Manifestations of headache and accompanying symptoms
We call any pain in the head area a headache, but the mechanism of its occurrence varies. It is caused by irritation of pain receptors in the dura mater, as well as blood vessels, nerves - trigeminal, glossopharyngeal, vagus, skin nerves, head muscles, cervical spinal roots. It can also manifest itself in different ways: it can be dull, pulsating, squeezing, bursting; can concentrate in the forehead, temples (on one or both sides), back of the head, crown of the head. Attacks can be strong, moderate or weak, and vary in duration and frequency. Pain may be accompanied by other symptoms (nausea, vomiting, visual disturbances, dizziness, increased or decreased blood pressure, etc.). All these characteristics are important for making a diagnosis.
Diagnostics
If you regularly experience discomfort in your temples and dizziness, you should definitely consult a doctor. If there are signs of vascular diseases, you should make an appointment with a cardiologist; in other cases, a consultation with a neurologist is indicated. If it is not possible to measure blood pressure or the nature of the symptoms does not allow you to independently figure out which specialist’s help is needed, it is better to initially consult a therapist. A general practitioner will help determine the cause of the problem and, if necessary, refer the patient to a specialist.
Initially, a survey of the patient is carried out, during which the characteristics of pain in the temples, the circumstances of its occurrence, the type of dizziness and the nature of other symptoms present are established. The doctor must examine the patient, measure blood pressure and, if necessary, perform neurological tests, which helps narrow the list of possible causes of poor health.
For accurate diagnosis of pathology and assessment of the severity of changes, the following may be prescribed:
- X-ray of the cervical spine;
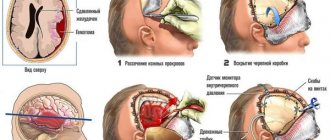
- CT scan of the brain and skull;
- MRI of the brain and cervical spine;
- CT angiography;
- Ultrasound scanning of the vessels of the neck and head;
- 24-hour blood pressure monitoring;
- electroencephalography (EEG);
- UAC, OAM.
Causes of headaches
There are primary and secondary headaches. Primary pain is considered to be pain that is not an accompanying symptom, but is an independent disease. In this case, it is the headache that is the main problem. Secondary headache is one of the manifestations of a disease that is not limited to headache. Severe headaches can be accompanied by infectious diseases and poisoning of various natures (both toxic substances entering the body from the outside and those produced inside the body, for example, toxins that are formed as a result of the activity of viruses and pathogenic microbes in the body). A headache can occur as a result of stress, weather changes, hypothermia or overheating of the body, lack of sleep, hunger, overeating, lack of oxygen - the cause can be anything that leads to disruption of the metabolism necessary for brain activity.
So, if you have a headache, it does not necessarily mean that you are sick: it may simply be the result of a random factor. However, if the headache occurs periodically or persists for a long time, then most likely there is some kind of disease. In 95% of such cases, there is a primary headache, and only in 5% of cases is it secondary.
Primary headache. Major diseases.
The most common forms of primary headache are “tension pain” and migraine, more rarely – cluster headache and other forms.
Tension headache (TTH)
can occur in anyone. This is the most common form of headache and is often characterized as a “normal” or “regular” headache. Attacks can last from 30 minutes to several days. The frequency of attacks varies from person to person, and it can also vary from one person to another during different periods of his life. The pain is described as squeezing, squeezing the head like a hoop or tight hat, usually bilateral, and moderate. In some people it can become chronic (chronic pain is diagnosed if there are more days with a headache than without it). A person experiencing chronic headaches becomes irritable. Weakness, fatigue, decreased appetite, and sleep disturbances may occur. The cause of TTH is physical tension in the muscles and ligaments of the head and neck - the so-called “muscle stress”, which can be a consequence, for example, of working in an uncomfortable position. TTH often occurs in those who work at a computer or whose work involves the need to look at details (jewelers, watchmakers, assemblers of electronic equipment, masters of artistic embroidery, etc.). The emotional factor is also important: emotional tension caused by stress or a state of increased anxiety can also lead to pain.
