Symptoms of the disease
If we talk about the symptoms of atherosclerotic cardiosclerosis, it should be noted that this disease does not have its own symptoms. It usually manifests itself already at the progression stage. Then a person can observe manifestations of ischemic heart disease in the atherosclerotic form of cardiosclerosis:
- pain behind the sternum, which can radiate to the left arm;
- repeated heart attacks;
- shortness of breath, which can occur even when walking;
- cough due to pulmonary edema;
- increased fatigue;
- attacks of cardiac asthma.
When the patient also has heart failure, edema will be added to the considered clinical picture of the atherosclerotic type of cardiosclerosis.
Diagnostic methods
In order for the doctor to make an accurate diagnosis, the patient must undergo a complete examination. It begins with collecting an anamnesis. At this stage, it is important to provide the most complete information about all existing symptoms, as well as hereditary predisposition to cardiovascular diseases, if any. This will be followed by instrumental diagnostics, which will consist of the following:
- ECG - this diagnostic method is considered the most basic, because it is characterized by maximum information content. It will show cardiac arrhythmias, ventricular hypertrophy, post-infarction scars;
- Ultrasound – allows you to evaluate the contractility of the heart and obtain accurate information about its size;
- bicycle ergometry - will allow you to assess the degree of dysfunction of the heart muscle, as well as obtain information about the functional reserves of the heart.
Laboratory blood tests will also be required. They will allow you to estimate the amount of fat, including cholesterol, which most often contributes to the formation of atherosclerotic plaques on the walls of blood vessels.
Atherosclerotic cardiosclerosis
Structural heart diseases, accompanied by impaired pumping function of the organ, are a common cause of death. Particularly dangerous is the lack of blood supply to the muscular lining of the heart, which often leads to the development of diseases such as coronary artery disease, atherosclerotic cardiosclerosis and myocardial infarction. In this case, treatment of the heart vessels is a priority. We should not forget that atherosclerotic cardiosclerosis is a progressive pathology.
Atherosclerotic heart disease
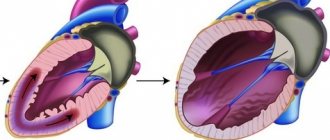
In the medical literature, atherosclerotic cardiosclerosis is a structural pathology characterized by the gradual replacement of the muscular lining of the heart with connective tissue cells against the background of progressive hypoxia. There are many causes of this pathology, but atherosclerotic lesions of the coronary arteries are the main etiological factor. Atherosclerotic cardiosclerosis can cause dangerous complications such as heart failure and heart attack.
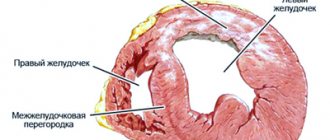
The human heart is a powerful four-chambered muscular pump that supplies all cells of the body with nutrients and oxygen. The constant movement of blood in the vessels is supported by rhythmic contractions of the myocardium. The muscular lining of the heart also requires a constant flow of blood, since cardiomyocytes are not able to accumulate enough oxygen to function autonomously. Even a slight decrease in blood flow to the myocardium leads to progressive changes and disruption of pumping function. The longer ischemia develops, the more dangerous the consequences of such a disease.
Atherosclerotic cardiosclerosis is not always considered an independent disease. As a rule, this is a consequence of a long course of coronary heart disease (CHD), inflammatory and autoimmune processes. However, replacement of normal cardiomyocytes by dysfunctional scar tissue is a major cause of myocardial dysfunction. To eliminate this pathology, first of all, treatment of the root cause of organ hypoxia is required.
8
24/7
Possible reasons
The main factor contributing to the development of cardiosclerosis is insufficient oxygen supply (hypoxia) to the muscle cells of the heart. Secondary factors include inflammatory and infectious processes, autoimmune diseases and organic myocardial damage. Under hypoxic conditions, myocardial cells first change and stop contracting, and then are destroyed.
Main reasons:
- Atherosclerosis of blood vessels is the gradual growth of fatty plaques on the inner walls of the arteries, causing a narrowing of the lumen of the vessel and a decrease in blood flow. Plaques form due to blood lipid imbalance, poor nutrition, vascular damage and other factors. With atherosclerotic disease of the coronary arteries that supply the heart, myocardial hypoxia develops.
- Coronary heart disease is a consequence of narrowing of the blood vessels of the heart. This may be atherosclerosis, dysregulation of tone, or a congenital anatomical defect of the arteries. IHD is a progressive disease that causes gradual replacement of cardiomyocytes with connective tissue. Atherosclerotic cardiosclerosis, in which angina pectoris occurs quite often, has a common mechanism of occurrence with ischemic heart disease.
- Coronary artery thrombosis is a partial or complete blockage of blood vessels.
- A heart attack is a sudden cessation of blood supply to the heart, accompanied by focal or diffuse destruction of cardiomyocytes. Destroyed muscle cells are also replaced by connective tissue.
- Pathologies of connective tissue, characterized by excessive proliferation of fibroblasts or the appearance of abnormal proteins.
Doctors are not always able to identify the real cause of atherosclerotic myocardial disease in a patient. Pathology is often detected in late stages.
