ABPM - features of the procedure
ABPM is a technique that allows timely detection of blood pressure disorders in people at high risk. With the help of this examination, it is possible to take appropriate measures, adjust the therapeutic course, and prevent the development of extremely dangerous complications.
Patients suffering from cardiovascular pathologies are prone to changes in blood pressure. The reasons for a decrease or increase in blood pressure can be stressful situations, physical activity, and even the characteristics of the patient’s daily diet.
Hypertension is not diagnosed by a one-time blood pressure measurement. Information obtained in this way often turns out to be unreliable, due to various factors. The very stay of a person in the hospital is a stressful situation that contributes to an increase in blood pressure.
An examination such as 24-hour blood pressure monitoring (ABPM) makes it possible to make an accurate diagnosis.
Daily monitoring is considered an extremely informative and accurate method of diagnosis in people with diagnosed pathologies of the heart and blood vessels.
24-hour blood pressure monitoring (ABPM)
Your heart is under control
Modern medicine has everything necessary to detect pathology in the cardiovascular system at an early stage. One of these methods is heart monitoring, or more precisely, ABPM - 24-hour Blood Pressure Monitoring. The method developed by Norman Holter, during which specialists continuously monitor cardiac function for 24 hours, was named after its creator. At one time, Holter proved the value of his technique, which lies in the fact that the maximum effectiveness of monitoring cardiac activity occurs not at rest, as in the ECG procedure, but when the full cycle of human activity is covered during the day.
What does ABPM show?
The ABPM device makes it possible to record minimal changes in blood pressure, displaying them graphically. ABPM results are examined by a qualified specialist. Based on the information received, the doctor makes a diagnosis for the patient and develops a therapeutic course suitable for the specific clinical case.
This examination shows:
- changes in the patient’s blood pressure during physical activity;
- working pressure, in a calm state;
- pulse pressure indicators;
- the patient's blood pressure at night.
During monitoring, it is necessary for the patient to keep a diary in which he would note all changes caused by physical activity, possible psycho-emotional shocks, times of awakening and falling asleep, and dietary habits. Thus, the interpretation of ABPM results will be extremely reliable.
Carrying out this diagnostic is a lengthy process, since specialists have to work with a large amount of data. The device is characterized by high sensitivity. ABPM data combines the following:
- changes in blood pressure during physical activity;
- pulse pressure indicators;
- a graph of blood pressure changes throughout the day;
- level of blood pressure decrease at night;
- average diastolic and systolic pressure;
- level of decrease in blood pressure in a sleepy state.
Based on the analysis of the data obtained, a final medical opinion is made regarding the interpretation of ABPM.
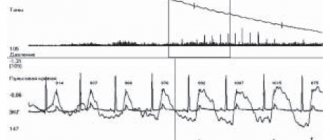
Example of survey results
Decoding the results
ABPM results are important for diagnosing many pressure abnormalities in patients, but they must be interpreted. They are deciphered by the doctor, allowing him to make an accurate diagnosis and select a course of therapy. After all, the results of monitoring, depending on the method and device, can be presented as a graph or a chain of blood pressure level records. Here are approximate comparative characteristics of the measurement results:
In this case, the patient is asked to keep a diary, entries in which allow an accurate interpretation of the ABPM results using the device. In the diary, the patient records all the loads and their time, the menu on the day of the study, and sleep time. If the patient experienced stress, he should record this fact in his notes, which will facilitate decoding. It is easy to decipher the readings, since there is a lot of information during this control.
- MRI of cerebral vessels - what it shows, indications and contraindications, how it is performed
Analysis of data obtained from a daily study of blood pressure with devices, the most informative are the following parameters: average blood pressure, time indices of hypertensive and hypotensive pressure, blood pressure range indicators. Moreover, the values are calculated both per day and for certain periods of time. The conclusion about hypertension is given after deciphering the monitoring.
Indications for examination
This procedure has the following clinical indications:
- hypotension;
- diagnosis of situational increases in blood pressure;
- identifying the degree of hypertension;
- monitoring blood pressure in women during pregnancy.
