ARRHYTHMIAS: diagnosis and treatment
Arrhythmia (heart rhythm disturbance) is one of the most common pathologies (15-25%) in the practice of a cardiologist. Arrhythmia threatens not only the health, but, in some cases, the life of the patient. It is known that 10% of patients who survive acute myocardial infarction (MI) die within a year. The main risk factors for sudden death after MI are ventricular arrhythmias and heart failure (HF).
Cardiac arrhythmias are a change in the basic electrophysiological properties of the heart (automatism, excitability, conductivity), leading to a violation of the coordinated contraction of the entire heart or its parts and manifested by a change in the frequency and regularity of the heart rhythm.
It is very important for the doctor to establish the underlying cause of the disease that caused the arrhythmia. Sometimes this is associated with certain difficulties, since the causes of arrhythmia can be different: extracardiac, cardiac and idiopathic (primary electrical heart disease).
Extracardiac factors for the development of arrhythmia include functional and organic lesions of the central nervous system, dysfunction of the autonomic nervous system, endocrine diseases, electrolyte imbalance, mechanical and electrical trauma, hypo- and hyperthermia, excessive physical activity, intoxication with alcohol, nicotine, coffee, and drugs. This is especially true for sympathomimetics, cardiac glycosides, diuretics, many psychotropic and other drugs, including antiarrhythmics.
Cardiac factors are primarily coronary heart disease, heart defects, heart failure, arterial hypertension, inflammatory and non-inflammatory myocardial lesions, diagnostic manipulations and operations on the heart and coronary vessels.
Today there is a European standard for the diagnosis and treatment of arrhythmias. If arrhythmia is suspected, the doctor must establish the fact of rhythm disturbances, determine the nature of the arrhythmia, its cause, functional or pathological nature, and decide on the use of antiarrhythmic therapy. For these purposes, physical examinations, ECG, daily ECG monitoring (Holter), esophageal electrocardiography are used.
To clarify the diagnosis use:
- long-term recording of leads II, aVF, doubled ECG voltage and increased paper tape speed to 50 mm/s to identify P waves;
- additional ECG leads, ECG recording during carotid sinus massage for 5 s, bolus tests with medications and exercise tests.
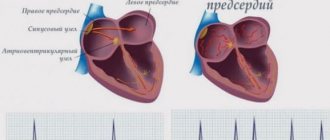
According to the clinical classification, arrhythmias are divided according to the functional principle: dysfunction of automaticity, excitability, conduction and combined arrhythmias. Automatic dysfunctions include sinus tachycardia, bradycardia, arrhythmia and migration of the rhythm source; dysfunction of excitability - extrasystole, paroxysmal and non-paroxysmal tachycardia, flutter and fibrillation (fibrillation) of the atria and ventricles. Conduction disorders include blockades: sinoauricular, atrial, atrioventricular, intraventricular; ventricular asystole. And the most complex are combined arrhythmias: sick sinus syndrome, escape contractions and rhythms, atrioventricular dissociation, premature ventricular excitation syndrome and parasystole.
All tachyarrhythmias are divided into two types.
- Tachycardia with a narrow QRS complex (antegrade conduction through the AV node); most often it is supraventricular paroxysmal tachycardia. It is treated carefully by administering verapamil, propranolol or digoxin intravenously.
- Wide QRS tachycardia (antegrade conduction through the accessory pathway) is often associated with atrial fibrillation and a very high (>250 beats/min) ventricular rate. If hemodynamic parameters are unstable, immediate cardioversion is indicated; Drug treatment is carried out with lidocaine or procainamide intravenously.
Arrhythmias with a narrow QRS complex
- Atrial extrasystole is an altered wave with normal QRS width. If symptomatic, β-blockers or group IA drugs are prescribed.
- Sinus tachycardia - heart rate 100–160 with a normal P wave. First of all, the causes of arrhythmia are eliminated, if the arrhythmia is symptomatic - β-blockers.
- Paroxysmal supraventricular tachycardia - at a heart rate of 140–250, the P wave is pointed or inverted in leads II, III, aVF. Adenosine, verapamil, β-blocker, group IA drug, and electrical pulse therapy (150 J) are prescribed. Paroxysmal atrial tachycardia with block - at a heart rate of 130–250, a straight pointed P 2:1, 3:1, 4:1 block. If digitoxin was administered, it should be interrupted and K+ corrected; diphenine 250 mg IV over 5 minutes.
- Atrial flutter - heart rate 250–350, saw-tooth flutter waves, 2:1, 4:1 T blockade. Digoxin, β-blockers or verapamil are administered to reduce the ventricular rate.
