Hepatic encephalopathy - symptoms and treatment
The diagnosis of “hepatic encephalopathy” is established by characteristic clinical manifestations, results of laboratory and instrumental studies and psychometric testing data. Further treatment tactics and prognosis of the disease will depend on the degree (stage) of the disease.
Diagnosis of stages I-IV of manifest (clinically pronounced) hepatic encephalopathy is not difficult, since each stage is characterized by certain symptoms [10]. It is much more difficult to recognize the disease at the initial stage: there are no clinical symptoms during a latent course, laboratory parameters are not changed. Therefore, psychometric tests are most often used to detect minimal hepatic encephalopathy.
Recognizing the hidden course of the disease is very important for two reasons:
- firstly, minimal hepatic encephalopathy is very common (50 to 70% of cases in liver cirrhosis);
- secondly, it can lead to a traumatic situation, especially while driving a car, since at this stage of the disease the patient does not respond adequately to extreme circumstances [10][16][17][18].
Hepatic encephalopathy can be suspected in patients with the following symptoms:
- inattention, memory impairment;
- inhibited thinking;
- decreased reaction speed;
- decreased performance;
- disturbance of visual perception;
- irritability.
Laboratory diagnosis involves determining the level of ammonia in arterial blood: it is elevated in more than 90% of patients with overt hepatic encephalopathy. However, during a latent course of the disease, the ammonia concentration may be normal, so this indicator is not an exclusion criterion when making a diagnosis [18].
| Degree of hepatic encephalopathy | Arterial ammonia levels |
| 0 | Norm |
| I | Up to 1.33 from ULN* |
| II | 1.33-1.67 ULN |
| III | 1.67-2 VGN |
| IV | More than 2 ULN |
| *ULN is the upper limit of normal, equal to 60 µmol/l | |
Psychometric testing is primarily used to diagnose clinically silent hepatic encephalopathy. The sensitivity of the tests is quite high - 70-80%.
Over the past 30 years, dozens of simple, accessible psychometric tests have been developed that can be used in various combinations. They are divided into two groups:
- tests for the speed of cognitive reaction (for example, the number connection test - the most common and well-known in clinical practice);
- fine motor accuracy tests (eg line copying test).
When conducting a number connection test, the patient needs to connect the numbers from 1 to 25 with a line. They are printed randomly on a sheet of paper.
To evaluate the test, the task execution time (in seconds), including time spent correcting errors, is used [18]. The interpretation of the results is given in the table.
| Time | Points | Disease stage |
| Less than 40 s | 0 | No |
| 41-60 s | 1 | 0-I |
| 61-90 s | 2 | I-II |
| 91-120 s | 3 | II |
| More than 120 s | 4 | II-III |
The following psychometric tests are also used in the diagnosis of hepatic encephalopathy:
- handwriting recognition test;
- numbers and symbols test;
- line copy test;
- visual memory test;
- alphabetical elimination test;
- linear maze test;
- dots and circles test;
- test for memorizing a pair of words;
- star construction test;
- sequential subtraction test;
- text retelling test, etc. [16][17][18].
Instrumental diagnostics are carried out using the critical flicker frequency (CFF) method. In 2002, it was first used to diagnose minimal hepatic encephalopathy. The study is carried out using the HepatonormTM hepatoanalyzer. In this device, the patient sees what seems to him to be a constant red glow, but is actually a high-frequency flickering [13][15].
During the FFM test, the frequency of the red light, which is initially 60 Hz and is generated as a high-frequency pulse, causes the patient to feel a constant light, and then changes to flickering over time. It is at this moment that the patient needs to press a button on the device. The hepatoanalyzer records the frequency at which the red beam “began to flicker.”
The study is carried out 8-9 times. The average value of the CFM is used for evaluation. Based on the test result, the stage of hepatic encephalopathy is established: values below 39 Hz correspond to minimal hepatic encephalopathy, 35.9-32 Hz - stage I, 31.9-28 Hz - stage II, below 27.9 Hz - stage III [15].
Hepatic encephalopathy can also be diagnosed using EEG - electroencephalography. However, the validity of the results of this study may be affected by medications or decreased sodium levels in the blood [21].
If intracerebral hemorrhage is suspected or differential diagnosis is necessary, CT and MRI of the brain may be required [21].
Differential diagnosis
When diagnosing hepatic encephalopathy, it is important to exclude other causes that could cause the same clinical symptoms. Such reasons include neurological, somatic diseases and various intoxications.
Differential diagnosis is complicated by the lack of distinctive symptoms that would be found only in hepatic encephalopathy. The American Association for the Study of Liver Diseases recommends that disorders that also alter the level of consciousness be considered when making a diagnosis. These include:
- metabolic encephalopathy - associated with metabolic or electrolyte disorders, characterized by low levels of sodium and potassium in the blood or hypoglycemia;
- alcoholic encephalopathy - accompanied by intoxication, withdrawal syndrome (abstinence), developing Wernicke encephalopathy is associated with vitamin B1 deficiency;
- drug encephalopathy - caused by taking benzodiazepines, antipsychotics and opioids;
- neuroinfections - occur under the influence of bacteria, viruses, fungi or protozoa;
- intracranial hemorrhage , subdural hematoma , stroke , tumor or brain abscess - develop against the background of congenital or acquired diseases associated with circulatory disorders [10][13][18].