Holter monitoring can be recommended for people who have suffered strokes or heart attacks in the recent past, in order to monitor the dynamics and timely correction of the therapeutic course.
The following pathologies are relevant to the procedure:
- renal failure;
- vascular atherosclerosis;
- diabetes;
- heart failure;
- gestational disorders.
Patients suffering from these diseases are at high risk and are most susceptible to developing hypertension.
During pregnancy, examinations are carried out to monitor the health of the expectant mother. In the last trimesters, negative 24-hour blood pressure readings in the patient serve as an indication for an urgent cesarean section.
Long-term monitoring is mandatory for patients with hypertension to monitor the dynamics of the pathological process, monitor the effectiveness of the treatment, and develop the most effective therapeutic course.
A LITTLE SMAD is watching you
Blood pressure indicators that are measured during an appointment with a doctor or by the patient themselves do not always reflect the actual picture. The reasons are different. This includes the patient’s anxiety - “white coat hypertension”, and the load that may have occurred recently, and the adjustment of the tonometer. In principle, a one-time blood pressure measurement is not very informative. In order to obtain reliable and diagnostically significant information, a research method such as 24-hour blood pressure monitoring, or ABPM for short, is used. Typically, an ABPM device installed on a patient measures blood pressure every 30 minutes during the day and every 60 minutes at night. Daily statistics include at least 21 measurements. Least! With such data, we can say that the doctor receives almost 100% reliable information about the dynamics of blood pressure. Let us repeat once again that one-time measurements do not provide a clinical picture, since the obtained indicators depend on the current physical or psychological stress, the serviceability of the device, and the skill of the person who measures blood pressure.
Who, in accordance with federal standards, needs to carry out 24-hour blood pressure monitoring (ABPM)? For patients with arterial hypertension, ABPM is recommended in 100% of cases. 100%! There can be no exceptions. In total, there are more than twenty indications for ABPM. Blood pressure monitoring should be carried out in pregnant women, patients with insulin-requiring diabetes mellitus, and patients with a family history of arterial hypertension. This could be “white coat hypertension”, or monitoring the effectiveness of treatment.
Based on the ABPM results, the doctor receives six key indicators. Let's look at them.
The first indicator includes average pressure during the day and at night. It is important to note that the normal average daily pressure is 135 over 80, at night - 120 over 70. If the average daytime pressure is above 140 over 90, this is hypertension. If the nightly average is above 125 over 80, this is also hypertension. What lies between these limits, normal and hypertension, is considered borderline pressure.
Another indicator is the so-called daily index. Normally, night pressure should be 10-20% lower than during the day. It should decrease when a person falls asleep, smoothly transition to a plateau, and gradually rise in the morning. On the graph, the curve looks like a bucket. Dipper is a dipper in English and people with such graphs are called dippers accordingly. This is the norm. If the pressure decreases slightly, by less than 10%, then the “bucket” exists, but it is shallow. Such patients are called non-dippers
(
non-dippers
) and they have a high risk of developing heart failure and damage to target organs - the brain, heart, kidneys, liver, eyes. If a patient is prescribed treatment, but meanwhile remains a non-dipper, then we can say that the therapy is ineffective.
The next category of patients are overdippers
(
over-dippers
). These are those whose blood pressure drops by more than 20 percent at night—the dipper is deep. Such dynamics of blood pressure leads to hypoperfusion, insufficient blood supply to the brain. These are patients at high risk of strokes in the morning and night hours.
And the last fourth group is the night pickers
(
night-peakers
), that is, those who have very high night pressure, that is, there are night crises. This happens, for example, in patients with diabetes mellitus, malignant hypertension, resistant and symptomatic hypertension. Knight pickers have a high risk of stroke.
The third indicator is the rate of morning pressure rise. Normally, the rate of morning pressure rise should not exceed 10 mmHg per hour. If, for example, such a patient is undergoing antihypertensive therapy and it is higher, then this is a signal that the prescribed medication is ineffective. If the rate of morning pressure rise is above 15%, then the patient is at high risk of heart attack.
