If your joints are swollen and painful at night, your rheumatologist will suggest you check your rheumatology profile. This examination will help make an accurate diagnosis, monitor the dynamics of the disease and prescribe the correct treatment.
If rheumatic disease is suspected, the following tests are used:
- blood test for uric acid levels;
- blood test for antinuclear antibodies;
- blood test for rheumatoid factor;
- blood test for ACCP (antibodies to cyclic citrulline-containing peptide);
- blood test for C-reactive protein.
Blood test for uric acid levels
Uric acid is the final breakdown product of purines. Every day a person receives purines through food, mainly meat products. Then, with the help of certain enzymes, purines are processed to form uric acid.
In normal physiological quantities, uric acid is needed by the body; it binds free radicals and protects healthy cells from oxidation. In addition, just like caffeine, it stimulates brain cells. However, high levels of uric acid have harmful consequences, in particular, they can lead to gout and some other diseases.
Testing uric acid levels makes it possible to diagnose uric acid metabolism disorders and related diseases.
1
Rheumatological examination
2 Rheumatological examination
3 Rheumatological examination
When to conduct an examination:
- with the first attack of acute arthritis in the joints of the lower extremities, which arose without obvious reasons;
- with recurrent attacks of acute arthritis in the joints of the lower extremities;
- if you have relatives in your family who suffer from gout;
- for diabetes mellitus, metabolic syndrome;
- with urolithiasis;
- after chemotherapy and/or radiation therapy for malignant tumors (and especially leukemia);
- with renal failure (the kidneys excrete uric acid);
- as part of a general rheumatological examination necessary to determine the cause of joint inflammation;
- with prolonged fasting, fasting;
- with a tendency to excessive consumption of alcoholic beverages.
Uric acid level
The level of uric acid is determined in the blood and urine.
Uric acid in the blood is called urecemia , and in urine - uricosuria . An increased level of uric acid is hyperuricemia , a decreased level of uric acid is hypouricemia . Only hyperuricemia and hyperuricosuria are of pathological significance.
The concentration of uric acid in the blood depends on the following factors:
- the amount of purines entering the body with food;
- synthesis of purines by body cells;
- the formation of purines due to the breakdown of body cells due to disease;
- the function of the kidneys, which excrete uric acid in the urine.
Under normal conditions, our body maintains normal uric acid levels. An increase in its concentration is one way or another associated with metabolic disorders.
Normal levels of uric acid in the blood
Men and women may have different concentrations of uric acid in the blood. The norm may depend not only on the gender, but also on the age of the person:
- in newborns and children under 15 years of age – 140-340 µmol/l;
- in men under 65 years old – 220-420 µmol/l;
- in women under 65 years of age – 40-340 µmol/l;
- in women over 65 years of age – up to 500 µmol/l.
If excess of the norm occurs for a long time, then crystals of uric acid salt (urate) are deposited in joints and tissues, causing various diseases.
Hyperuricemia has its own symptoms, but can also be asymptomatic.
Reasons for increased uric acid levels:
- taking certain medications, such as diuretics;
- pregnancy;
- intense loads in athletes and people engaged in heavy physical labor;
- prolonged fasting or eating foods containing large amounts of purines;
- some diseases (for example, endocrine), consequences of chemotherapy and radiation;
- impaired metabolism of uric acid in the body due to a deficiency of certain enzymes;
- insufficient excretion of uric acid by the kidneys.
How to reduce uric acid levels
Those who suffer from gout know how much trouble an increased concentration of uric acid can cause. Treatment of this disease must be comprehensive and must include taking medications that reduce the concentration of uric acid in the blood (xanthine oxidase inhibitors). It is recommended to drink more fluids and reduce the consumption of foods rich in purines.
