- devices measuring eye pressure
- non-contact blood pressure monitors
- contact tonometers
- pneumatic VOP devices
- stationary or portable meters?
Intraocular pressure is a separate parameter that characterizes the force of pressure of the fluid contained inside the eyeball on the walls of the organ.
Intraocular pressure must be measured for people over 40 years of age, even if they have no obvious complaints about this. The need for regular checking of intraocular pressure is caused by the fact that due to its excess, serious pathologies of the organs of vision can develop. The most dangerous disease associated with IOP disorders is glaucoma. In later stages, it can lead to complete loss of visual function. In addition, eye tonometry is performed to monitor the prescribed treatment and monitor the dynamics of recovery after surgery.
Ophthalmotonus - why is it so important?
A change in ophthalmotonus should be considered an alarming symptom that indicates pathological processes in the functioning of the visual organs.
Increased intraocular pressure is a consequence of disturbances in the outflow of fluid that is located under the membrane of the eye. Circulation becomes impossible due to the presence of plugs in the tubules that drain fluid. Moisture gradually accumulates, which leads to increased pressure on the shell.
High pressure inside the eye causes pressure on the fundus vessels. As a result, the retina is injured and the photosensitive elements die. Compression of the optic nerve is also observed, which threatens to disrupt the delivery of oxygen and nutrients to cells. If this happens over a long period of time, the tissues of the organ atrophy, vision gradually decreases and, as a result, disappears completely.
Reduced ophthalmotonus also indicates the development of pathological processes. Low pressure leads to a deterioration in the blood supply to the organ, due to which the tissues atrophy and the eyes gradually cease to see.
Changes in ophthalmotonus may result from problems in the functioning of certain organs and systems. Thus, high intraocular pressure is often observed in people with heart and vascular diseases, and low intraocular pressure may be a concomitant sign of liver failure or the initial stages of retinal detachment.
Contraindications
The main contraindications include:
- progressive corneal defects;
- state of alcohol or drug intoxication;
- external influence, injuries resulting in destruction of the membrane of the organ of vision;
- allergy to anesthetics;
- diseases of a bacterial or viral nature (it is possible to perform a tonometry procedure after completion of the course of treatment);
- severe migraine, pain in the eyes;
- diseases of the endocrine system, neurological.
It should be noted that the described contraindications apply only to contact research methods. Non-contact tonometry can be used even in the presence of relevant diseases. Next, we will consider in detail the main methods of tonometry.
Indications for measuring IOP pressure
Ophthalmologists measure eye pressure based on patient complaints. Key symptoms of concern include:
- changes in visual acuity;
- feeling of a film on the eyes;
- recurrent headaches that occur in the temporal region and around the eyes;
- rapid eye fatigue;
- poor vision in low light conditions;
- redness of the eyes;
- pain when concentrating on a specific object;
- painful sensations that occur during eyelid movement;
- dry eyes;
- narrowing of visual fields;
- change in the shape of the pupil.
For 40-year-old patients, eye pressure is measured without fail, regardless of whether they have complaints or not. Monitoring of ophthalmotonus in such people is performed at least once a year.
In patients with glaucoma, ophthalmotonus is measured at least once every three months. If a person has a genetic predisposition to the disease, but there are no complaints about the functioning of the visual organs, for prevention, intraocular pressure is measured at least once every two years.
How to measure correctly
To know how to determine eye pressure yourself, you should follow certain recommendations:
- You need to constantly monitor your blood pressure when you feel unwell. For timely detection of deviations in intraocular pressure, measurements are required 4-5 times a week.
- Patients who suffer from hypertension should measure their blood pressure daily.
- When doubt arises about the correctness of the results, the procedure is repeated after 5 minutes.
- During manipulation, you need to ensure that the device lies flat and its tubes are not twisted.
Before the procedure, it is prohibited:
- Drink coffee or smoke.
- Exercise.
- Take a hot bath or visit a sauna.
- Be exposed to ultraviolet radiation for a long time.
- Eat a lot of food.
To know how to determine eye pressure, you need to consult a specialist, since incorrect actions will affect the indicators.
Diagnostic methods
Ophthalmologists use tonometric and tonographic methods not only to diagnose glaucoma and determine an effective treatment strategy for the disease, but also to monitor the dynamics of the pathology and identify complications.
Techniques for measuring intraocular pressure vary, the main ones being:
- palpation;
- instrumental research (conducted both contact and non-contact).
