Hyponatremia is the most common electrolyte disturbance encountered in clinical practice. Sodium is a vital macronutrient that performs many functions in the human body (providing resting and action potential, maintaining plasma osmotic pressure, acid-base balance). A decrease in Na concentration primarily adversely affects the functioning of neurons. The bulk of cases of this condition occur in patients in intensive care units (about 15-20%). More precise statistical data on the incidence of hyponatremia are not available.
Causes of hyponatremia
Sometimes hyponatremia develops for conditionally physiological reasons. For example, sodium levels in the blood decrease in people on a salt-free diet. Hyponatremia can occur with prolonged excessive sweating (this is often observed in professional athletes and people working outdoors in hot countries). The pathological causes of the condition are as follows:
- Excess sodium loss
. Increased excretion of sodium from the body occurs with chronic diarrhea and profuse vomiting. A characteristic cause of hyponatremia is considered to be the so-called salt-wasting nephropathy, i.e. kidney diseases in which Na reabsorption in the nephron tubules is impaired (tubulointerstitial nephritis, polycystic kidney disease, congenital tubular dysfunction). - Fluid retention in the body
. A common cause of hyponatremia is pathologies characterized by impaired excretion of fluid from the body (acute or chronic renal failure, CHF, cirrhosis of the liver with ascites. Electrolyte imbalance can occur with the syndrome of inappropriate secretion of antidiuretic hormone (SIADH), which develops against the background of various diseases (endocrine, pulmonary , oncological). - Pathological hemodilution (dilution)
. An increase in water content in the vascular bed can also cause hyponatremia. This occurs when drinking excess water (non-mineral) with diabetes mellitus or diabetes insipidus, psychogenic polydipsia. Parenteral administration of large quantities of low- or salt-free solutions as detoxification therapy is a cause of iatrogenic hyponatremia. - Endocrine disorders
. Deficiency of mineralocorticoid hormones, which is observed in primary and secondary adrenal insufficiency, a salt-wasting form of congenital dysfunction of the adrenal cortex, impairs the absorption of sodium ions in the renal tubules. The cause of hyponatremia can be hypothyroidism, severe hyperglycemia in decompensated diabetes mellitus. - Taking medications
. The use of diuretics (especially thiazide and osmotic), such as hydrochlorothiazide, mannitol, to relieve emergency conditions in intensive care unit patients often causes a drop in sodium concentration. The condition can develop while taking medications such as hypoglycemic and psychotropic drugs. - Other reasons
. Hyponatremia occurs with pancreatitis, peritonitis, and massive burns. This condition is observed during some surgical procedures, especially transurethral resection of the prostate (TUR syndrome).
Regulation of water balance is normal
In the body, the secretion of vasopressin (ADH) is activated by:
- an increase in the osmotic pressure of the blood and the sodium content in the blood, to which special receptors of the heart and blood vessels (osmo-, natrio-, volumo- and mechanoreceptors) and the hypothalamic neurons themselves (central osmoreceptors) are sensitive. In adulthood and old age, the number of osmoreceptors decreases, and the likelihood of chronic dehydration increases;
- activation of the hypothalamic nuclei under any stress (pain, emotional stress, physical activity, increased body temperature);
- nicotine, angiotensin II, interleukin 6, morphine, acetylcholine and some other substances (ethanol and glucocorticoids - suppress the secretion of ADH);
- irritation of J-receptors of the lungs (located in the alveolar walls near the capillaries), this explains the possible appearance of Parhon syndrome in any lung diseases.
In the blood, ADH is not bound by plasma proteins; it is associated with platelets, which thus perform a transport function.
There are two types of membrane receptors for ADH in target tissues - V1 and V2. Stimulation of V1 receptors localized on the membrane of endothelial and smooth muscle cells of blood vessels causes vasoconstriction. Stimulation of V2 receptors in cells of the distal renal tubules increases water reabsorption and urine concentration. ADH is the only hormone that can stimulate tubular reabsorption of water without retaining sodium in the body. ADH also stimulates the absorption of water in both the exocrine glands and the gallbladder.
Pathogenesis
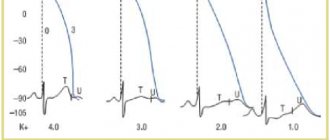
Sodium is one of the most important cations for the normal functioning of many cells, especially nerve and muscle cells. When its content decreases, the excitability of neurons and myocytes decreases as a result of changes in their membrane potential. Due to this, the formation and conduction of excitation waves in the nervous system is inhibited, the tone of skeletal muscles, blood vessels and myocardium is reduced, which causes clinical symptoms.
Hyponatremia leads to plasma hypoosmolarity; water flows along a concentration gradient from the intercellular space into the cells. As a result, edema and swelling of the cells occurs, which disrupts their normal functioning. The volume of circulating blood (volemia) may vary. This is determined by the cause of hyponatremia. With hypovolemia, the volume of blood volume decreases, and the secretion of ADH compensatory increases, which further aggravates the pathology.