The fourth indicator of ABPM is the pressure load index, which shows the proportion of daily measurements exceeding the norm. If it makes up about 20% of all measurements taken during the day, then this is acceptable. If the pressure load index is above 25%, then we are talking about hypertension, above 30% is persistent hypertension, above 50% is refractory malignant hypertension.
The next indicator is pulse pressure, that is, the difference between systolic and diastolic pressure. Example: as a result of measuring blood pressure, the result was 120 over 80. Pulse pressure is 120 minus 80, for a total of 40. High pulse pressure is a risk factor for target organ damage. Normally, it should be less than 46. If ABPM reveals that it is higher, then we can conclude that therapy is ineffective, if any. There is a risk of complications developing.
The sixth indicator is blood pressure variability. During the day, pressure, like any other indicator, will change. It is important that it varies within a certain corridor. If the variability is high, that is, during the day the pressure went beyond the maximum permissible limits, then most likely the patient has vegetative-vascular dystonia, the prescribed therapy is ineffective and there is a high risk of target organ damage.
These are the main key points that you need to know when prescribing ABPM or if you keep your own blood pressure diary.
There are ABPM devices that only “can” measure blood pressure, and there are those that have the function of taking an electrocardiogram (ECG). We are talking about ABPM plus daily ECG monitoring. The latter makes it possible to identify the presence of coronary heart disease in the patient. As a result, very valuable diagnostic information can be obtained, since patients very often have a combination of hypertension and coronary artery disease. In the following materials we will talk about Holter ECG monitoring, the indicators that the doctor receives, and what they mean when diagnosing heart pathologies.
When is the procedure contraindicated?
24-hour blood pressure monitoring has no absolute clinical contraindications. The examination may be temporarily postponed for the following reasons:
- skin rashes;
- period of exacerbation of dermatological diseases occurring in a chronic form;
- fractures;
- burn lesions;
- bruises, traumatic injuries.
Various injuries and violations of the integrity of the skin in the area where the cuff is installed make the examination impossible. In such cases, diagnosis is postponed until the patient’s skin has fully recovered and restored.
In case of a fracture, ABPM is not possible
Preparation for the event
To obtain the most accurate and reliable ABPM results, it is necessary to properly prepare for the procedure. Patients should pay attention to the following recommendations:
- do not wear clothes that restrict or impede movement;
- normalize your schedule and daily routine;
- refrain from performing water procedures;
- avoid physical exertion and psycho-emotional shocks.
In the evening, before installing the device, you can take a sedative in order to have a good rest and recover before the examination.
If the patient is being treated with drugs, the effect of which may affect the examination results, it is necessary to report this.
When wearing the device, it is important to ensure that no moisture gets on it and the device does not fail.
How is the procedure performed?
The Holter examination includes an electrocardiogram and ABPM. This procedure is a round-the-clock monitoring of changes in heart rate and pulse, with fluctuations in blood pressure.
The examination is carried out as follows:
- An air-permeable cuff is placed on the patient’s arm (in the shoulder area);
- The cuff is fixed to the ABPM device;
- The device is attached using a harness to the patient’s chest;
- Blood pressure readings are measured automatically every half hour;
- The received data is recorded in the device’s memory.
The ABPM device is distinguished by a complex device that has the ability not only to measure blood pressure indicators, but to analyze them and draw up graphs. In order to get reliable results, the patient only needs to follow the following rules:
- refrain from taking medications without prior approval from your doctor;
- move freely and live according to your usual schedule;
- refrain from water procedures;
- Make sure that the tube of the device is not kinked.
It is also necessary to responsibly keep a diary, entering into it data about any physical activity or stressful situations that can provoke changes in blood pressure.
Holter study includes ABPM and electrocardiogram
ABPM and HOLTER
24-hour blood pressure monitoring (ABPM) and 24-hour Holter ECG monitoring.
ABPM-
The technique by which blood pressure is measured and the results recorded for 24 hours is called 24-hour monitoring.