It is also important to gradually lose excess weight, since obesity is usually associated with increased uric acid. The diet should be designed so that the amount of foods rich in purines is limited (red meat, liver, seafood, legumes). It is very important to give up alcohol. It is necessary to limit the consumption of grapes, tomatoes, turnips, radishes, eggplants, sorrel - they increase the level of uric acid in the blood. But watermelon, on the contrary, removes uric acid from the body. It is useful to consume foods that alkalize urine (lemon, alkaline mineral waters).
Positive effects of hyperuricemia
Paradoxically, a high level of purine metabolic product in the blood, according to a number of researchers, has a beneficial effect on the body and allows the correction of some pathological conditions:
- Numerous studies from the 60-70s. confirmed a higher level of intelligence and reaction speed in patients with acute hyperuricemia. The chemical structure of the acid is similar to trimethylated xanthine caffeine, and as a result, it is believed to be capable of increasing performance.
- Increased acid levels promote longevity by acting as an antioxidant that blocks peroxynitrite, superoxide, and iron-catalyzed oxidative reactions. Transfusion of uric acid enhances the antioxidant activity of blood serum and improves endothelial function.
- Uric acid is a powerful neuroprotector, inhibitor of neuroinflammation and neurodegeneration, reducing the risk of Parkinson's disease and Alzheimer's disease.
However, such a positive effect is observed with an acute increase in acid in the blood. Chronic hyperuricemia leads to endothelial dysfunction and promotes the development of the oxidative process.
Antinuclear antibodies (ANA)
Using the ANA test, you can determine the presence of antinuclear antibodies (antibodies to nuclear antigens) in the blood.
ANAs are a group of specific autoantibodies that are produced by our body's immune system in case of autoimmune disorders. Antibodies have a damaging effect on the body's cells. In this case, a person experiences various painful symptoms, such as pain in muscles and joints, general weakness, etc.
Detection of antibodies belonging to the ANA group (for example, antibodies to double-stranded DNA) in blood serum helps to identify an autoimmune disease, monitor the course of the disease and the effectiveness of its treatment.
1 Blood test for ACCP
2 Blood test for C-reactive protein
3 Blood test for ACCP
When is a blood test for antinuclear antibodies necessary?
Detection of antinuclear antibodies may be a sign of the following autoimmune diseases:
- polymyositis;
- dermatomyositis;
- systemic lupus erythematosus;
- mixed connective tissue disease;
- scleroderma;
- Sjögren's syndrome and disease;
- Raynaud's syndrome;
- autoimmune hepatitis
How is the antinuclear antibody test performed?
Blood for antinuclear antibodies is taken from a vein in the elbow, on an empty stomach. Before the study, you do not have to adhere to any diet.
In some cases, in order to differentiate various autoimmune diseases, additional clarifying tests for autoantibodies from the group of antinuclear antibodies, the so-called ANA immunoblot, may be required.
What do the test data mean?
Antinuclear antibodies (another name is antinuclear factor ) indicate the presence of some kind of autoimmune disorder, but do not precisely indicate the disease that caused it, since the ANA test is a screening test. The goal of any screening is to identify people at increased risk of a particular disease.
A healthy person with normal immunity should not have antinuclear antibodies in the blood or their level should not exceed the established reference values.
A normal ANA value implies an antibody titer not exceeding 1: 160. Below this value, the test is considered negative.
A positive test for antinuclear antibodies (1:320 or more) indicates an increase in antinuclear antibodies and the presence of a disease of an autoimmune nature in a person.
Currently, two methods are used to detect antinuclear antibodies: indirect immunofluorescence reaction using the so-called Hep2 cell line and enzyme-linked immunosorbent assay. Both tests complement each other, and therefore they are recommended to be performed simultaneously.
The following types of ANA antinuclear bodies can be distinguished in the indirect immunofluorescence reaction:
- homogeneous coloring - can be with any autoimmune disease;
- spotty or speckled coloration may occur with systemic lupus erythematosus, scleroderma, Sjögren's syndrome, rheumatoid arthritis, polymyositis and mixed connective tissue disease;
- peripheral coloring – characteristic of systemic lupus erythematosus;
If the test for antinuclear antibodies is positive, it is necessary to perform an immunoblot of antinuclear antibodies to clarify the type of autoimmune disease and make a diagnosis.
