Synonyms: immunoglobulins class G, IgG.
Immunoglobulins (IG) are protein compounds in blood plasma - glycoproteins, the main function of which is to protect the body from infections. IGs are specific antibodies produced by cells of the immune system in response to the invasion of pathogenic microorganisms - pathogens of viral, bacterial, fungal and other diseases.
Immunoglobulins class G (IgG) are dominant among all other serum immunoglobulins. They provide long-lasting and persistent, in some cases lifelong, immunity against a number of serious pathologies, for example, measles, rubella, and chickenpox.
The IgG test is used in the diagnosis of chronic, often recurrent diseases, viral liver pathologies, diffuse connective tissue damage, autoimmune disorders, HIV infection, oncology, etc.
Function of immunoglobulin IgG
Immunoglobulins G deactivate viral and bacterial toxins and trigger complement-fixing reactions and phagocytosis. Due to their small molecular weight, they quickly and easily enter the extracellular space, where they perform a protective function. Immunoglobulins G are able to penetrate the placental barrier and enter the blood of the fetus from the mother's blood.
Antibodies are part of the humoral immune response; they act very specifically, since they are always directed against a specific antigen. Their purpose is to participate in immune reactions. Immunoglobulins form immune complexes with antigen molecules, activate the complement system and cause inflammatory reactions. This aims to neutralize the irritant and safely remove it from the body.
Each class of antibodies has different structural properties, so they perform specialized functions. In particular, immunoglobulin G is capable of:
- neutralize microorganisms;
- prevent relapses of diseases, for example, mumps, chickenpox, measles, rubella;
- protect the fetus.
What are antibodies? And how to decipher the results of the analysis?
Antibodies are proteins that the immune system produces in response to infection. In laboratory diagnostics, it is antibodies that serve as markers of infection. The general rule for preparing for an antibody test is to donate blood from a vein on an empty stomach (at least four hours must pass after eating). In a modern laboratory, blood serum is examined on an automatic analyzer using appropriate reagents. Sometimes a serological test for antibodies is the only way to diagnose infectious diseases.
Tests for infections can be qualitative (they answer whether there is an infection in the blood) or quantitative (they show the level of antibodies in the blood). The level of antibodies for each infection is different (for some there should be none at all). Reference values (normal values) of antibodies can be obtained with the test result. In the online laboratory Lab4U you can take a set of tests for all TORCH infections at one time and with a 50% discount!
IgG during pregnancy
Immunoglobulins are a natural component of blood plasma. They can cross the placental barrier. There are receptors for IgG on the surface of the trophoblast; they combine and transfer immunoglobulins from the mother’s blood directly into the fetal blood. Thus, this mechanism becomes a passive defense of the child against infections. The fetus's immune system has not yet formed, so maternal antibodies come to the fore. When the mother's antibodies are lacking, doctors prescribe intravenous immunoglobulin G.
General information
IgG makes up up to 80% of all immunoglobulins contained in serum, and up to 20% of its total proteins. They produce IgG plasma cells (mature B lymphocytes).
Class G immunoglobulins provide the body's secondary humoral response to infection. That is, first, class M immunoglobulins (“alarm antibodies”) are produced in response to foreign cells in the body, and only after 5 days do G antibodies (IgG) appear. Their half-life is 23-25 days. This means that throughout this time the body is actively “fighting” the disease, as a result of which its resistance to the disease increases.
Indications for IgG testing
Indications for immunoglobulin G testing:
- assessment of local immunity and speed of reaction to antigens;
- diagnosis of immunodeficiency conditions and determination of their severity;
- elucidation of the causes of frequent inflammatory, infectious and chronic pathologies;
- assessment of the functioning of the immune system in the diagnosis of autoimmune diseases;
- determination of blood composition in hematological diseases;
- screening for oncological processes;
- assessment of the effectiveness of treatment with immunoglobulin replacement drugs;
- monitoring the course of myeloma during treatment.