It involves recording indicators at specified time intervals using a special apparatus. This method of monitoring cardiac activity makes it possible to determine the average pressure, its values at night and during the day, the amplitude of fluctuations and the threat of damage to target organs.
Measuring blood pressure around the clock is considered a diagnostic standard and prescribes treatment for hypertension. It has more potential for obtaining reliable results than a random one-time measurement.
The benefits of 24-hour blood pressure monitoring (ABPM) include:
- shows how the daily level of load affects the pressure value;
- reflects nighttime pressure changes;
- helps diagnose sharp fluctuations - hypertensive and hypotensive crises, orthostatic form of the disease, fainting conditions;
- when examining it, it is possible to make a forecast about the possibility of acute vascular disorders (stroke, heart attack);
- gives a chance to accurately select the optimal time and dosage of antihypertensive drugs or assess the effectiveness of taking prescribed medications;
- eliminates reaction to medical personnel.
The best option is simultaneous monitoring of blood pressure and ECG (Holter)
. This complex makes it possible to establish the relationship between the main characteristics of the cardiac cycle, which cannot be identified by standard one-time methods.
Indications for use
Used to diagnose the following conditions:
- clinical hypertension (reaction to health care workers);
- increased blood pressure during stress overload during working hours;
- borderline increase in pressure;
- nocturnal form of hypertension, angina, apnea;
- symptomatic variants of the disease - a reaction to medications that increase blood pressure, disorders of the autonomic nervous system, myocardial infarction or ischemia, circulatory failure, inadequate electrical stimulation or its poor tolerance;
- variability of indicators across multiple measurements;
- high blood pressure was detected in the absence of objective data from clinical studies;
- traditional measurement shows the norm for numerous risk factors and diseases of target organs;
- diagnosis of hypertension in pregnant women with possible preeclampsia.
The technique has no contraindications, but there are a number of pathologies when it needs to be temporarily abandoned:
- injuries or pathology of blood vessels of the hands,
- exacerbation of blood diseases,
- patient's refusal,
- pressure exceeding 195 mm Hg. Art.,
- serious forms of arrhythmia.
What should a patient do with ABPM in order to obtain reliable blood pressure readings?
:
The patient must adhere to the following rules during the monitoring period:
- the arm does not need to be bent during the measurement period, it should be in a relaxed state, located along the body; the lower level of the cuff is placed 1 - 2 cm above the elbow bend;
- if the device has started taking measurements, and at this time the patient is in motion (for example, walking down the street), then you need to stop and lower your hand;
- You can’t play sports or do intense physical work
- When carrying out diagnostics, it is prohibited to disconnect parts of the blood pressure measuring device, hit it or expose it to moisture.
The pneumatic cuff communicates with the pressure recorder through connecting tubes. It is a compact monitor that is attached to the subject's belt. Measurements are taken every 15 minutes during the day and every 30 minutes at night. The received data is loaded into a computer for processing by a special program.
Why keep a diary
In parallel with blood pressure measurements, the patient must record all events related to activity and health status: duration of sleep and its depth, number of night awakenings; level of psychological stress, stressful situations and your well-being during this period; physical activity; eating; all medications that are taken; presence of headache, dizziness, fainting, heart pain, visual impairment.
Then the doctor compares the data provided by the monitor with the patient’s complaints recorded in the self-monitoring diary. Based on them, we can draw conclusions about situations that contribute to increased blood pressure and draw up an optimal antihypertensive therapy regimen.
Patient Instructions
The installation process of the device is painless and does not cause any discomfort to the person. The only inconvenience that the patient faces is the pressure on the arm with the cuff that occurs during the period of measuring blood pressure.
There are certain instructions, following which the patient can prevent possible ABPM errors:
- wear comfortable, loose-fitting clothes;
- do not be nervous and try to avoid stress;
- eat as usual without changing your diet;
- avoid overwork;
- refrain from using medications intended to treat hypertension.
On the day of monitoring, in order to avoid unnecessary worries and unpleasant emotions that can distort the results, the patient is recommended to avoid unnecessary contacts and, if possible, spend time at home, in a calm, relaxed state.
