What it is
The thymol test is considered a highly specialized blood test. Its second name is Maclagan's test. With its help, the condition of the liver is assessed, or rather its ability to produce blood plasma protein. In addition, the doctor, based on the sample, evaluates the ratio of protein fractions , which makes it possible to identify some diseases and even predict them before noticeable symptoms appear.
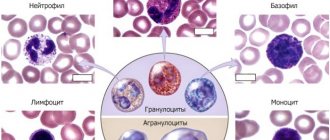
The blood proteins themselves are divided into two general groups, which also have their own subsections:
- globulins;
- albumins.
With the help of the above proteins, the acid-base balance of the blood plasma is regulated, the rate of coagulation is changed, the required volume is maintained, as well as the transport of drug components and other compounds.
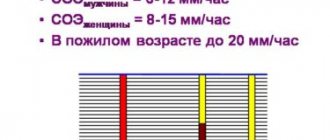
The sample is studied based on the rate of protein sedimentation. For this reason, it is classified as coagulation biochemical studies. A test is carried out by adding a special solution to the resulting serum. As a result, a chemical reaction is observed.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
If the course is positive, cloudiness of the serum is observed. Depending on the severity of the turbidity of the resulting solution, the result of the sample is determined. It is indicated in Maclagan units, that is, in units of M.
The thymol test is considered an outdated type of test, but is still used in some laboratories. It is prescribed mainly when it is necessary to identify:
- hepatitis type A;
- drug intoxication;
- lupus erythematosus;
- other diseases.
How is a biochemical study carried out?
The essence of the analysis is to monitor the blood serum sediment. Units of magnitude are expressed in M or according to Shank-Hoaland in SH. The research method is called photocolorimetric (the wavelength of the radiation is usually 0.65 microns) or turbidimetric.
Blood serum is taken and a solution of thymol and medinal-veronal is added. After 30 minutes, a laboratory assistant examines the result using a photocolorimeter. Due to the reaction of proteins to the influence of thymol, a change in the transparency of the test liquid occurs. The color and type of sediment are taken into account, and not its chemical properties.
Normal for women
Normal test results depend on the correctness of the tests. This must be done on an empty stomach in the morning, but you are allowed to drink water before the test. When using a study against the background of drug therapy , before the test you should notify the doctor about the use of drugs so that he can make an adjustment for distortion of the results.
In women, the normal thymol test is up to 5 units M. However, with dysproteinemia and taking oral contraceptives, the norm increases. If the indicator is elevated outside of these conditions, then there is a high probability of liver failure. The test itself allows you to identify the stability of proteins, and depending on the indicators, health problems are identified.
An increase in the indicator may not be diagnosed with obstructive jaundice ; only when the disease moves to a more serious stage and with the development of inflammation can a problem be diagnosed.
In addition to jaundice, the absence of a positive result of the thymol test can be observed when the natural ratio of alpha and beta globulins differs, or in the presence of significant amounts of excess or insufficient weight.
It is worth noting that when a person develops hepatitis B, the thymol test does not give a positive result, since its result will vary from 1 to 5 M units , this is not a deviation from normal values.
Blood chemistry
Procedure, preparation
This is unlikely to be a revelation for anyone, but just in case, let us remind you: a small amount of venous blood taken into a syringe by venipuncture is subjected to
biochemical analysis The ulnar vein, which runs shallow under the skin in the cubital fossa, is punctured (pierced with a thin hollow needle); For a single analysis, the left hand is often used. A rubber tourniquet is first applied over the elbow joint, and you are asked to clench and unclench your fist several times so that the vein becomes prominent (after puncturing, the tourniquet is immediately removed). In some cases, the veins turn out to be “bad”, they escape or “go away” from the needle, but for an experienced nurse in the vast majority of cases this is not a problem; and if there is a problem, then the blood will be collected in the same way from the back of the hand. Talking seriously about the “painfulness” of venipuncture or persuading adults not to be afraid, for example, comparing the procedure to “a mosquito that is about to bite you unnoticeably,” is really somehow awkward. From our point of view, a mosquito bite, if not more painful, is certainly a hundred times more offensive, not to mention the acoustic accompaniment and the pointlessness of such blood loss. However, in the manipulation room there is always a cotton swab with ammonia on hand, and the nurse’s eyes remain wary and attentive, even if she smiles: patients are different, including hypersensitive (to the point of fainting) to the sight of their own blood. Let us emphasize that it is to the appearance and the very fact of venipuncture, and not to the pain. It is a completely different matter if such an analysis is prescribed for a child - unfortunately, in some cases it is absolutely necessary. Here, again, a lot depends on the experience, technicality and psychological skill of the manipulative “sister”, as well as, sometimes to a decisive extent, on the emotional state of the parents: it can be both analgesic and sensitizing (in some cases, ammonia is more likely to be needed by an adult than by a child who curiously watches the actions of the nurse and the shaking pale green mother).
that new methods of biochemical analysis will be introduced into widespread clinical and laboratory practice : the study of saliva (instead of blood), microemulsion analysis based on a microchip, SIMBAS technology, etc., which will make this laboratory test much faster , accurate, inexpensive and completely painless.
