Most abdominal organs are supplied with blood from the celiac trunk, the superior and inferior mesenteric arteries and their branches. This ensures the flow of nutrients and oxygen to the tissues.
The danger of the disease lies in the fact that its symptoms are significantly similar to the clinical picture of many diseases of the digestive tract, which is what makes diagnosis difficult. Exacerbation of the disease can have tragic consequences, so timely diagnosis and treatment are extremely important.
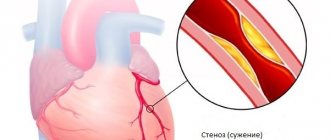
The mechanism of development of the disease is long-term disruption of blood flow and ischemic processes. To varying degrees, this disease occurs in more than half of elderly patients. The acute stage of the disease is intestinal infarction or acute occlusion of abdominal vessels. The pathology is also known as abdominal toad or tonsillitis.
The disease is divided into celiac, superior and inferior mesenteric forms. It depends on the vessel that is involved in the process. Each form has its own characteristic symptoms, which arise depending on the location of the outbreak. Also, abdominal ischemia occurs in several stages. The first stage is compensation, when the disease manifests itself slightly, and the vessels continue to provide blood flow. The subcompensated stage is accompanied by a deterioration in the function of the abdominal vessels, which is manifested by a pronounced clinical picture. Decompensation occurs when the damage to the vessel is so great that it completely disrupts the blood supply to the tissue.
Why does abdominal ischemia occur and how does it manifest?
Factors that lead to blockage or narrowing of a vessel are divided into intravasal (those that act directly inside the artery) and extravasal (factors whose influence is directed from the outside).
The following are common intravasal causes of abdominal ischemia:
- atherosclerotic changes in the abdominal aorta and its branches;
- changes in the vascular wall against the background of aortoarteritis;
- periarteritis nodosa;
- hypoplasia of the vascular wall;
- aortic aneurysm in the abdominal region;
- the formation of pathological connections between an artery and a vein - fistulas;
- fibromuscular dysplasia of the abdominal arteries.
Extravascular risk factors include:
- compression of the artery lumen by a fibrous cord;
- features of the placement of the “legs” and ligaments of the diaphragm;
- tumor of internal organs;
- scar tissue or adhesions in the abdominal cavity.
The clinical picture of abdominal ischemia is varied and in many ways similar to other pathologies of the abdominal cavity. The main symptom of disease is pain. It can be observed in various parts of the abdomen. You can trace the connection between its occurrence and food intake. Most often, pain occurs 30-40 minutes after eating. Minor relief occurs in a forced position, when the patient becomes in a knee-elbow position.
In addition to pain, abdominal ischemia is accompanied by symptoms such as:
- weight loss;
- general weakness and exhaustion.
- nausea and vomiting;
- stool disorders (constipation and diarrhea);
- feeling of bloating;
Patients eat less often, because every meal is accompanied by painful symptoms. This leads to a lack of nutrients and weakness. Frequent pain and unpleasant phenomena lead to disorders of a person’s psychological state.
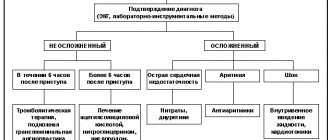
Atypical heart attacks
The classic symptoms of myocardial infarction are known to many people today. A sign of this formidable cardiac pathology is sudden sharp - so-called "dagger" - pain in the heart or behind the sternum, which can radiate to the left lower jaw, left arm, left shoulder or under the left shoulder blade. Along with the pain, there is a feeling of lack of air, shortness of breath, fear of death, cold pouring sweat and severe weakness.
This is a typical full-blown clinical picture of a heart attack, the so-called anginal variant. It allows you to immediately suspect a heart problem, provide first aid and promptly call an ambulance. However, unfortunately, not all heart attacks have a typical course. This is especially true for people over 75 years of age, in whom the proportion of atypical heart attacks is about 30%.
Diagnostic program for abdominal ischemia
Diagnosis of the disease must take into account the patient's symptoms and have a combined approach. The doctor clarifies the patient’s complaints, asks about the time of their occurrence and characteristics. To assess the function of the abdominal vessels, auscultation is performed - that is, listening to noises. They can occur when the celiac and mesenteric arteries are narrowed. Sometimes phonoenterography is used - this is an image of vascular murmurs on a graph.