- Atrial fibrillation - heart rate>350, P is indistinguishable, QRS intervals are irregular. EIT may be required to restore sinus rhythm (after prolonged anticoagulation) with procainamide or quinidine (flutter: 50 J; fibrillation: 100-200 J).
- Multifocal atrial tachycardia - with a heart rate of 100–220 - more than three differentiated forms of the P wave with different P-P intervals. If there is pathology of the lungs, treatment of the underlying disease is required, verapamil is prescribed to reduce the frequency of ventricular contractions.
Arrhythmias with wide QRS complex
- Ventricular extrasystoles - with complete compensatory pauses between normal complexes. The use of certain drugs, as for ventricular tachycardia.
- Ventricular tachycardia is a moderately severe irregularity with a heart rate of 100–250. In case of unstable hemodynamics, cardioversion (100 J) or intravenous administration of procainamide, lidocaine, or bretylium is indicated. For long-term prevention, it is advisable to prescribe drugs of groups IA, IB, 1C, III.
- Ventricular tachycardia of the “pirouette” type is sinusoidal oscillations with a height in the QRS. The administration of lidocaine is indicated, in the absence of a history of coronary heart disease - isoproterenol, bretylium, magnesium. Quinidine and all drugs that prolong the QT interval are contraindicated.
- Ventricular fibrillation - unstable electrical activity on the ECG. Immediate defibrillation is needed (200-400 J).
- Supraventricular tachycardia with aberrant ventricular conduction - a wide QRS complex with a P wave typical of a supraventricular rhythm.
Treatment is prescribed as for the corresponding supraventricular rhythm, but if the ventricular rate exceeds 200 - as for WPW syndrome.
Atrioventricular block
I degree. An extended constant PR interval (0.20 s) does not require treatment and can be considered as normal or be caused by vagotonia, which often occurs after the use of digitalis.
II degree. Mobitz I (Wenckebach). The ECG shows a narrow QRS complex with a progressive increase in the PR interval until the QRS complex drops out, after which the sequence is repeated. It is observed with digitalis intoxication, vagotonia, and lower myocardial infarction. Usually does not require treatment; if the arrhythmia is symptomatic, atropine 0.6 mg is injected into a vein (the injection is repeated three to four times). In some situations, a temporary pacemaker is used.
Mobitz II. The PR interval is fixed, the complexes periodically fall out in a ratio of 2:1, 3:1 or 4:1, the QRS complex is wide. Usually occurs with damage to the conduction system or myocardial infarction. This rhythm is life-threatening and often leads to complete AV block. To eliminate the pathology, a pacemaker is prescribed.
III degree (complete AV block). The atria and ventricles contract independently of each other. It is observed in cases of damage to the conduction system of the heart, myocardial infarction, and digitalis intoxication. If there is no transient combination of complete AV block with asymptomatic congenital heart block or inferior myocardial infarction, a permanent pacemaker is indicated.
Pre-excitation syndrome (WPW)
The impulse is carried out through an additional pathway between the atria and ventricles. The ECG is characterized by a short PR interval and merged, upward-directed QRS complexes (delta wave).
At the treatment stage, it is important to select the most effective drug in terms of matching the spectrum of action and the nature of the arrhythmia and at the same time the safest drug. Let's look at some of these medications most commonly used by the medical practitioner.
All modern antiarrhythmic drugs are divided into three groups.
Group 1. Drugs that reduce the flow of sodium ions into cardiac muscle cells.
These substances - membrane stabilizers - block sodium channels and prevent the spread of pathological impulses. However, it should be remembered that increasing the dose of the drug often provokes arrhythmia, suppressing impulse conduction in normal tissues, especially with tachycardia, hyperkalemia and acidosis.
Group 1 A with moderate conduction delay.
- Quinidine sulfate - loading dose (LOD) - 500-1000 mg IV, maintenance dose (SD) - 200-400 mg orally after 6 hours; side effects (AE) - arterial hypotension, tinnitus, diarrhea, QT prolongation, anemia, thrombocytopenia.
- Quinidine gluconate - UD-500 - 1000 mg IV, PD - orally 324-628 mg after 8 hours, PE - the same.
- Procainamide - 500-1000 mg IV, IV: 2-5 mg/min orally 500-1000 mg after 4 hours; PE - nausea, lupus-like syndrome, agranulocytosis, QT prolongation.
- Long-acting procainamide - PD - orally 500-1250 mg every 6 hours, PE - AV blockade, myocardial depression, QT prolongation.