Forecast
The prognosis is generally favorable, but depends on the nature of the underlying disease and the cause of inadequate ADH secretion. Severe forms of Parhon's syndrome can be fatal as a result of severe water intoxication.
Sources
- National leadership. Brief edition. Edited by I. I. Dedov, G. A. Melnichenko. M., 2011. - 741 p.
- Guide to Medicine. Diagnosis and treatment. Second edition. Translation from English under the general editorship of A. G. Chuchalin. M. - 2011. - 3693 p.
- Evidence-based endocrinology. Translation from English edited by G. A. Melnichenko, L. Ya. Rozhinskaya. M. - 2009. - 632 p.
- Treatment of diseases of internal organs. Volume 2. A. N. Okorokov. M. - 2007. - 596 p.
- Clinical endocrinology. Management. Edited by N. T. Starkova. 3rd edition. St. Petersburg - 2002. - 576 p.
Classification
There are several types of hyponatremia:
- Pseudohyponatremia
. It is caused by a decrease in the proportion of the water part of the blood due to a large amount of proteins and lipids. - Hypertensive hyponatremia
. It develops as a result of the movement of water from cells into the interstitial space due to the presence of highly osmotic substances (glucose, mannitol) in the blood. - Hypotonic hyponatremia
. Depending on the BCC it is divided into:
- Hypovolemic. Characterized by a deficiency of Na and water, and a decrease in BCC. It is observed in salt-wasting nephropathies, mineralocorticoid deficiency, vomiting and diarrhea.
- Isovolemic. This form occurs in SIADH, in which water retention and increased natriuresis occur.
- Hypervolemic. With this type, intravascular volume decreases due to the diffusion of fluid into various body cavities (abdominal, thoracic), which leads to increased secretion of ADH and “dilution” of sodium. This is typical for CHF and liver cirrhosis.
According to severity, hyponatremia is divided into:
- Light
– from 130 to 134 mmol/l. - Moderate
– from 125 to 129 mmol/l. - Severe
– less than 125 mmol/l.
According to the rate of development, hyponatremia is:
- Acute
– lasting up to 48 hours. - Chronic
– lasting more than 48 hours.
Pathophysiology
The syndrome is based on an imbalance of fluid in the body: water intake exceeds its removal. Most patients continuously secrete ADH or ADH-like peptides despite plasma hypoosmolarity. Overproduction of ADH leads to water retention, decreased plasma osmolarity, renal sodium loss, and hyponatremia, but low plasma sodium and hypervolemia do not cause a compensatory, adequate decrease in ADH synthesis. Hypervolemia suppresses aldosterone production, thereby exacerbating sodium loss.
Aldosterone regulates sodium reabsorption in the distal tubules of the kidneys and retains sodium.
Under conditions of hypervolemia, the secretion of atrial natriuretic factor increases, which also promotes sodium excretion. Thus, the pathophysiological basis of the syndrome of inadequate ADH production is: loss of sodium in the urine; hyponatremia, suppressing the thirst center; hypervolemia leading to water intoxication.
Symptoms of hyponatremia
Clinical symptoms depend on the rate of onset and severity of hyponatremia. With a mild and slowly developing decrease in Na levels, there are no serious symptoms of central nervous system damage. There may be slight drowsiness and imbalance. In severe cases, severe somnolence and a soporous state appear. The person begins to react poorly to external stimuli. Epileptiform seizures are characteristic.
Due to a decrease in myocyte excitability, vascular tone and myocardial contractile function, muscle weakness and symptoms of arterial hypotension (increased heart rate, dizziness, loss of consciousness) appear. The skin and mucous membranes become dry, skin turgor and elasticity decrease. Sometimes there is a decrease in diuresis, gastrointestinal symptoms - loss of appetite, nausea.
Clinical picture
Parhon syndrome rarely develops on its own, and the patient is primarily concerned about the manifestations of the underlying disease. The leading clinical manifestations are symptoms of impaired consciousness; rarely (with severe hyponatremia and water intoxication) an increase in body weight and the formation of edema due to water retention due to oliguria are possible. The severity of clinical manifestations is determined by the degree of hyponatremia.
When the sodium concentration in the blood is below 120 mmol/l (normal: 120–150 mmol/l), symptoms of increased intracranial pressure are characteristic: headache, drowsiness, nausea and/or vomiting, muscle weakness, muscle spasms, convulsions. When the sodium content in the blood is less than 110 mmol/l, confusion, psychosis, disorientation, decreased body temperature, decreased tendon reflexes, and pseudobulbar palsy are noted. With a further decrease in sodium concentration in the blood, coma develops and death occurs.