Treatment methods for secondary ID
Immunotropic therapy is mainly used, which can be of different directions:
- active immunization;
- replacement therapy;
- taking immunotropics.
The choice of immunotropic therapy depends on how acute the inflammatory-infectious process is and what immunological defect is identified. When the symptoms of the disease subside, vaccine therapy can be used for prevention.
Immunoglobulins administered intravenously are used as replacement therapy. Their main active ingredient is special antibodies obtained from donors. Immunoglobulins containing only IgG are often prescribed.
Immunotropic treatment of secondary ID
Using immunomodulators, the effectiveness of antimicrobial therapy can be increased. Immunomodulators should be part of complex therapy together with etiotropic treatment of infection. The doctor calculates the regimen and dosage individually.
Immunological monitoring should be carried out while taking immunomodulators. If the infection is in an acute stage, immunomodulators are used with caution. Otherwise, you can cause a severe general inflammatory response and septic shock as a result. Source: G.A. Samsygina, G.S. Koval Problems of diagnosis and treatment of frequently ill children at the present stage // Pediatrics, 2010, v. 89, no. 2, pp. 137-145
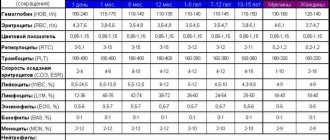
Normal value for immunoglobulin G
The norm of immunoglobulin G for newborns is 3.97–17.65 g/l. This indicator is due to the fact that the body of a child who has just been born still uses antibodies received from the mother.
In the first year of a child’s life, he begins to produce his own antibodies. At this age, the normal immunoglobulin level for boys is 3.97–17.65 g/l, and for girls – 3.91–17.37 g/l. Norm up to two years: for boys – 4.75–12.1 g/l, for girls – 4.88–12.26 g/l.
Then the amount of immunoglobulins in the blood reaches the same level as in adults. For boys and men, the norm is 5.4-18-22 g/l, for girls and women - 5.52-16.31 g/l.
Prevention methods
ID is easier to prevent than to treat. It is important to remember that the condition of the child directly depends on how correctly the pregnancy was planned. If one of the parents has problems with immunity, he must undergo special procedures to exclude a similar pathology in the child.
In the first six months of life, only breastfeeding is recommended, because breast milk contains all the necessary elements that contribute to the development of full immunity. If there is no lactation, you need high-quality artificial mixtures, but always supplemented with multivitamins.
Sources:
- Doan Thi Mai. Recurrent infections in children - the risk of immunodeficiency // Pediatrician, 2021, v. 8, special issue, pp. 109-110.
- M.V. Kudin, S.A. Sergeeva, A.V. Skripkin, Yu.N. Fedorov. Prevention of morbidity in children with secondary immunodeficiency in disadvantaged ecological regions // Bulletin of VolSMU, 2009, No. 1(29), pp. 87-95.
- G.A. Samsygina, G.S. Koval. Problems of diagnosis and treatment of frequently ill children at the present stage // Pediatrics, 2010, v. 89, no. 2, pp. 137-145.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
What can affect immunoglobulin G?
It is important to know that during intense muscle loads, as well as psychological stress, the level of immunoglobulin G can physiologically increase. In addition, immunization in the last 6 months or taking medications may increase the level.
Agents that increase the concentration of immunoglobulin G:
- valproic acid;
- carbamazepine;
- phenytoin;
- chlorpromazine;
- penicillamine;
- dextran;
- oral contraceptives;
- methylprednisolone;
- gold preparations;
- estrogens.
The level of immunoglobulin G can be reduced by:
- burns received;
- radiation exposure;
- taking cytostatics and immunosuppressants;
- intestinal pathologies that are accompanied by protein loss, for example, ulcerative colitis, Crohn's disease;
- renal failure, nephrotic syndrome.