The issue of proper preparation is very important and serious. It should be remembered that no one is as interested in the information content and reliability of the analysis as the patient himself. Blood is a very complex and mobile tissue in every sense, including in terms of biochemical composition. The doctor who ordered a laboratory blood test (this applies to any test, not just biochemical), must be informed about all regularly taken medications, herbal remedies and nutritional supplements, as well as about chronic and previous diseases. Almost always, blood for biochemical testing is donated in the morning, on an empty stomach. You can only drink clean, non-carbonated water, and you should not smoke for an hour before sampling. Actually, smoking is not allowed at all - it is strictly contraindicated! – so due to the analysis I will have to quit.
Please note that, firstly, the rules for preparing for biochemical analysis may change in individual cases (the referring doctor will tell you this in detail) and, secondly, a strict fast before the analysis includes refusing not only food, but also chewing rubber bands. In addition, the above-mentioned emotions also affect the composition of the blood, in particular, the balance of hormones, so the most accurate result is achieved when the patient is in a calm, balanced state (for example, it is not advisable to rush to the laboratory in a McLaren through morning traffic jams, but it is better to leave early and leisurely take a walk - thinking about how beautiful our city is, how we decorate it with our presence and what nice people are waiting for us at the Lakhta Clinic).
Promoted
If the test result is positive, liver damage is diagnosed. Today, a positive test result is also observed in diseases of the kidneys, digestive system, and the appearance of malignant neoplasms. Due to the inaccuracy of diagnosing the disease, it is necessary to carry out additional research to identify the exact reason for the deviation of the thymol test from the norm.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
Increased test results can be observed without pathologies. Most often, increased results appear in people who often eat fatty foods. There is an increase in cholesterol in their blood.
The gradual accumulation of lipoproteins will contribute to their deposition in blood vessels and the formation of atherosclerotic plaques.
Their formation contributes to the development of atherosclerosis. Thus, if the result of the thymol test is elevated, but there are no clinical manifestations of the disease, then it is necessary to urgently change the diet .
Advantages of thymol test
Typically, a thymol test is used in addition to bilirubin and enzymes (transaminases - AlT, AST, alkaline phosphatase) if damage to an organ is suspected, characterized by the variety of biochemical reactions occurring in it. Of course, we are talking about the liver, on the normal functioning of which the implementation of basic life processes in all cells of a living organism largely depends. And what’s interesting is that these indicators may not yet particularly respond to pathological changes and therefore may not exceed or slightly exceed the levels of normal values, and the thymol test will already clearly “creep” upward.
In addition to identifying liver abnormalities, the thymol test, the norm of which is from 0 to 4 SH units, in other cases helps in diagnosing pathological conditions of the heart, gastrointestinal tract, kidneys and other organs.
The main advantages of the thymol test are that it:
- Does not require special time and material costs, or the use of complex equipment (reagents are prepared on a magnetic stirrer in a fume hood);
- It is easy to perform (the result is read using an electrospectrophotometer, which is available in any laboratory);
- Makes it possible to start treatment in the early stages of the disease and thus helps to avoid unwanted complications caused by a prolonged inflammatory process;
- Can be used as a good indicator of the effectiveness of therapeutic measures aimed at restoring the functional abilities of the liver tissue.
That is why, despite the wide variety of new laboratory tests, in some cases the thymol turbidity test remains among the main tests that identify pathological conditions of the liver.
Causes
An increase in sample values may be caused by the following reasons:
- kidney diseases;
- large area burns;
- strict diets;
- genetics;
- frequent consumption of fatty foods;
- systemic diseases;
- endocarditis;
- diseases of the gastrointestinal tract;
- rheumatoid diseases;
- myeloma;
- pancreatitis;
- energite;
- hepatitis;
- various types of neoplasms in liver tissue;
- damage to the liver parenchyma by alcohol substitutes or alcohol;
- poisoning by poisons, metals, drugs;
- cirrhosis;
- fatty damage to liver tissue;
- long-term use of hormonal drugs;
- liver diseases of various etymologies.
It is the last point that most often leads to an increase in sample rates. However, to calculate an accurate diagnosis, it is recommended to visit a doctor and get prescriptions for treatment.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
A special feature of the thymol test is its ability to detect type A hepatitis in the early stages, however, the test is not informative if a person has already had hepatitis before and was successfully cured. Therefore, to clarify the diagnosis, it is recommended to undergo additional tests.
In order for the results of the study to be as reliable as possible, it is necessary
to prepare in advance for the test .
A week before the test, it is recommended to follow a diet with limited fat and sugar intake. The day before the study, you must give up coffee, tea, and alcohol. The sample itself is taken in the morning on an empty stomach; for this reason, eating is not recommended 12 hours before the test. In the morning you can only drink water in limited quantities, and you cannot eat anything.
Biochemistry 13 indicators (venous blood) in Moscow
Albumen:
Elevated levels of albumin in the blood can occur with dehydration.