Diagnostic criteria
- Hyponatremia in combination with a corresponding decrease in blood osmolality.
- Urine osmolality is higher than plasma osmolality.
- Renal sodium excretion is more than 20 mmol/l (normal for adults: 10–20 mmol/l).
- There is no arterial hypotension, hypovolemia and pronounced edema syndrome, as with hypothyroidism and adrenal insufficiency, etc.
- There is no dysfunction of other organs (kidneys, adrenal glands, thyroid gland).
Osmolality is the concentration of osmotically active particles in a solution, expressed in the number of osmoles per kilogram of solvent. One of the main constants of the human body fluctuates within insignificant limits and depends mainly on the concentration of sodium, glucose and urea ions.
Complications
A large number of complications are typical for this syndrome. The overwhelming majority of adverse effects are associated with damage to the central nervous system. These include coma, swelling and herniation of the brain. Pulmonary edema, infarctions of the hypothalamus and posterior pituitary gland are sometimes observed. A fatal outcome at a Na level of 125 mEq/L occurs in 25%, with levels below 115 mEq/L – in 50% of cases.
A dangerous complication of improper treatment of hyponatremia is osmotic demyelinating syndrome (pontine and extrapontine myelinolysis), which develops as a result of dehydration and shrinkage of brain cells due to a sharp increase in plasma osmolarity with too rapid administration of saline solutions. Symptoms include dysphagia, bulbar abnormalities, and tetraplegia. The mortality rate for this syndrome reaches more than 50%.
Etiology
ADH hypersecretion syndrome can develop with various diseases and taking certain medications. Thus, with damage to the central nervous system, the development of the syndrome is due to an increase in the production of ADH by the pituitary gland. Malignant neoplasms can themselves produce ADH, regardless of the hypothalamic-pituitary link, while hypersecretion of ADH develops as part of the paraneoplastic syndrome, but more often it has a mild, erased form of the course and is detected quite late, so it cannot become a marker of tumor growth at an early stage. Another common cause of ADH overproduction is acquired immunodeficiency syndrome ( AIDS ). In AIDS, the syndrome of inadequate ADH production can be a consequence of bacterial or viral infections of the lungs and central nervous system. Parhon syndrome often develops in older people and patients with chronic somatic pathology.
Main causes of ADH hypersecretion
| CNS damage | Stroke Hemorrhage Neoplasms Infections Hydrocephalus Hypophysectomy via transsphenoidal approach Lupus erythematosus Acute intermittent porphyria |
| Malignant neoplasms | Small cell lung cancer Pharynx cancer, thymoma Pancreatic cancer Bladder cancer Lymphoma, sarcoma Cancer of other organs (prostate, duodenum, ovaries, mesothelium) |
| Damage to the respiratory system due to stimulation of J-receptors | Infections (pneumonia, abscess, tuberculosis) Bronchiectasis Artificial ventilation |
| Taking medications | Psychotropic drugs (neuroleptics, tricyclic antidepressants, selective serotonin reuptake inhibitors, carbamazepine) Neurological drugs (narcotic analgesics, amphetamines) Acetylcholinesterase inhibitors Antineoplastic drugs (vincristine, vinblastine, cyclophosphamide) Endocrinological drugs (oxytocin, desmopressin, clofibrate) |
| Infectious diseases indirectly through IL-6 | Diseases of the central nervous system and respiratory system AIDS |
| Idiopathic |
Diagnostics
Almost all patients with hyponatremia, especially severe, should be under the joint supervision of a resuscitator and a specialized specialist (endocrinologist, nephrologist). To determine the cause of this syndrome, anamnestic data are important - previous diarrhea, vomiting, taking medications. Identifying the specific type of pathology helps to identify signs indicating dehydration - dry skin, hypotension, decreased diuresis.
Information about the patient's concomitant diseases is also required. During the examination, attention is paid to symptoms such as swelling of the face, lower extremities, enlargement and tension of the abdomen, dilatation of the saphenous veins on the anterior abdominal wall. An additional examination is prescribed to determine the type of hyponatremia and determine its cause:
- Laboratory research
. Serum osmolarity and the level of other electrolytes (potassium, calcium, magnesium) are determined. In a biochemical blood test, the content of glucose, liver enzymes (ALT, AST), and kidney function indicators (urea, creatinine) are measured. The level of thyroid and adrenal hormones (TSH, free T4, cortisol) is studied. The quantity, osmolarity, specific gravity of urine, the concentration of Na and glucose in it, and the presence of ketone bodies are checked. - Instrumental Research
. The most important clinical value is the measurement of central venous pressure (CVP). This is the most accurate way to determine the volume of blood volume, which allows you to clarify the type of hyponatremia (hypovolemic, hypervolemic or euvolemic). If pulmonary edema is suspected, a chest X-ray is performed; if there are symptoms of cerebral edema, a CT scan of the brain is performed.