Risk factors
Atherosclerotic cardiosclerosis of the heart can progress even faster under the influence of negative factors that are not the direct cause of the disease. This may be an unhealthy lifestyle, primary disorders of the cardiovascular system and other phenomena.
The main risk factors include:
- Pathologies of the heart and blood vessels in a family history.
- High blood pressure.
- Obesity and sedentary lifestyle.
- The predominance of fatty foods in the diet.
- Blood lipid imbalance (high concentration of bad cholesterol).
- Diabetes.
- Kidney diseases.
- Smoking and alcoholism.
- Use of drugs that affect the heart.
The listed factors largely determine the mechanism of development of almost any pathology of the heart and blood vessels.
Symptoms and signs
Atherosclerotic cardiosclerosis, the causes of which are usually associated with primary diseases of the heart and blood vessels, can manifest with various symptoms. First of all, these are symptoms of ischemic heart disease, myocarditis, heart attack or any other factor in the development of cardiosclerotic disease. In this case, the process of replacing cardiomyocytes with connective tissue practically does not manifest itself until the patient experiences myocardial dysfunction.
8
24/7
Possible manifestations of the disease:
- Constant fatigue, especially during physical activity.
- Hesitant breathing.
- Dizziness and headache.
- Loss of consciousness.
- Cardiopalmus.
- Feeling of heaviness in the chest area.
- Chest pain (angina pectoris).
- Swelling of the lower extremities and abdominal cavity.
- Pulmonary edema.
- Insomnia.
- Anxiety and fear.
- Violation of the rhythm of heart activity.
Thus, atherosclerotic cardiosclerosis masks its symptoms under ischemic heart disease and other primary diseases. As a result, cardiosclerotic changes are detected already at the stage of severe complications.
Diagnostic methods
Most often, atherosclerotic cardiosclerosis is an incidental diagnostic finding during a cardiac examination for ischemia, atherosclerosis or other diseases. Patients consult a cardiologist with complaints of angina, exercise intolerance, dizziness and other symptoms. The doctor reviews your history for risk factors and performs a physical examination. During listening (auscultation) of the heart and general examination, objective signs of myocardial dysfunction are often detected. The diagnosis of atherosclerotic cardiosclerosis is made based on the results of instrumental and laboratory methods.
Additional research:
- Electrocardiography – registration of the bioelectrical activity of the heart. To do this, special sensors are placed on the patient’s body connected to a cardiogram recording device. Based on the test results, one can judge the presence of a structural pathology that prevents the normal propagation of an impulse in the myocardium.
- Echocardiography is the main imaging method in cardiology. The doctor uses a transducer that sends high-frequency sound waves into the heart to produce an image. Monitoring the heart's performance on a monitor in real time allows you to detect the focus of cardiosclerosis and assess the degree of pumping dysfunction.
- Angiography – visualization of blood vessels. As a rule, this method is used to diagnose coronary artery disease, heart attack and atherosclerosis. Before taking the image, the doctor injects a contrast agent intravenously to improve the accuracy of the study. Based on the results of coronary angiography, one can judge the cause of cardiomyocyte hypoxia.
- Stress test - obtaining a cardiogram during increased heart activity. This test is most often used to diagnose hidden arrhythmia and pumping dysfunction.
- Holter study – recording of a cardiogram on an electronic device of a portable device within 24-48 hours. Before the study, the patient is instructed to keep a diary of well-being to clarify the time of occurrence of the arrhythmia. This is the optimal method for searching for manifestations of myocardial dysfunction.
- Cardiac biopsy – removal of a section of heart tissue followed by histological examination.
- Blood test for lipid profile, hormones, minerals and heart attack indicator enzymes.
- Computed tomography and magnetic resonance imaging are methods for obtaining high-resolution images of the heart and blood vessels. The images are often used to plan surgery.
- Radionuclide study - visualization of the heart with the preliminary introduction of radioactive isotopes into the bloodstream. The results of the study demonstrate the effectiveness of blood supply to the myocardium.
The abundance of diagnostic methods is justified by the number of possible etiological factors. To treat the disease, the doctor also needs to assess the degree of cardiosclerosis.
Treatment and prevention
Treatment should be aimed at eliminating the root cause of the pathology, restoring myocardial function and preventing the development of dangerous complications. Surgical and medicinal correction methods are used.
Prescribed drugs:
- Beta blockers to lower blood pressure and eliminate arrhythmias.
- Calcium channel blockers to improve blood supply to the myocardium.
- Aldosterone inhibitor to lower blood pressure.
- Diuretics to improve hemodynamics.
- Cardiac glycosides, statins and other drugs necessary to treat the cause of the pathology.
Atherosclerotic cardiosclerosis can rarely be eliminated with medication, but medications prevent the progression of the disease and eliminate symptoms.
Surgical methods:
- Implantation of a pacemaker or defibrillator.
- Correction of the coronary arteries to improve blood flow.
- Surgery for structural heart pathologies.
Prevention methods are also important. Giving up bad habits and fatty foods, losing weight, moderate physical activity and timely treatment of primary pathologies of the cardiovascular system helps prevent the development of irreversible changes in the heart. If symptoms of myocardial dysfunction appear, it is recommended to consult a cardiologist for examination.
8
24/7