Migraine
characterized by severe and painful attacks of headache, which are often accompanied by nausea (and in some cases vomiting), as well as intolerance to light and sound. The perception of smells changes, thermal sensations are disrupted. Migraine attacks last from 4 hours to 3 days and can be repeated with a frequency of 1-2 times a year to several times a month. During an attack, so-called “precursors” may be observed - irritability, depression, fatigue, occurring several hours or even days before the onset of pain. In a third of cases, pain is preceded by phenomena called “auras”: 10-30 minutes before the attack there may be visual disturbances (blind spots, flashes, zigzag lines in front of the eyes), tingling and numbness starting from the fingertips and spreading up the body and etc.
Predisposition to migraine is congenital and is associated with disorders in the brain structures responsible for pain and other sensations. Every seventh adult suffers from migraines, with women three times more likely than men. In girls, migraines usually begin during puberty.
Factors that contribute to the development of migraine attacks: chronic fatigue, anxiety or stress, in women - menstruation, pregnancy and menopause.
But a predisposition to seizures does not mean that an attack will definitely happen. There are factors that act as a “trigger” for an attack. An attack can be triggered by: skipping meals, insufficient fluid intake, certain foods, sleep disturbances, physical activity, changes in weather, sudden changes in emotions.
Cluster (or beam) headache
characterized by one-sided sharp (“dagger” or “drilling”) pain. The intensity of the pain rapidly increases within 5-10 minutes, and the attack itself lasts from 15 minutes to 3 hours, during which the patient cannot find a place to rest. The pain is usually localized in the eye area, and the eye may become red and watery. Recurrent attacks form a cluster (that is, they follow each other), the duration of the cluster is from 6 to 12 weeks. This form of pain occurs five times more often in men than in women. However, those who smoke a lot or have smoked in the past are more susceptible to it.
Treatment
Conservative therapy
Therapeutic tactics are determined taking into account the cause of the symptom. The basis is medicines, which in some cases are supplemented with non-drug methods:
- Migraine
. The attack is stopped with the help of non-narcotic analgesics and caffeine-containing drugs. Sometimes therapeutic blockades are performed. Very intense pain and prolonged attacks are indications for the use of triptans. For repeated vomiting, medications are administered subcutaneously, used in the form of sprays or rectal suppositories. - Cluster headache
. To eliminate paroxysm, triptans are prescribed, oxygen inhalations are performed, and local anesthetics are applied to the nasal mucosa. As part of prevention, calcium channel blockers are recommended; in case of intolerance, antiepileptic drugs or glucocorticosteroids are recommended. - Paroxysmal hemicrania
. The effectiveness of non-steroidal anti-inflammatory drugs, sometimes steroids, and calcium channel blockers is noted. Due to long-term use of painkillers, damage to the gastric mucosa is possible, so patients are additionally prescribed antacids and proton pump blockers. - Hypnic headache
. There is no uniform treatment regimen. It is possible to use lithium and melatonin preparations, hypnotics, benzodiazepines, NSAIDs, steroids and caffeine-containing drugs. - Vertebrobasilar system syndrome
. The treatment regimen includes medications with vascular, hypotensive and neuroprotective effects, anticoagulants, antiplatelet agents, and antidepressants. Non-drug therapy includes hyperbaric oxygenation, exercise therapy, vestibular exercises, massage, post-isometric relaxation, and magnetic laser therapy. - Arachnoiditis
. Anti-inflammatory, antiepileptic, absorbable, antiallergic and dehydration agents, metabolites, neuroprotectors, tranquilizers, and antidepressants can be prescribed. - ENT pathologies
. Antibacterial therapy, antihistamines and vasoconstrictor medications, immunocorrectors, UHF, and diadynamic currents are indicated. For sinusitis, punctures and sinus evacuation are performed; for mastoiditis, paracentesis of the tympanic membrane is performed.