This condition must be differentiated from hypernatremia, since both of these pathologies have almost completely identical clinical symptoms. Cerebral edema during hyponatremia should be distinguished from cerebral edema of other etiologies (hypertensive crisis, stroke, traumatic brain injury). It is much more important to differentiate the varieties of this syndrome (hyper-, hypo-, euvolemic, hyper- and hypotonic).
Treatment
The treatment algorithm for hyponatremia depends on the severity of the electrolyte disturbance, its duration, and the characteristics of clinical manifestations (hypovolemia, hypervolemia, cerebral edema).
In case of hypovolemic variant, intravenous administration of isotonic sodium chloride solution is prescribed. The volume and rate of administration required for correction are calculated by the doctor in each specific case using special formulas.
If the cause of hyponatremia is too large a volume of infusion of hypoosmolar solutions, then it is necessary to limit further fluid intake into the body and correct the content of sodium ions.
To correct hyponatremia, administration of isotonic sodium chloride solution is indicated.
Elimination of hyponatremia, especially with severe clinical manifestations, should be carried out with great caution and gradually. This approach reduces the risk of developing neurological disorders, including life-threatening ones.
Simultaneously with the correction of water and electrolyte balance, therapy is carried out for the diseases and conditions that caused its occurrence.
Treatment of hyponatremia
Most often, patients with hyponatremia are hospitalized in the intensive care unit. First, you need to stop taking medications that can cause hyponatremia and stop administering hypotonic solutions. You can additionally prescribe the intake of ordinary table salt orally. Sometimes with mild hyponatremia this is enough. For moderate to severe cases, the following treatment is provided:
- Fluid restriction
. This is the main condition for the treatment of the hypervolemic form, as well as SIADH. Fluid intake, both orally and in the form of solutions, should not exceed 1000 ml/day. - Introduction of saline solutions
. Infusion therapy with a 0.9% NaCl solution is necessary both to eliminate sodium deficiency and to maintain blood volume in the hypovolemic form. At the same time, it is necessary to compensate for the deficiency of other electrolytes. If pronounced neurological symptoms occur, hypertronic (3%) NaCl is administered. To prevent osmotic demyelinating syndrome, monitoring the rate of increase in serum sodium levels is mandatory; it should be less than 0.8 mmol/day. - Diuretics
. Used to remove excess fluid in hypervolemic form. Loop diuretics (furosemide) are used for this purpose. Thiazide diuretics are strictly contraindicated as they worsen hyponatremia. - ADH blockade
. Since hyponatremia often causes increased secretion of ADH (vasopressin), measures to suppress its effect are important. Demeclocycline and ADH receptor antagonists (conivaptan, tolvaptan) have an inhibitory effect on ADH. However, these medications should be avoided in patients with kidney disease.
Since hyponatremia itself is a very dangerous condition that can lead to death in a short time, the sodium level is first corrected. Therefore, only after eliminating the symptoms of threatening cerebral edema do they begin to treat the disease that caused hyponatremia:
- CHF
: ACE inhibitors, beta-blockers, loop diuretics. - Liver cirrhosis
: administration of albumin, transfusion of fresh frozen plasma, avoidance of alcohol. - Endocrine disorders
: hormone replacement therapy with fludrocortisone, hydrocortisone (for adrenal insufficiency), levothyroxine (for hypothyroidism). - Chronic renal failure
: hemodialysis.
Differential diagnosis
When carrying out differential diagnosis, it is first necessary to exclude diseases of the liver, kidneys, heart, adrenal insufficiency and hypothyroidism. The greatest difficulties arise when trying to differentiate the diagnosis from idiopathic edema syndrome - a disease that has many clinically similar symptoms, but a different pathophysiological nature (pathogenesis is associated with a number of neurogenic, hemodynamic and hormonal changes leading to dysregulation of water-salt homeostasis). This syndrome is characterized by the development of peripheral or widespread edema. ADH is elevated in all patients with Parhon's syndrome, while in idiopathic edema, an increase in ADH is rarely observed, and hyponatremia and hypervolemia are never observed in idiopathic edema.
Prognosis and prevention
Hyponatremia is a dangerous life-threatening condition with a fairly high mortality rate (from 25 to 50% of patients die in various forms of this pathology). According to some authors, the mortality rate reaches 65%. The cause of death is mainly cerebral edema and coma. However, with timely and competent treatment, serious complications do not occur.
An unfavorable outcome may be neurological disorders such as dysphagia, dysarthria and tetraplegia due to generalized demyelination of nerve fibers due to inappropriately rapid correction of serum Na. Prevention of this condition comes down to timely treatment of those diseases that could potentially cause hyponatremia, and regular monitoring of plasma sodium levels.