Life schedule is also of great importance. Going to bed should be done at a person’s usual hours. Therefore, you should also refuse to work on night shifts during monitoring or schedule an examination for another day.
What does the doctor see from the ABPM results?
In addition to the direct increase in blood pressure in various situations, the cardiologist examines a person’s circadian rhythms - the natural decrease or increase in blood pressure during the day. Deviations from the normal rhythm may be a harbinger of hypertension or other health problems. Based on the information received, the doctor may recommend that you change your diet, give up bad habits, or undergo additional examinations. All this will help to avoid severe cardiovascular diseases in the future and maintain health and well-being for a long time!
Based on the data obtained during diagnosis, specialists from the Department of Cardiovascular Pathology of the European Clinic Siena-Med will determine a comprehensive treatment, which will include modern medication programs and a complex of computer hardware and physiotherapeutic methods.
We can help you. Remember that timely diagnosis is the key to high-quality and highly effective treatment
Disadvantages of the procedure
The ABPM device is compact and invisible to others, so it can even be worn under clothing.
The disadvantages of this procedure include the following:
- Impaired sensitivity of the hand in the area where the cuff fits. Some patients complain of tension, discomfort, and increased fatigue of the limb.
- Diaper rash, skin irritation. It is observed in people with overly sensitive and delicate skin. This is due to the fact that the material from which the cuff is made does not allow air to pass through and the skin cannot breathe.
- The need to ensure that there is no compression of the tube that connects the device to the cuff. It is especially difficult to follow this rule at night. Before going to bed, a person needs to choose a certain position that does not interfere with the free flow of air into the cuff area. As a result, some patients complain of insomnia and sleep disorders.
This procedure does not cause any other side effects or unwanted reactions. During the examination, a person can carry out everyday activities and lead a normal lifestyle.
Compact device causes minimal discomfort
Examination price
Daily blood pressure monitoring is prescribed to patients by a cardiologist. The price of the examination depends on factors such as the type of device used during the examination, as well as the prices of the specific clinic the patient goes to.
The average cost of ABPM is about 2300 - 2500 rubles. At the same time, in some clinics, the procedure can cost only 1200-1500 rubles, and in other, more expensive, private medical institutions - 3000 rubles.
Is it possible to deceive ABPM?
ABPM is a procedure that diagnoses hypertension, severe heart failure and other serious pathologies that are contraindications for military service.
For this reason, young people are often interested in the possibility of distorting the results of the examination in order to avoid conscription. It is indeed possible to deceive ABPM by using methods that artificially increase blood pressure:
- 3 days before installation of the device, use tonic medications.
- Drink strong coffee drinks, black tea, or take caffeine tablets.
- Hold your breath while the cuff is installed.
- When wearing the device, lower the arm to which the device is attached as often as possible below the level of your heart. Thus, blood flow processes are disrupted, which contributes to increased blood pressure.
- While measuring blood pressure, pull up your toes and squeeze your gluteal muscles.
- Avoid sleep on the day of monitoring. This is due to the fact that when you fall asleep, your blood pressure drops by 20%.
Experts note that the above actions have an extremely negative impact on the state of the cardiovascular system!
Daily blood pressure monitoring (ABPM) is an informative diagnostic method that allows you to monitor the condition of patients with diagnosed cardiovascular pathologies and prescribe them the most effective treatment, avoiding adverse consequences and complications.
ABPM indications
ABPM is prescribed in the following cases:
- if you suspect “white coat syndrome”;
- with a “borderline” increase in blood pressure (when its numbers are not high enough to immediately make a diagnosis, but cause caution in the doctor);
- with the first detected increase in blood pressure;
- if you suspect the symptomatic nature of hypertension (for example, when the increase in pressure is associated with stress before consulting a doctor or occurs due to a concomitant disease);
- when examining young people with unfavorable heredity for hypertension;
- if the patient periodically experiences fainting, to exclude hypotension (low blood pressure);
- in patients with already established hypertension, coronary heart disease and vascular lesions of the brain to identify critical blood pressure values;
- to evaluate and adjust drug therapy.