Total information
Liver pathology is extremely rarely complicated by hepatic encephalopathy. However, if the disease is nevertheless detected, its outcome is almost always tragic: for 2/3 of those affected, encephalopathy ends in death. Chronic liver diseases are more often complicated by hepatic encephalopathy than acute ones. They are potentially reversible, but significantly affect the patient’s ability to work and lifestyle.
Modern medical science does not yet have a clear idea of the causes of the development of the disease, but recent research allows us to hope for a solution to this problem in the near future. Discovering the mechanisms of the disease will contribute to the development of an effective treatment plan that will not only reduce the number of deaths, but will significantly improve the quality of life of those affected.
Sources
- I. L. Klyaritskaya Hepatic encephalopathy. 2005. Crimean therapeutic journal;
- Polukhina A.V., Khaimenova T.Yu., Vinnitskaya E.V. Hepatic encephalopathy: the problem of pharmacotherapy. 2021. Medical Council;
- Ivanikov I. O., Syutkin V. E. Hepatic (porto-systemic) encephalopathy. 2003. Practical medicine;
- Podymova Svetlana Dmitrievna New approaches to the pathogenesis, clinical picture, treatment of hepatic encephalopathy. 2021. Therapeutic Archive;
- Tsapyak T. A., Klopotiy E. V., Viltsanyuk I. A. Hepatic encephalopathy and the possibilities of its drug correction. 2007. Crimean therapeutic journal;
- Polunina T. E., Maev I. V. Hepatic (porto-systemic) encephalopathy. 2011. Medical advice.
Video from YouTube on the topic of the article:
Causes of pathology
The appearance of encephalopathy can be provoked by:
- acute liver disease;
- entry of neurotoxins into the circulatory system;
- cirrhosis of the liver.
Factors contributing to the development of the disease: hepatitis of all types (alcoholic, fatty, toxic, viral), oncology, drug or toxic intoxication, other diseases accompanied by hepatocytolysis.
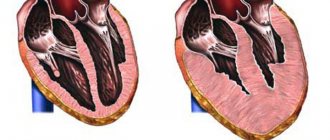
An excessive increase in the microflora of the obligate intestine or the consumption of excess amounts of protein-rich food can trigger the entry of intestinal neurotoxins into the circulatory system. Liver cirrhosis, complicated by hepatic encephalopathy, is accompanied by the formation of scars (replacement of healthy liver tissue with connective tissue), inhibition of all basic liver functions.
The following factors can provoke the death of hepatocytes and toxic damage to brain cells:
- internal bleeding;
- taking hepatotoxic drugs (without medical supervision and adequate supportive therapy);
- constipation, protein dyspepsia;
- surgical interventions or serious injuries;
- peritonitis provoked by ascites;
- bacterial, viral diseases.
Liver failure is accompanied by a list of pathological changes:
- disturbance of homeostasis, CBS;
- changes in oncotic and hydrostatic pressure.
These changes significantly disrupt the normal functioning of astrocyte cells, which account for approximately a third of the weight of brain tissue. Astrocytes are responsible for the normal regulation of the permeability of the cellular barrier, which ensures complete exchange between brain tissues and blood, removing toxins and ensuring the supply of nutrients to brain cells.
In addition to ammonia, toxic damage to astrocytes can cause exposure to false neurotransmitters, magnesium, as well as breakdown products of protein and fatty acids.
Forms of the disease
Depending on the etiological factor, several types of hepatic encephalopathy are distinguished:
- type A – caused by acute liver failure;
- type B - caused by the release of neurotoxins from the intestines into the bloodstream;
- type C – associated with cirrhosis of the liver.
Based on the rate of increase in symptoms, hepatic encephalopathy is divided into two forms:
- acute – develops rapidly, accompanied by severe mental disorders;
- chronic – symptoms increase slowly over months, and sometimes even years.
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Dyachenko Ksenia Vasilievna
Head of the center for the treatment of dizziness and balance disorders.
The doctor is a neurologist of the highest category.
Angioneurologist. Neurorehabilitation specialist. Physiotherapist. Candidate of Medical Sciences.
Experience: 19 years.Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
Therapy
Therapy for this disease is a complex process that requires as quickly as possible clarification of the causes of its occurrence. The course of treatment includes: diet therapy, bowel cleansing, lowering nitrogen levels and symptomatic therapy.
It is necessary to reduce the amount of protein coming from food. It is necessary to adhere to this diet for a long time, since an increase in the amount of protein in the diet of a cured patient can provoke a relapse of the disease.
To speed up the excretion of ammonia in feces, it is necessary to achieve at least two bowel movements per day. For this purpose, cleansing enemas are used.
Antibacterial therapy involves taking antimicrobial drugs, the action of which is especially effective in the intestinal lumen (vancomycin, metronidazole, neomycin).
To achieve a sedative effect, benzodiazepine drugs are used, with preference given to haloperidol.