Surgery
Patients with primary cephalgia do not require surgery. Surgical techniques can be used in the following cases:
- Insufficiency of vertebrobasilar blood flow
: carotid-subclavian bypass, endarterectomy. - Brain tumor
: removal of a tumor using microsurgical techniques or stereotactic radiosurgery methods, shunt operations for hydrocephalus. - Diseases of the ENT organs
: open and endoscopic maxillary sinusotomy or frontotomy, mastoidotomy, sanitizing and general cavity interventions on the middle ear. - Spinal lesions
: laser vaporization, microdiscectomy, interbody fusion, fixation with cages.
Secondary headache and diseases in which it occurs
In general, primary headache, although it disrupts the normal course of life during attacks, does not have serious consequences for a person’s general health. And secondary pain, despite the fact that it occurs much less frequently (in 5% of cases), can be a consequence of a dangerous disease.
Headache is necessarily present among the symptoms of the following diseases:
- vegetative-vascular dystonia (headaches can be combined with dizziness, nausea, fluctuations in blood pressure);
- hypertension (pain is mainly localized in the occipital region, there may be dizziness, noise in the head, spots before the eyes, heat in the head, pain in the heart);
- stroke;
- traumatic brain injury;
- meningitis;
- encephalitis;
- eye diseases (for example, glaucoma);
- diseases of the ear and nasopharynx (otitis media, sinusitis);
- neuralgia;
- diabetes;
- renal failure;
- oncological diseases.
Methods for diagnosing pain in the left hemisphere
To determine why the left side of your head hurts, you will need a full examination. Neurologists diagnose diseases that can lead to this symptom. According to their recommendations, a number of examinations are carried out, the results of which can be informative in determining the cause of the headache and making a diagnosis:
- collecting medical history data - it is important for the doctor to know about the conditions for the occurrence of headaches, its nature and strength, as well as the patient’s lifestyle and habits, old injuries and diseases;
- Ultrasound examination of cerebral vessels (Dopplerography) is a method by which you can evaluate the speed of blood flow and the degree of filling of blood vessels;
- encephalography is a technique that allows you to examine the functional activity of the brain;
- MRI is one of the main diagnostic methods, more often used to identify tumors, but it is also informative for other pathologies.
At the Clinical Brain Institute you can undergo a full examination and determine the cause of your headache. The test results will show a complete clinical picture, on the basis of which it will be possible to select an individual treatment and prevention regimen.
When should you see a doctor for a headache?
Many people prefer to simply take popular painkillers and not see a doctor. However, self-medication can lead to excessive use of such drugs, which can cause gastritis, peptic ulcers, as well as chronic headaches caused by taking medications. In addition, without undergoing a medical examination, you may miss the development of a dangerous disease. And a momentary effect obtained with the help of a random drug will still not be a solution to your problem.
You should definitely consult a doctor:
- if pain occurs for the first time in life (especially important for people over 50 years old);
- with very severe headaches;
- if the pain continues for a significant time (more than a week);
- if the pain intensity increases over time;
- when a headache occurs or worsens after a change in position or sudden movement of the head;
- if there are cases of loss of consciousness, memory impairment, changes in personal qualities;
- if the pain does not go away after taking antipyretic and painkillers.
Which doctor should you see if you have a headache?
If you complain of a headache, you should first contact your physician. To make it easier for the doctor to understand your disease, it is advisable to prepare answers to the following questions before visiting the doctor:
- How long has the pain been present?
- How often do the attacks recur?
- How long do they last?
- How severe is your pain (mild, moderate, severe, intolerable)?
- What is its character (pressing, bursting, pulsating)?
- In what part of the head is the pain concentrated?
- Are there any accompanying symptoms and what are they?
- At what point does pain occur (what contributes to its occurrence)?
- Do you manage to relieve pain (prevent attacks) and how do you do it?
- Do your relatives have similar complaints?