the cardia of the stomach. Despite the fact that the overall mortality rate for gastrointestinal bleeding from the mucous membrane of the upper gastrointestinal tract, according to various sources, reaches 8-10%, and for bleeding from varicose veins of the esophagus against the background of chronic portal hypertension - 30-40%, with Mallory-Weiss syndrome the mortality rate is significantly below. This bleeding is usually self-limiting, but its outcome also depends on the total volume of blood loss, which, in turn, is determined by the severity of the concomitant pathology of the hemostatic system characteristic of alcoholic liver damage. One way or another, the following are considered predictors of an unfavorable outcome of gastrointestinal tract diseases: age > 60 years; shock and hypotension: SBP less than 100 mm Hg. Art. in patients under 60 years of age, systolic blood pressure is less than 120 mmHg. Art. in patients over 60 years of age; young people tolerate massive blood loss more easily; orthostatic drop in blood pressure and/or heart rate; severe bradycardia or tachycardia with heart rate >120; chronic liver diseases; other chronic diseases (heart, respiratory system, kidneys); hemorrhagic diathesis; disturbances of consciousness.
Gastrointestinal bleeding should be suspected in any patient with alcohol withdrawal syndrome and persistent hypotension. The basic algorithm of pharmacotherapy in patients with gastrointestinal tract on the background of alcoholic liver disease is presented in the figure.
In patients with signs of chronic alcohol intoxication and alcoholic polyvisceropathy, acute alcohol poisoning and withdrawal syndrome must be differentiated from hepatic encephalopathy (HE). HE is a potentially reversible disorder of nervous and mental activity in any liver disease that occurs with insufficiency of hepatic cellular function. In most cases, PE complicates the course of the terminal stage of chronic diffuse liver diseases or acute necrotizing (fulminant) hepatitis. It has been established that with liver damage of any etiology, PE can lead to the development of coma and become the direct cause of death of the patient.
As with alcohol withdrawal syndrome, the leading clinical syndrome of PE is a deep disorder of consciousness, occurring with intellectual-mnestic and neurological disorders. Early signs of disturbances of consciousness in PE include a decrease in spontaneous movements, a fixed gaze, lethargy, and apathy. Impaired consciousness in PE is, in principle, characterized by drowsiness and inversion of the normal rhythm of sleep and wakefulness. In this case, the worsening of the condition and the transition from drowsiness to coma can be observed within a very short time.
Neurological disorders in PE are generally not specific and can also develop with uremia, severe respiratory and heart failure. However, one of the most pathognomonic neurological symptoms of PE is considered to be the development of “flapping” tremor (asterixis), the distinctive feature of which is the patient’s inability to maintain a fixed position. The greatest severity of hyperkinesis of the muscles of the limbs when maintaining a constant posture and its decrease during movement make it possible to differentiate asterixis from tremor in alcoholic delirium and encephalopathy.
Differential diagnosis of hepatic encephalopathy and alcoholic delirium
Hepatic encephalopathy: drowsiness, sleep disturbance, sleep inversion; “flapping” tremor (pronounced at rest and minimal during voluntary movements); increasing confusion; increased muscle tone and deep tendon reflexes; increased appetite (persistent hypoglycemia).
Alcoholic delirium (withdrawal syndrome): motor and mental agitation; disorganization of consciousness; insomnia; hallucinations; tremor (increases with voluntary movements and disappears at rest); increased activity of the autonomic nervous system; anorexia (normal plasma glucose and hyperglycemia).
Changes in personality and intelligence during PE are the most difficult to diagnose, since they are always superimposed on constitutional, previously acquired disorders and require dynamic assessment. The greatest difficulties in clinical practice are encountered in the differential diagnosis of PE and personality disorders that develop with chronic alcohol abuse (toxic or alcoholic encephalopathy), the presence of which does not directly affect the outcome of acute PE, but determines the risk of developing delirium against the background of alcohol withdrawal syndrome. It is important that in alcoholism, acute PE can develop with any of the clinical and morphological forms of alcoholic liver disease.
In patients with liver cirrhosis, the most important aspect of diagnosis is also to identify the causes that led to the development of PE.
Factors contributing to the development of acute HE in liver cirrhosis
- Metabolic: electrolyte imbalance (taking diuretics, massive vomiting, severe diarrhea); prolonged fasting; stopping drinking alcohol (withdrawal syndrome); massive laparocentesis.
- Bleeding and blood loss: from varicose veins of the esophagus and stomach; from acute gastroduodenal ulcers (portal gastropathy); with Mallory-Weiss syndrome; during surgery or injury.
- Influence of chemical and pharmacological factors: acute alcoholic excess; taking opiates, benzodiazepines, barbiturates.
- Infectious diseases: spontaneous bacterial peritonitis; urinary tract infections; bronchopulmonary infection.
- Constipation.
- A diet high in protein.