Measuring ophthalmotonus by palpation
The method is one of the simplest. It is used when the patient has contraindications to the use of instrumental diagnostics, or the correctness of the information from the instrumental examination is in doubt. Most often, palpation is used when the examination is carried out on an injured cornea or after eye surgery.
During palpation, the specialist evaluates how elastic the membrane of the eye is. He draws conclusions based on the degree of deformation when exposed to ocular structures.
There are several options for conducting such a survey:
- the specialist palpates the eyeball directly during surgery after the administration of anesthesia;
- transpalepebral palpation is performed, when the doctor, with the patient’s eyelids closed, determines the hardness of the eyes by gently squeezing the area above the eye cartilage with the fingers of both hands.
Conclusions about the level of ophthalmotonus can also be drawn from the characteristics of the sclera's reaction to external influences. If the intraocular pressure is normal, but as the sclera is compressed, obvious tremors will be felt. With high IOP, the degree of pressure must be increased, and the force of the push decreases.
Diagnostics of IOP pressure using instruments
In ophthalmological practice, a wide range of contact devices is used to perform eye tonometry. Their main advantage is the provision of results with a minimum degree of error, which does not exceed 1 mm Hg. But such devices also have significant disadvantages. First of all, the risk of infection increases. Often, to conduct a study, it is necessary to first anesthetize the treatment field. The use of such devices in diagnosing children is limited, since it is difficult for children to remain still and calm during the procedure. Because of this, there is a high risk of eye injury.
One of the common ways to perform contact tonometry is using the Maklakov apparatus. The procedure is characterized by simplicity, accurate results and relatively low cost.
Non-contact measurement of intraocular pressure
Devices for non-contact changes in intraocular pressure have a simple design, so they can be used even at home. The peculiarity of the technique is that the procedure is performed without contact with the surface of the eyes, therefore, the probability of infection is zero. In this case, the patient does not experience pain or discomfort during the examination.
The non-contact device for measuring ophthalmotonus operates almost instantly. It takes a few seconds for the device to produce results. Using them, the doctor can determine the presence of risks for the development of certain ophthalmological pathologies.
The procedure for measuring intraocular pressure using a non-contact method is carried out as follows: the patient places his head on a stand, its position should be fixed, and then looks through a special window, concentrating his gaze on the white spot. At this time, the device produces a powerful stream of air and records how it affects the shape of the cornea. It is from these changes that conclusions about intraocular pressure indicators are drawn.
Despite the fact that the non-contact method of eye tonometry is considered the safest, the accuracy of the results using the Maklakov method is still higher.
What's pressing on your eye?
The structure of the eye has a complex structure, but it is not necessary to study it all in detail to understand what intraocular pressure is and why it suddenly deviates from the norm. It is enough to imagine the eye as a liquid surrounded by multiple membranes. The outer one is the sclera, behind it is a network of blood vessels, and even deeper is the ciliary body. When the muscles contract, the shape of the lens changes and the person can see something up close. But this is not the only function of the ciliary body.
Another important task assigned to it is the secretion of intraocular fluid. By circulating between the various chambers of the eye, it ensures normal metabolism and maintains a certain level of intraocular pressure (IOP). In other words, the fluid secreted by the ciliary body constantly puts pressure on the eye, setting the parameters of its normal size and shape. As soon as the amount of this fluid increases excessively or there are problems with its outflow, the pressure will jump. This will entail distortion of the shape, and, consequently, of the entire optical system of the eye.
Important! Intraocular pressure directly affects the quality and acuity of vision. When it deviates from the norm, the shape of the eyeball changes and the mechanisms of accommodation that allow close vision are disrupted.
Measuring IOP at home
Patients with glaucoma in extreme stages are advised to monitor eye pressure throughout the day. To perform such measurements, special portable instruments are used. One of them is the ICare device. It helps determine the degree of ophthalmotonus by applying special replaceable sensors to the cornea of the eye.
Among the advantages of this technique are:
- minimal error in the obtained data;
- efficiency of the procedure;
- no negative consequences for the cornea;
- patient comfort during the examination;
- eliminating the risk of infection.
Since the device has a memory function and stores the results of the last 10 measurements, this increases the convenience of monitoring changes.
Interpretation of measurement results
Normal pressure is approximately equal in both eyes. The permissible difference in measurements should be no more than 3-4 mm Hg. Art. If the difference is greater than this value, then we may be talking about the early stages of glaucoma development.