Research methods used for abdominal toad
- vascular angiography, which will confirm or exclude the presence of stenosis and occlusion;
- plain radiography of the abdomen, which can determine calcification of the aortic walls;
- endoscopic studies that will help visualize changes in the mucous membrane, erosion, ulcers;
- analysis of feces will show digestive disorders, in which the amount of mucus and undigested particles in the feces is increased.
Also, methods such as scintigraphy, ultrasound duplex scanning, ultrasound of the abdominal organs, and flowmetry are used. Sometimes, in the process of diagnosing abdominal ischemia, diagnoses are made: gastritis, peptic ulcer, cholecystitis, pancreatitis.
Does your stomach or heart hurt? Abdominal form of myocardial infarction
A heart attack does not always cause chest pain. Sometimes it manifests itself as nausea, vomiting, indigestion, and abdominal pain. Which makes us wonder about the root cause of such complaints. Abdominal form of myocardial infarction. Is it worth doing a cardiogram for abdominal pain?
Why does my stomach hurt and my heart cells die?
The reasons for the development of an atypical heart attack are no different from the classic one: progressive atherosclerosis, high cholesterol, vasoconstriction, high blood pressure. Where do abdominal pains come from? It turns out that the pain syndrome is caused by damage to the lower wall of the heart muscle, which is located close to the diaphragm. This explains why the pain radiates to the stomach. After a few days, necrosis (death) spreads throughout the heart muscle so much that the pressure drops and the pain moves to the chest. The name of the abdominal form is directly related to abdominal pain (from the Latin abdomen - belly).
Cholecystitis, pancreatitis, diarrhea... How not to miss a heart attack
The most understandable option is when abdominal pain first appeared due to dietary errors. We suspect gastritis and are looking for the cause. It is more difficult if chronic gastritis, cholecystitis, pancreatitis or an ulcer were identified a long time ago. Then the usual painkillers are used, despite the lack of effect. Having consumed a week's supply of medications in a few days, pale due to low blood pressure, they only then seek medical help.
If digestive disorders (loose stools, vomiting, abdominal pain) come to the fore, patients can go to the infectious diseases department with suspected poisoning.
Consider a heart attack if you have digestive disorders
With the abdominal form of a heart attack, the upper abdomen hurts (under the stomach, right half, especially the right hypochondrium). The pain is severe, suddenly onset, burning, accompanied by nausea, vomiting, bloating, and loose stools.
The alarming thing is that they are provoked, in addition to physical activity and stress, by eating. The pain changes in character: it intensifies, is less tolerated, becomes oppressive, changes location, lengthens (gradually increasing, reaching its peak within an hour), makes you panic and be afraid of death. The effect of nitroglycerin is short-term, sometimes it is not at all.
Don't forget about an electrocardiogram for abdominal pain
Sudden severe abdominal pain is an indication for taking an electrocardiogram before prescribing pills and injections. Therefore, if atypical abdominal pain appears, radiating to the middle of the chest, it would be more correct to contact a medical institution to conduct this research method.
What to do before the ambulance arrives
Treatment of the abdominal form of heart attack is carried out in a hospital. But what about emergency medical care before entering the hospital if the pain occurs at home? You won’t chew aspirin every time you experience stomach pain or nausea. After 5-6 such attempts, your stomach will answer you with an ulcer, with which you will certainly end up in the hands of doctors. If the attack drags on and the pressure allows (figures greater than 140/80 mm Hg), take a tablet or nitroglycerin spray and listen to the pain. If it becomes dull, call an ambulance and rely on their professionalism.
What is the danger of abdominal pain associated with a heart attack?
The prognosis of any heart attack is always worse if the time from the onset of the first symptoms to medical care and admission to the hospital is delayed. In the case of the abdominal form, the likelihood of delaying treatment is high. The patient, of course, will not die, but the dead heart cells cannot be resurrected.