Rheumatoid factor
A blood test for rheumatoid factor is aimed at identifying specific IgM class antibodies to IgG class antibodies.
A laboratory test for rheumatoid factor is a screening test aimed at identifying autoimmune disorders. The main objective of the study for rheumatoid factor is to identify rheumatoid arthritis, Sjogren's disease and syndrome and a number of other autoimmune diseases.
A rheumatoid factor test may be needed for the following symptoms:
- pain and swelling in the joints;
- limited mobility in joints;
- feeling of dryness in the eyes and mouth;
- skin rashes like hemorrhages;
- weakness, loss of strength.
1 Rheumatoid arthritis
2 Rheumatological examination
3 Rheumatological examination
Norms of rheumatoid factor in the blood
Theoretically, rheumatoid factor should not exist in a healthy body. But still, in the blood of some, even healthy people, this factor is present in a small titer. Depending on the laboratory, the upper limit of normal for rheumatoid factor varies from 10 to 25 international units (IU) per milliliter of blood.
Rheumatoid factor is the same in women and men. In older people, the rheumatoid factor level will be slightly higher.
The normal rheumatoid factor in a child should be 12.5 IU per milliliter.
Rheumatoid factor testing is used to diagnose the following diseases:
- rheumatoid arthritis;
- systemic autoimmune diseases;
- Rioglobulinemia.
Other causes of elevated rheumatoid factor
Additional reasons for increased rheumatoid factor may be the following:
- syphilis;
- rubella;
- Infectious mononucleosis;
- malaria;
- tuberculosis;
- flu;
- hepatitis;
- leukemia;
- cirrhosis of the liver;
- sepsis
If the cause of increased rheumatoid factor is an infectious disease, for example, infectious mononucleosis, then the titer of rheumatoid factor is usually less than with rheumatoid arthritis.
However, rheumatoid factor testing primarily helps to recognize rheumatoid arthritis. However, it should be emphasized that it is impossible to make a diagnosis on its basis alone. Since rheumatoid factor can be elevated in many other pathological conditions of an autoimmune and non-autoimmune nature. In addition, in approximately 30% of patients with rheumatoid arthritis, a blood test for rheumatoid factor may be negative (seronegative rheumatoid arthritis).
A blood test for rheumatoid factor is carried out in the morning on an empty stomach (8 to 12 hours should pass since the last meal).
How to prepare for the procedure?
- Blood sampling for biochemistry is always performed on an empty stomach, most often between 8 and 11 am. On the day of the procedure, it is allowed to drink still water, and the day before the procedure, heavy foods, carbonated drinks, strong coffee, tea and alcohol should be excluded from the diet.
- You should not smoke in the last hour before donating blood.
- Immediately before the procedure, try to avoid physical and emotional stress; for the last 10–20 minutes it is better to just sit near the manipulation room.
- If the date of the biochemical blood test falls during a course of drug treatment or a course of physical therapy, then it is worth consulting with a doctor - he may recommend rescheduling the test to another time or interrupting the course of treatment for several days.
ACDC
A blood test for ACCP consists of determining the titer of antibodies to cyclic citrullinated peptide and is one of the accurate methods for confirming the diagnosis of rheumatoid arthritis. With its help, the disease can be detected several years before symptoms appear.
What does the ACDC analysis show?
Citrulline is an amino acid that is a product of the biochemical transformation of another amino acid - arginine. In a healthy person, citrulline does not take part in protein synthesis and is completely eliminated from the body.
But with rheumatoid arthritis, citrulline begins to integrate into the amino acid peptide chain of proteins in the synovial membrane and cartilage tissue of the joints. The “new” modified protein, which contains citrulline, is perceived by the immune system as “foreign” and the body begins to produce antibodies to citrulline-containing peptide (ACCP).