Reasons for low albumin levels: impaired albumin synthesis (with liver diseases or hereditary pathologies), increased protein consumption (with burns, diabetes, blood loss, kidney disease), increased metabolic rate (with thyrotoxicosis, infectious and rheumatic diseases, tumors), fluid retention in the vascular bed (when taking estrogen-containing drugs, heart pathologies), deficiency in albumin intake from food (during fasting or diseases of the digestive tract).
Creatinine:
Increased levels with: active physical activity, consumption of meat foods, acromegaly, hypothyroidism, gigantism, infectious processes and diabetes.
Decreased levels in: hyperthyroidism, consumption of vegetarian foods, anemia, leukemia, paralysis and muscular dystrophies, diseases with a decrease in muscle mass, advanced stage of kidney pathology, inflammatory and metabolic diseases.
Potassium, Sodium, Chlorides:
Increased potassium (hyperkalemia): cell damage (hemolysis - destruction of blood cells, severe starvation, convulsions, severe injury), dehydration, acute renal failure (impaired excretion by the kidneys), adrenal insufficiency. Reduced potassium (hypokalemia): chronic fasting (failure to receive food), prolonged vomiting, diarrhea (loss with intestinal juice), impaired renal function, excess adrenal hormones (including taking dosage forms of cortisone), cystic fibrosis.
Increased sodium (hypernatremia): excessive salt intake, loss of extracellular fluid (profuse sweat, severe vomiting and diarrhea, increased urination (diabetes insipidus), excessive retention (increased function of the adrenal cortex), impaired central regulation of water-salt metabolism (hypothalamic pathology, coma ).
Reduced sodium (hyponatremia): loss (abuse of diuretics, kidney pathology, adrenal insufficiency), decreased concentration due to increased fluid volume (diabetes mellitus, chronic heart failure, liver cirrhosis, nephrotic syndrome, edema).
Increased chlorides: dehydration, acute renal failure, diabetes insipidus, salicylate poisoning, increased adrenal function.
Decreased chlorides: excessive sweating, vomiting, gastric lavage, increased fluid volume.
Total cholesterol:
Increased: genetic characteristics (familial hyperlipoproteinemia), liver disease, hypothyroidism (thyroid deficiency), alcoholism, coronary heart disease (atherosclerosis), pregnancy, taking synthetic sex hormones (contraceptives).
Decreased: hyperthyroidism (excess thyroid function), impaired fat absorption.
Glucose:
Increased (hyperglycemia): diabetes mellitus (insulin deficiency), physical or emotional stress (adrenaline release), thyrotoxicosis (increased thyroid function), acromegaly, gigantism (increased levels of growth hormone), Cushing's syndrome (increased levels of the adrenal hormone - cortisol ), diseases of the pancreas (pancreatitis, tumor, cystic fibrosis), chronic diseases of the liver, kidneys.
Decreased (hypoglycemia): fasting, insulin overdose, pancreatic disease (tumor from cells that synthesize insulin), insufficiency of the endocrine glands (adrenal glands, thyroid, severe poisoning with liver damage (alcohol, arsenic, chlorine, phosphorus compounds, salicylates, antihistamines), condition after gastrectomy, diseases of the stomach and intestines (malabsorption).
Alkaline phosphatase:
Increase: during pregnancy, liver diseases, diseases of the skeletal system, infectious mononucleosis, primary cirrhosis of the liver.
Reduction: with hypothyroidism, lack of magnesium and zinc, severe anemia.
Urea
An increase in urea levels is typical with a diet with excess protein, increased protein catabolism, taking glucocorticoids, androgens; feverish conditions; increased physical activity; when the excretory function of the kidneys is weakened (glomerulonephritis; renal amyloidosis; pyelonephritis; renal tuberculosis; taking nephrotoxic drugs (tetracycline), heart failure; severe bleeding; shock; intestinal obstruction; burns; impaired outflow of urine (bladder tumor, prostate adenoma, stones in the urinary bladder); dehydration.
Reduced urea levels: in case of liver dysfunction (hepatitis, cirrhosis), phosphorus poisoning, vegetarian low-protein diet, fasting, pregnancy, in case of impaired intestinal absorption syndrome (malabsorption), hyperhydration, condition after dialysis.
Gamma GT:
Increased: liver and biliary tract disease (inflammatory processes, cirrhosis, obstructive jaundice, education, alcoholism), pancreatitis, obesity, taking toxic medications, systemic lupus erythematosus, malignant tumors, heart failure, hyperthyroidism.
Decreased: for hypothyroidism.
Total protein:
Increased: fluid loss, acute and chronic infection, autoimmune diseases, respiratory failure.
Decreased: fasting, inflammatory processes in the intestines, liver disease, injury, prolonged fever, malignant neoplasms, diabetes, kidney disease.
Alanine aminotransferase (ALT):
Increased with: liver diseases, when taking toxic medications, bile duct obstruction, cytolysis.
Decreased: Normal activity is low.
Aspartate aminotransferase (AST):
Increased: liver diseases, when taking toxic medications, bile duct obstruction, cytolysis, injuries, severe physical exertion, tumors, muscle damage.
Decreased: Normal activity is low.