Cardiologist at the Lutik polyclinic Irina
Modern methods of treating abdominal ischemia
In the early stages of the disease, conservative therapy is used. it involves modification of eating habits. Patients are advised to eat small portions and also avoid rough foods and foods that stimulate the production of gases. Medication assistance consists of taking antispasmodics that expand the lumen of the vessel, anticoagulants, and blood circulation stimulants. Such assistance is sufficient at the compensation stage. Regular use of medications and compliance with recommendations will prolong the compensation stage.
For subcompensated and decompensated abdominal ischemia, surgical intervention is indicated. This can be a conditionally reconstructive operation - impact on the legs of the diaphragm, removal of cords. Reconstructive surgery - decompression, vascular bypass. their dilatation and stenting. Minimally invasive intervention on the vessels of the abdominal cavity - angioplasty and stenting). Surgical and minimally invasive treatment methods ensure the restoration of blood supply to the suffering organ. expansion of the lumen of the vessel, and installation of a stent is the prevention of relapse of the disease. The operation is performed under anesthesia. Modern techniques allow it to be carried out in a short time and with minimal trauma.
Features of the postoperative period
After the operation, the patient is under the supervision of medical personnel for some time. The state of health and digestion processes are gradually normalized. In the early period after surgery, it is recommended to take medications and correct the condition after anesthesia.
If the patient has a stent installed, anticoagulant and antiplatelet drugs are indicated, which are necessary to prevent thrombus formation.
In order to evaluate the result of treatment, the attending physician conducts a study of the condition of the blood vessels and observes the patient over time. It is necessary to attend prescribed consultations and studies, as there is a risk of relapse of the pathology.
In order to receive treatment, you must consult a doctor. After the diagnostic methods have been carried out and an accurate diagnosis has been made, the doctor will, if necessary, set a date for intervention.
Abdominal pain and intestinal pathology. Diagnostic issues, treatment approaches
Vladimir Trofimovich Ivashkin , academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
– Message from Marina Fedorovna Osipenko, professor from Novosibirsk.
Marina Fedorovna Osipenko , professor:
– Good afternoon, dear colleagues, dear Vladimir Trofimovich! The problem that I would like to discuss and touch on today concerns abdominal pain and intestinal pathology, issues related to diagnosis and treatment approaches. It seems to me that the fact that we began to discuss not only the nosological approach to patient management, but also the syndromic one, is actually very important, because especially for primary care doctors - and not only for primary care doctors, and for specialized specialists – patients do not come with a ready-made diagnosis, patients come with symptoms, syndromes, and, of course, our task is to verify the cause of these symptoms and syndromes, to build a nosological diagnosis. But on the other hand, our task is to ensure a certain quality of life for our patients even at the time of examination, and on the other hand, of course, to provide assistance in relieving symptoms and syndromes.
So, dear colleagues, you and I know very well that chronic pain - and in the vast majority of cases and most often we still encounter just such pain - affects 19-20% of the adult population. That is, almost every fifth person suffers from various manifestations or various causes, so to speak, underlying the occurrence of pain, and, of course, abdominal pain is one of the very serious symptoms for which our patients suffer greatly. Of course, we must remember very seemingly simple points, but they are very important so that you and I, in addition to identifying the abdominal pain itself, can also identify the causes of its occurrence. We all know very well from our student days that the mucous membrane does not have pain receptors, and accordingly, even severe lesions of the mucous membrane are often not accompanied by any pain. On the other hand, we understand that changes in pressure in the lumen of a hollow organ, which undoubtedly includes the entire intestine, lead to the activation of nociceptive receptors and the appearance of various pain sensations, just like the parietal peritoneum and mesentery , and in the end this is very, I emphasize once again, important, and you and I understand this, in order to verify the cause of pain.
Actually, it has long been clear that the level and threshold of pain perception is very different for everyone, and now a large amount of research in the world is devoted specifically to the genetics of pain, and more and more research concerns the enzymes involved in the metabolism of catecholamines and enkephalins, and features in the structure of the metabolism of opioid receptors, and genes that transfer afferent neurons, just like the genes that determine the transport of potassium, calcium, sodium ions, and so on. It is absolutely clear that in many respects the subjective perception of pain (and you and I perfectly understand that pain is a subjective manifestation of one or another degree of ill-health on the part of different systems and organs), it is determined precisely by a number of complex genetic factors, because one and the same In fact, a stimulus, if assessed even from some strict physical parameters, evokes completely different sensations in the patient. And we must, despite seemingly very banal things, clearly understand that in order to move from the syndrome to the actual nosological form, we must verify abdominal pain well enough and understand the possible mechanism of its occurrence.