ACCP is a specific marker of rheumatoid arthritis, a kind of harbinger of the disease at an early stage, with high specificity. Antibodies to cyclic citrullinated peptide are detected long before the first clinical signs of rheumatoid arthritis and remain throughout the disease.
Methodology of analysis and its significance
To detect ACCP, an enzyme-linked immunosorbent assay is used. A blood test for ACCP is carried out according to the “in vitro” principle (translated from Latin - in a test tube), serum from venous blood is examined. The ACCP blood test can be ready within 24 hours (depending on the type of laboratory).
Detection of ACCP in rheumatoid arthritis may indicate a more aggressive, so-called erosive form of the disease, which is associated with more rapid resolution of joints and the development of characteristic joint deformities.
If the test result for ACCP is positive, then the prognosis for rheumatoid ACCP arthritis is considered less favorable.
1 Blood test for ACCP
2 Blood test for C-reactive protein
3 Blood test for ACCP
ACDC. Reference values
The normal range for the ACCP test is approximately 0-5 U/mL. The so-called “ ACCP norm ” may vary depending on the laboratory. The “ACCP norm” values for women and men are the same.
The so-called “ Increased ACCP ”, for example, ACCP 7 units/ml or more, indicates a high likelihood of rheumatoid arthritis. An analysis result assessed as “ ACCP negative ” reduces the likelihood of rheumatoid arthritis, although it does not completely exclude it. A rheumatologist with experience in diagnosing and treating rheumatoid arthritis should always evaluate the ACCP values and interpret them; only a rheumatologist can take into account all the nuances.
To get tested for ACCP, you need to come for examination on an empty stomach.
Indications for the purpose of analysis:
- rheumatoid arthritis;
- early synovitis;
- osteoarthritis;
- polymyalgia rheumatica;
- psoriatic arthritis;
- Raynaud's disease;
- reactive arthritis;
- sarcoidosis;
- scleroderma;
- Sjögren's syndrome;
- SLE;
- vasculitis;
- juvenile RA.
If you want to know the cost of a blood test for ACCP, please call.
Contact center specialists will tell you the price of the ACDC and explain how to prepare for the study.
Transparency (turbidity)
Normal urine is clear. Cloudiness of urine can be the result of the presence of red blood cells, leukocytes, epithelium, bacteria, fat droplets, precipitation of salts, pH, mucus, urine storage temperature (low temperature promotes the precipitation of salts).
In cases where the urine is cloudy, you should find out whether it is immediately cloudy, or whether this cloudiness occurs some time after standing.
| Children | Full transparency |
| Men | Full transparency |
| Women | Full transparency |
C-reactive protein test
C-reactive protein ( CRP ) is a very sensitive element of a blood test that quickly responds to even the slightest damage to body tissue. The presence of C-reactive protein in the blood is a harbinger of inflammation, injury, and the penetration of bacteria, fungi, and parasites into the body.
CRP more accurately shows the inflammatory process in the body than ESR (erythrocyte sedimentation rate). At the same time, C-reactive protein quickly appears and disappears - faster than the ESR changes.
Due to the ability of C-reactive protein to appear in the blood at the very peak of the disease, it is also called “acute phase protein.”
As the disease enters the chronic phase, C-reactive protein decreases in the blood, and when the process worsens, it increases again.
C-reactive protein is normal
C-reactive protein is produced by liver cells and is found in minimal amounts in the blood serum. The content of CRP in blood serum does not depend on hormones, pregnancy, gender, or age.
The norm of C-reactive protein in adults and children is the same - less than 5 mg/l (or 0.5 mg/dl).
A blood test for C-reactive protein is taken from a vein in the morning, on an empty stomach.