As a person gets older, intraocular pressure changes, but these changes are minor. For example, in 20-year-old patients, IOP increases with age, and after reaching 70 years, on the contrary, it decreases.
Main pressure is an important criterion for determining the overall health of the eyes. If abnormalities occur, IOP should be measured regularly to avoid complications. Today, doctors have a huge arsenal of tools and methods that allow them to perform such studies. The most widely used are non-contact tonometry methods that exclude direct contact with the eye. Since science does not stand still, methods and equipment for measuring IOP are constantly being improved, making the process even safer and the results as accurate as possible.
Professional devices measuring eye pressure
Measuring intraocular pressure is a mandatory step in any ophthalmological examination. To accurately determine this indicator, an eye tonometer is used. The principle of operation of any of its varieties is based on measuring the level of deformation of the eyeball under the influence of a strictly dosed external factor.
Using this device, the doctor quickly, accurately and painlessly performs the studies necessary to make a diagnosis. The use of a tonometer does not create any discomfort even in patients with increased sensitivity of the cornea.
Non-contact devices for measuring IOP
The most convenient, informative and hygienic method for the patient is a non-contact examination. The directed air flow causes the cornea of the eye to bend. The change in curvature is recorded and processed by a computer program, which produces an accurate result. The method does not cause any discomfort in the patient and is completely safe, as it eliminates accidental damage to the eye or infection.
The procedure for examining the fundus using a non-contact method
- The patient sits on a chair and takes a comfortable position that allows him to remain still for some time.
- The patient's head is fixed in a certain position, the gaze must be kept at a certain point indicated by the doctor.
- The ophthalmologist asks the patient to open the eyelids as wide as possible to increase the area exposed to the air flow.
- The doctor turns on the device, and an air stream begins to flow from the nozzle opposite the eye. The device records the air pressure at which the cornea bends, as well as the degree of its deformation.
- After computer processing, the equipment shows the level of pressure inside the eye.
Characteristics of non-contact tonometers
Let's consider the most important characteristics of the device:
- Range. Popular models are single-range tonometers that perform measurements ranging from 5 mmHg. up to 50 mm Hg
- Error. A deviation of no more than 0.1 mmHg is considered acceptable.
- Trigger. Depending on the design, the meter is triggered automatically during applanation or by a signal given by the doctor. The most convenient models are those that combine both methods.
- Lighting. To reliably record corneal smoothing, the sensitivity of the optical system provided by the illumination is important. A powerful LED, white or red, is used as a light source.
- Working distance. In all tonometers, the optimal distance is 20 mm. You can move your eye a little closer to the meter, but it is not recommended to exceed the specified interval.
- Location. There are stationary, portable and manual models. Stationary ones are usually installed on a special table or mounted on the wall. Portable and hand-held devices are commonly used during home visits. In the process of measuring intraocular pressure, they are placed on a suitable surface or held in the hands.
- Print information. Modern models are often equipped with a high-speed thermal printer for instant printing of results.
- Display. Screen size is an important parameter that ensures ease of use of the device. Practice shows that if the display diagonal is less than 5 inches, reading measurement results becomes difficult.
- Product weight. A medium-sized stationary ophthalmic tonometer weighs about 18 kg. The weight of the manual model is approximately 1 kg.
Features of choosing a device for measuring pressure
An extensive range of eye tonometers allows you to make the optimal choice taking into account the working conditions of an ophthalmologist.
- Stationary ones are installed in specialized ophthalmology offices in order to properly equip the workplace of the doctor who receives patients. The device is mounted on the wall so that it is convenient to examine a patient sitting on a chair, or installed on the ophthalmologist’s desk. Such devices are characterized by high accuracy, ideal automatic centering, versatility, and a wide operating range.
- Portable meters that allow you to monitor the patient's current intraocular pressure are used primarily in ophthalmic operating rooms.
- Hand-held tonometers are indispensable in the practice of ophthalmological consultants. A small device, comparable in size to a regular ballpoint pen, allows you to measure the level of fundus pressure in any setting, including at the patient’s home. For certain diseases, patients themselves purchase such devices in order to monitor IOP fluctuations and take measures prescribed by the doctor to normalize it.
All of these categories provide measurement accuracy that is quite sufficient for diagnosing the vast majority of diseases associated with changes in pressure. Another distinctive feature of these devices is complete safety for the patient, which is ensured by the absence of direct contact with the working part of the product.