We must find out the duration of the pain, we must find out its nature, we must find out its localization, we must try to determine whether its genesis is functional or organic, we must try to determine the mechanism of its formation, while taking into account and taking into account that in origin, despite localized in the abdominal area, this may not only be a pathology of the gastrointestinal tract itself, but it may also be manifestations from other systems and organs. Therefore, purely propaedeutic things were, are and remain very important in order for us to get out or move on, strictly speaking, to a diagnostic search. This is a necessary option for a normal diagnostic search. Of course, in most cases, we, gastroenterologists, and therapists in general, most often encounter subacute or chronic pain, that is, pain that lasts more than two days, let’s say. Acute pain in most cases is still the destiny of surgery, although any pain that later becomes chronic, it certainly begins at some point.
Of course, such moments as colic, which is still more associated with an increase in intraluminal pressure, or pain of an inflammatory nature, is more well localized, of a constant nature, more acute in the subjectivity of sensations, or ischemic in nature, with increasing intensity, aching , constant, around the clock - all this also helps us to verify the diagnosis in the same way as the localization of pain. If we are now focusing, or I am emphasizing in my message, on intestinal diseases that are manifested by abdominal pain, then we also know very well the places of localization of pain associated with the intestines - these are the lower abdomen or the right upper quadrant of the abdomen. The same important point is the attempt to determine the leading mechanism of the formation of abdominal pain, because we know very well that parietal pain is always the involvement of the peritoneal cover. It is clearly localized, it is accompanied by varying degrees of muscle tension, and the example that Vladimir Trofimovich gave at the very beginning of our round table once again emphasizes that the presence of parietal pain in the patient was not accompanied by the classic manifestations of this disease, but for all that in Ultimately, this situation turned out to be so. It intensifies with a change in body position, coughing, and, of course, if there is a suspicion that the pain is of a parietal nature, without a doubt, consultation with a surgeon and the surgeon’s participation in the management of patients must be mandatory.
Visceral pain - this is what we mostly encounter - this is precisely a change in pressure, stretching, tension, perhaps a circulatory disorder, this is the involvement of nosoceptive factors, and so on. In most cases, we are faced with precisely this genesis of pain. Referred, referred pain also gives us a lot of problems, since we often deal with it, and, of course, not arising in the place where the organ is projected, it gives us a lot of problems. Well, and, finally, psychogenic, which, essentially, we can diagnose only by the method of exclusion and with the help of completely different, very weak, let’s say, inherently tests. Of course, parietal pain is always an organic disease, without a doubt. As for organic diseases, in the initial stages, or rather, not even in the initial stages, but in the absence of complications, they can be accompanied by visceral pain. As soon as a reaction from the peritoneum occurs, it is, without a doubt, parietal pain.
Functional diseases are always visceral pain plus psychogenic pain, plus there may be components of radiating pain. The scope of examinations is different for all patients, and this, in fact, is a big task, because if all patients with abdominal pain are examined in depth using everything that is available in the world today, then, in general, not in any of the most developed civilized The country will not have enough such opportunities. Therefore, our task as doctors is, first of all, to outline for each patient, in each specific clinical situation, our own reasonable algorithm of actions and our own reasonable list of those examinations that will help us diagnose pathology. Of course, even such a method - I say “even”, because there was a time when a lot of people put their faith in laparoscopy and believed that this was a method that allowed practically, well, almost in 100 percent of cases, to reach the nosological form - in fact in fact, without a doubt, it has justified itself in this sense quite relatively, because a very specific list of nosological forms or pathological situations allows us to identify, and laparoscopy does not always allow us to get out, as I already said, and as you and I know very well , to a specific nosological form.