1 Blood test for uric acid levels
2 blood test for antinuclear antibodies
3 Blood test for rheumatoid factor
Causes of increased C-reactive protein
C-reactive protein may be elevated in the presence of the following diseases:
- rheumatism;
- acute bacterial, fungal, parasitic and viral infections;
- gastrointestinal diseases;
- focal infections (for example, chronic tonsillitis);
- sepsis;
- burns;
- postoperative complications;
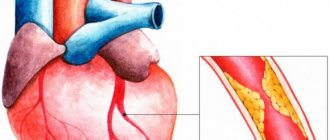
- myocardial infarction;
- bronchial asthma with inflammation of the respiratory system;
- complicated acute pancreatitis;
- meningitis;
- tuberculosis;
- tumors with metastases;
- some autoimmune diseases (rheumatoid arthritis, systemic vasculitis, etc.).
With the slightest inflammation, in the first 6-8 hours the concentration of C-reactive protein in the blood increases tenfold. There is a direct relationship between the severity of the disease and changes in CRP levels. Those. The higher the concentration of C-reactive protein, the stronger the inflammatory process develops.
Therefore, changing the concentration of C-reactive protein is used to monitor and control the effectiveness of treatment of bacterial and viral infections.
Different reasons lead to different increases in C-reactive protein levels:
- The presence of chronic bacterial infections and some systemic rheumatic diseases increases C-reactive protein to 10-30 mg/l. With a viral infection (if there is no injury), the level of CRP increases slightly. Therefore, high values indicate the presence of a bacterial infection .
- If neonatal sepsis is suspected, a CRP level of 12 mg/l or more indicates the need for urgent antimicrobial therapy.
- In acute bacterial infections, exacerbation of some chronic diseases, acute myocardial infarction and after surgery, the highest level of CRP is from 40 to 100 mg/l. With proper treatment, the concentration of C-reactive protein decreases within the next few days, and if this does not happen, it is necessary to discuss other antibacterial treatment. If after 4-6 days of treatment the CRP value has not decreased, but remains the same and even increased, this indicates the occurrence of complications (pneumonia, thrombophlebitis, wound abscess, etc.). After surgery, the more severe the operation, the higher the CRP will be.
- During myocardial infarction, protein increases 18-36 hours after the onset of the disease, decreases after 18-20 days and returns to normal by 30-40 days. With angina pectoris, it remains normal.
- In a variety of tumors, elevated levels of C-reactive protein can serve as a test to assess tumor progression and disease recurrence.
- Severe general infections, burns, sepsis increase C-reactive protein to enormous values: up to 300 mg/l or more.
- With proper treatment, the level of C-reactive protein decreases already on days 6-10.
Preparation for rheumatological tests
In order for analyzes to show objective information, it is necessary to adhere to certain rules. You need to donate blood in the morning, on an empty stomach. Approximately 12 hours should pass between taking tests and eating. If you're thirsty, drink some water, but not juice, tea or coffee. It is necessary to exclude intense physical exercise and stress. You cannot smoke or drink alcohol.
The multidisciplinary clinic "MedicCity" provides diagnostics of the highest level, experienced, qualified rheumatologists and specialists in more than 30 specialties. We treat arthritis, arthrosis, vasculitis, lupus erythematosus, osteoporosis, gout, rheumatism and many other rheumatological diseases. Do not delay your visit to the doctor, contact us at the slightest symptoms. High-quality diagnosis is 90% of successful treatment!
Urine color
The color of urine normally ranges from light yellow to deep yellow and is due to the pigments it contains (urochrome A, urochrome B, uroethrin, uroresin, etc.).
Reference values:
| Children | Various shades of yellow |
| Men | Various shades of yellow |
| Women | Various shades of yellow |
Interpretation
The intensity of the color of urine depends on the amount of urine excreted and its specific gravity. Rich yellow urine is usually concentrated, excreted in small quantities and has a high specific gravity. Very light urine is slightly concentrated, has a low specific gravity and is excreted in large quantities.
Discoloration may be the result of a pathological process in the urinary system, the effects of dietary components, or medications taken.