IgG is elevated
An increase in the level of immunoglobulin G indicates that an acute or chronic infectious process is beginning in the human body. Immunoglobulins may increase in the following cases:
- whooping cough;
- diphtheria;
- scarlet fever;
- measles;
- rubella;
- chicken pox;
- tuberculosis;
- mononucleosis;
- hepatitis;
- cirrhosis of the liver;
- lupus erythematosus;
- rheumatic fever;
- rheumatoid arthritis;
- helminthic infestations;
- acute and chronic pathologies of the pulmonary, urogenital and intestinal systems;
- recovery period after an infection;
- sarcoidosis;
- cystic fibrosis;
- Waldenström's disease;
- chronic lymphocytic leukemia;
- multiple sclerosis;
- syphilitic damage to the brain or spinal cord;
- severe allergies;
- AIDS, HIV;
- development of oncology.
Various classes of antibodies IgG, IgM, IgA
Enzyme immunoassay determines infectious antibodies belonging to various Ig classes (G, A, M). Antibodies to the virus, in the presence of infection, are detected at a very early stage, which ensures effective diagnosis and control of the disease. The most common methods for diagnosing infections are tests for IgM class antibodies (acute phase of infection) and IgG class antibodies (sustained immunity to infection). These antibodies are detected for most infections.
However, one of the most common tests - hospital screening (tests for HIV, syphilis and hepatitis B and C) does not differentiate the type of antibodies, since the presence of antibodies to the viruses of these infections automatically assumes a chronic course of the disease and is a contraindication, for example, for serious surgical interventions. Therefore, it is important to refute or confirm the diagnosis.
A detailed diagnosis of the type and amount of antibodies for a diagnosed disease can be done by taking an analysis for each specific infection and type of antibodies. Primary infection is detected when a diagnostically significant level of IgM antibodies is detected in a blood sample or a significant increase in the number of IgA or IgG antibodies in paired sera taken at an interval of 1-4 weeks.
Reinfection, or repeated infection, is detected by a rapid rise in the level of IgA or IgG antibodies. IgA antibodies have higher concentrations in older patients and are more accurate in diagnosing ongoing infection in adults.
A past infection in the blood is defined as elevated IgG antibodies without an increase in their concentration in paired samples taken at an interval of 2 weeks. In this case, there are no antibodies of classes IgM and A.
Reduced IgG
Since immunoglobulins G are able to penetrate the placental barrier, their level often drops in a pregnant woman, resulting in infectious processes.
Also, IgG levels may decrease in the following cases:
- tumors of the lymphatic system;
- variable immunodeficiency;
- agammaglobulinemia;
- transcobalamin deficiency;
- chronic viral infection;
- Louis-Bar syndrome;
- Wiskott-Aldrich syndrome;
- inflammatory pathologies of the large intestine;
- nephrotic syndrome;
- congenital muscular dystrophy;
- poisoning from coal or oil processing waste;
- long-term treatment with immunosuppressants;
- dermatitis, burns and other diseases that are associated with the body’s loss of protein;
- irradiation;
- splenectomy.
Low immunoglobulin in newborns in the first year of life is physiological and is considered normal.
Diagnostics of ID
A family history and complaints of the child (if he is not a newborn), an examination, as well as a number of laboratory tests are collected: molecular genetics, clinical blood test, etc.
Important! If the family already has a child with primary immune deficiency, then prenatal diagnosis is extremely important when carrying a second one.
Signs and symptoms of primary immunodeficiency are detected in children already in the first weeks of life. When a doctor collects anamnesis, he pays special attention to the frequent incidence of viruses and bacterial infections, to heredity aggravated by disorders of the immune system, to congenital malformations.
Often such pathology is detected much later and by chance, when other tests are performed.
The main methods for diagnosing both congenital and acquired disorders of the immune system:
- examination of the child, during which special attention is paid to the condition of the skin, as there may be fungal infections, erosions, dystrophy, ulcers, swelling of different parts of the body;
- blood tests - pathology is indicated by a violation of the leukocyte formula;
- special immunological studies;
- molecular genetic analysis.