In addition to dimensions, models of ophthalmic tonometers differ in their sets of functions and capabilities, providing accuracy and speed of diagnosis. Additional options include a soft air shot. Devices equipped with this function do not cause patients the slightest discomfort during measurements. Modern devices provide the ability to connect to a computer to upload examination results to the local network of a medical institution.
The service life of a high-quality, reliable tonometer is at least five years, subject to daily active use.
Non-contact eye pressure measuring device 7CR Reichert (USA)
— operating modes: single “shot” and a series of three “shots”; — built-in printer; — data transfer via USB; — measuring range: 7 ~ 60 mm Hg. Art. (standard for tonometers ISO 8612);
Easy to use. Has maximum automatic guidance speed. The process of measuring IOP is comfortable and does not frighten the patient. There is no need for adjustment when positioning the patient. Intuitive color LCD touchscreen display. The best device in its series in terms of price-quality ratio.
Preparing for the examination
If you wear contact lenses, regardless of the type of examination, you must remove them before the procedure and do not use them for at least two hours after completion. You can get to the clinic wearing glasses. Also, after the examination, it is highly recommended not to touch your eyes with your hands.
Clothes with tight collars, ties and other accessories that put pressure on the neck should be avoided. This may well inflate the indicators, affecting the accuracy of the study.
4 hours before the medical procedure, reduce the amount of fluid you consume; you should also not abuse alcohol or use drugs at least 12 hours before the appointed time.
Women should not overdo it with cosmetics and use eye shadow and mascara. Be prepared that all methods, except non-contact, use anesthesia. Make sure you are not allergic to the anesthetic used in the clinic.
Apart from the above, additional preparation of the eyes for any type of examination is not required.
Contact intraocular pressure meters
With the contact method of diagnosis, the patient inevitably experiences unpleasant sensations, so before measuring intraocular pressure, an anesthetic solution is instilled into him. The advantage of contact measurements is the maximum accuracy of the results obtained. It allows you to diagnose diseases of the visual organs at a professional level and give an expert assessment of the patient’s condition.
There are several different ways to measure. The doctor chooses the most appropriate technique, taking into account the individual characteristics of the patient.
- Impression tonometry. The patient's head is fixed at a certain distance from the device, then a special plunger (rod) is gently pressed against the cornea. The impact is relatively painless, the measurement takes only a few seconds, so the method is usually used when examining children.
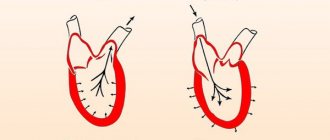
- Applanation method. The patient lies supine and opens his eyes wide, after which a weight with a flat bottom moistened with paint is placed on the surface of the cornea. Then the weight is pressed against the paper and the area of the spot in the center of the area is measured. The lower it is, the higher the pressure inside the eye.
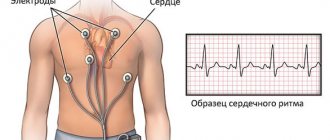
- Dynamic method. It is an improved version of applanation, as it eliminates the influence of corneal deformation on the result. The piezoelectric transducer is placed on the cornea and pressed with a constant force equivalent to one gram, while measuring the electrical resistance. The measurements last about 8 seconds. The method can be used to correlate intraocular pressure with heart rate.
After examining the patient, the contact part of the device must be disinfected to prevent the transmission of various infections. If the doctor's office does not have disinfection equipment, a non-contact tonometer should be selected for examining patients.
Contact eye pressure meter Icare (Finland)
— The professional model of Icare tonometers has advanced functions. — Icare Pro takes measurements in sitting, standing and lying positions. — Convenient for measuring IOP in children and patients in the operating room. — The device is equipped with a USB cable for transferring data to a computer. — Easy to use — has sound prompts. — Automatic saving of data from ten previous measurements. — Automatic display of measurement data on the screen.
Applanation tonometry
The first study in our review related to the group of contact methods. The method is recognized as the most accurate, which has given it widespread use in medicine. All techniques in this group are quite painful due to direct contact with the cornea, so local anesthesia is required.
Internal pressure is measured by applying a certain amount of force (applanate) required to create a flat surface area. When the colored base of the tonometer comes into contact with the cornea, the coloring enzyme is distributed along its boundaries. The resulting prints are transferred to paper and measured. A smaller imprint will indicate greater internal pressure.
There are two types of applanation tonometry:
- tonometry according to Maklakov - a weight is used, the flat bottom of which is painted with a special substance;
- Goldman tonometry - fluorescein-stained plates are used, and pressure readings are read by a probe exposed to bright lighting.