In patients with acute PE without signs of chronic portal hypertension (varicose veins of the anterior abdominal wall, edematous-ascitic syndrome, splenomegaly, liver disease or a history of alcoholism), the diagnosis of PE at the prehospital stage is especially difficult. In these cases, the diagnosis of PE should be made, firstly, on the basis of a thorough examination of the medical history (if possible), and secondly, an analysis of the effectiveness of standard nonspecific therapy for coma is necessary. Differential diagnosis in patients without cirrhosis of the liver must be carried out with a number of diseases leading to a sudden and severe impairment of consciousness (Table).
It is known that in patients with premorbid damage to the central nervous system of traumatic, vascular or toxic origin, the withdrawal state is often complicated by the development of alcoholic delirium or convulsive syndrome. For example, in 2002, more than 76 thousand cases of acute alcoholic psychosis were registered in the Russian Federation, and it should be noted that alcoholism and associated behavioral disorders and mental disorders were first diagnosed in 221.3 thousand people.
In international practice, the severity and prognosis of alcohol withdrawal syndrome is usually determined using the CIVA-AR scale, which allows one to evaluate the severity of the above withdrawal symptoms, as well as the state of a number of physiological parameters. The CIVA-AR scale from 0 to 6 allows you to evaluate hyperthermia, diastolic blood pressure, pulse and respiratory rate, severity of nausea and vomiting, tremor, headache, facial flushing, convulsions, sweating, tactile and visual disturbances, auditory hallucinations, general orientation patient in time and space, level of anxiety and contact, general arousal, thinking disorders. Controlled studies have proven the high sensitivity and specificity of the CIVA-AR scale in the treatment and monitoring of patients with alcohol withdrawal (evidence level “A”). With a total score of more than 8 points, alcohol withdrawal syndrome is considered severe, the patient is hospitalized and treated with benzodiazepines - most often, diazepam 10 mg 3 times a day with a gradual dose reduction over the next 3 days. During dynamic observation of the patient, 5 mg of diazepam is administered additionally each time the total score on the CIVA-AR scale exceeds 8 points. If seizures occur, the patient is given a single intravenous dose of lorazepam at a dose of 2 mg.
Observation of a patient with alcohol withdrawal syndrome at the prehospital stage is organized in accordance with general resuscitation principles and pharmacotherapy is administered aimed at maintaining vital functions and correcting hypovolemia. It is advisable to carry out massive infusion and targeted symptomatic therapy, for example, treatment of electrolyte disturbances, at the prehospital stage only if appropriate portable laboratory equipment is available and in accordance with the main indicators of chemical homeostasis.
Today, a number of emergency medical services have at their disposal portable analyzers of gases and electrolytes of blood (such as GASTAT-mini, Techno Medica), which make it possible to determine acid base, glycemic level, partial pressure of carbon dioxide and blood pH, concentration of Na+ and K+ and blood urea in a patient’s capillary blood sample , hemoglobin concentration and hematocrit.
To carry out analysis using the GASTAT-mini portable blood gas and electrolyte analyzer, the following is required: a capillary blood sample with a volume of 0.5-1 ml; analysis execution time - 180-270 s; performing calibration before measurement (the calibrator is built into the sensor cartridge); heating a blood sample (the device has a built-in thermostat); compliance with operating conditions: temperature 10-30°C, humidity 30-80%.
I would like to note that preclinical laboratory diagnostics of chemical homeostasis indicators allows the use of computerized modular diagnostic and treatment systems at the prehospital stage.
The use of “pocket” reference computers makes it possible to optimize medical care and transfer the diagnosis and treatment of acute emergency conditions from the sphere of empirical to the sphere of evidence-based medicine.
Thus, the level of glycemia and blood alcohol content are highly specific signs that allow acute alcohol poisoning and withdrawal syndrome to be differentiated from other conditions that do not require hospitalization in the intensive care unit in patients suspected of abusing alcohol at the prehospital stage. Moreover, determining blood glucose levels is a priority task in organizing targeted symptomatic treatment of any emergency conditions with impaired consciousness.
Modern methods of express diagnostics (for example, immunochromatographic indicator strip "ALKOSKRIN" for determining alcohol in saliva, produced by Progressive Bio-Medical Technologies LLC, (Moscow); indicator strip for determining alcohol in saliva "ALCOSENSOR", portable analyzer of gases and electrolytes blood GASTAT-mini) allow you to determine the alcohol content in saliva and, accordingly, in the blood with a sufficient degree of accuracy.
E. I. Vovk, Candidate of Medical Sciences, Associate Professor MGMSU, NNPOSMP, Moscow
For questions regarding literature, please contact the editor.
Future plans
In each microdistrict there were modern “candle” houses, which were used to consolidate the previous buildings. Will they continue to be built?
— Neighborhoods east of the street. Angarskaya are fully formed,” said Daria Davidovich, head of the architecture and construction department of the Zavodsky district administration. — There are no plans for their further development. New houses will appear only on the site of the former correctional colony within the boundaries of the intersection of the street. Angarskaya and Magnitnaya.
Photo by Pavel Rusak
See also:
Published: 11/27/2021