- Disopyramide - PD - orally 100-300 mg every 6-8 hours, PE - anticholinergic effects.
Group 1 B with minimal conduction delay.
- Lidocaine - UD-1 mg/kg bolus IV, then 0.5 mg/kg bolus every 8-10 minutes to a total dose of 3 mg/k; PD - 1–4 mg/min; PE - confusion, seizures, respiratory depression.
- Tocainide - orally 400-600 mg every 8 hours; PE - nausea, tremor, lupus-like reaction, confusion.
- Mexiletine - orally 100–300 mg every 6–8 hours; PE - muscle tremors, nausea, impaired gait.
Group 1 C with pronounced slowing of conduction.
- Flecainide - orally 50-200 mg every 12 hours; PE - nausea, increased ventricular arrhythmia, prolongation of PR and QRS intervals.
- Propafenone - 150-300 mg orally every 8 hours.
Group 2. β-blockers.
As a result of eliminating the excessive effect of catecholamines on the heart, these drugs reduce excitability, heart rate, and normalize rhythm. This class includes metoprolol, nadolol, pindolol, trazicor, cordanum. A typical representative of β-blockers is propranolol.
Propranolol - UD - 0.5-1 mg/min IV to 0.15-0.2 mg/kg; PD - orally 10-200 mg every 6 hours; PE - bradycardia, AV block, CHF, bronchospasm.
Group 3. Drugs that block potassium channels and prolong the action potential.
- Amiodarone - UD - orally: 800-1400 mg daily for one to two weeks; PD - orally 200-600 mg daily, every four to five days of taking the drug you should take a break of one or two days; PE - thyroid dysfunction, pulmonary fibrosis, hepatitis, lipofuscin deposition in the cornea, bluish skin, QT prolongation.
- Bretilium - UD-5-10 mg/kg IV; PD - 0.5-2.0 mg/min i.v.; PE - nausea, arterial hypertension, orthostatic hypotension.
- Sotalol - orally 80-160 mg every 12 hours; PE - fatigue, bradycardia, increased ventricular arrhythmia.
Group 4. Medicines that block slow calcium channels.
They slow down the conduction of electrical impulses, preventing the transport of calcium ions into the cell. The most pronounced antiarrhythmic properties are found in two representatives of this class - verapamil and diltiazem.
Verapamil - UD - 2.5-10 mg IV; PD - orally 80-120 mg three to four times a day; PE - AV block, arterial hypotension, CHF, constipation.
For arrhythmias, drugs of other classes are also used: potassium drugs, digoxin, adenosine.
Digoxin - UD - orally i.v. 0.75-1.5 mg for 24 hours; PD - orally, intravenously 0.125-0.25 mg daily; PE - nausea, AV block, supraventricular and ventricular arrhythmia.
Adenosine - iv 6 mg bolus, if no effect, 12 mg; PE - transient arterial hypotension or atrial asystole.
It should be remembered that all antiarrhythmic drugs, without exception, can have toxic effects. This applies to a greater extent to drugs in group 1 A, which cause prolongation of the QT interval in combination with torsades de pointes (TdP), torsade de pointes/fibrillation, and ventricular tachycardia. In this case, discontinuation of the drug is necessary if the QT interval adjusted to heart rate is prolonged by more than 25% (QT must be divided by the square root of the RR interval).
So, when prescribing antiarrhythmic drugs, monitoring drug levels and ECG intervals (especially QRS and QT) is mandatory. If the patient has a history of liver or kidney failure, doses should be reduced. Antiarrhythmic drugs should not be prescribed to patients after acute myocardial infarction with asymptomatic ventricular arrhythmias, as this increases the risk of death.
L. N. Romanova, Candidate of Medical Sciences, Associate Professor of NSMA named after. S. M. Kirova, Nizhny Novgorod
Diagnosis of arrhythmia
Doctors have several methods for detecting arrhythmias, and each has its own characteristics.
- ECG
is a publicly available method that provides information about the patient’s rhythm at a given moment in time, allows you to record permanent disturbances and transient ones, if they are present at the time of registration. - Holter monitoring
ECG - 24-hour recording of an electrocardiogram. With this method, it is possible to establish all disturbances in the functioning of the heart within a day. - EchoCG
is an ultrasound examination of the heart. Makes it possible to visually determine the presence of arrhythmia and identify the organic cause of its occurrence. - Provocative tests
: orthostatic test, transesophageal electrophysiological study, intracardiac ECG recording) are capable of artificially inducing and recording arrhythmia when it cannot be detected during daily monitoring due to its transient nature.