And now a review, in general, ten years ago, but quite correctly, let’s say, carried out, showed that from 10 to 15% of patients who underwent laparoscopy, essentially, were left, let’s say, without a definite diagnosis, because Laparoscopy was not helpful in diagnosing the cause of abdominal pain in these patients. Of course, today, gastroenterology especially is still a field of medicine in which the scope of the examination is largely determined by whether the patient has symptoms of anxiety or does not have these symptoms of anxiety. And you and I, understanding, on the one hand, the seemingly banality of these symptoms of anxiety and, it would seem, their obviousness, on the other hand, we must clearly understand that such moments as the nocturnal nature of pain, as the onset of the disease after 50 years , such as the presence of oncological or organic diseases in the family, if we are now talking about intestinal diseases, this is inflammatory bowel disease celiac disease, this is fever and loss of body weight, these are changes in direct examination of the patient, changes in the size of organs, these are changes in laboratory parameters - and routine ones, and the results of instrumental research methods, they force us, of course, to examine patients in more depth, because these are signals and markers of organic pathology. If we talk about intestinal diseases in general, then, of course, the most common cause of chronic abdominal pain is irritable bowel syndrome.
We all know the criteria very well, since they have practically not changed since 2006, and we understand that the leading one here is precisely recurrent abdominal pain, which is associated either with the fact of defecation, or with a change in frequency, or with a change in the shape of stool. And we perfectly understand that in order to diagnose irritable bowel syndrome, these are all the criteria that are listed and which are recommended to us by the Rome recommendations, all these criteria must be very strictly observed. Then, indeed, with a clear history and consistency of these symptoms, the likelihood of irritable bowel syndrome is high. This is visceral pain, and chronic, with a complete absence of anxiety symptoms. Moreover, it is chronic, that is, they arose, these pain sensations and these disorders, within six months. At the same time, we understand that despite the fact that this nosological form is called a syndrome, it is, in general, an independent nosological form, and issues related to the pathogenesis of its occurrence, the pathophysiology of its occurrence, are repeatedly discussed and very actively studied.
In doing so, we understand that if we clearly meet the criteria, the likelihood of irritable bowel syndrome—this is data relevant to previous irritable bowel syndrome recommendations—is 93%. However, irritable bowel syndrome can be masked, so to speak, or combined with some other diseases. These include enteropathies, inflammatory bowel diseases, parasitic colitis, lymphocytic/allergic colitis, bacterial overgrowth syndrome, diverticular disease, and endometriosis. Moreover, we must understand that there may be several options here. On the one hand, these may be similar syndromes of irritable bowel syndrome and intestinal diseases, and the second very important point is that there may be an overlap, that is, the presence of both intestinal diseases of an organic nature and at the same time irritable bowel syndrome. That is, when we encounter symptoms that are included in the criteria for the diagnosis of irritable bowel syndrome, we must understand that symptoms of another disease may be hidden behind them, or this may be the intersection of organic pathology and purely functional pathology.
If we consider approaches to the treatment of irritable bowel syndrome, there are a lot of guidelines. One that is fairly widely cited and not the most recent is the American College of Gastroenterology. Antispasmodics occupy a significant place there, they have a fairly good, let’s say, level of evidence, and it is m-anticholinergics that are predominantly discussed, and selective m-anticholinergics, when they talk about evidence-based therapy for IBS. But, however, if we are talking about what we must first differentiate irritable bowel syndrome from, then according to the recommendations of the World Gastroenterological Organization, celiac disease and parasitic diseases are most similar to IBS. Therefore, in patients with classic IBS manifestations, without symptoms of anxiety, we must exclude celiac disease, we must also exclude parasitic diseases. And then the most alarming from the point of view of other organic diseases are patients who have persistent diarrhea. Now, if we look at celiac enteropathy, today there are quite clear diagnostic recommendations in the world. They are based on determining, first of all, antibodies to transglutaminase, in addition, on determining the level of endomysial antibodies and the characteristics of the HLA system.
But in any case, when we talk about enteropathy, this is, of course, visceral pain, this is persistent diarrhea syndrome, this is the presence of varying degrees of melaabsorption, although melaabsorption may be absent, and extraintestinal symptoms that are characteristic of celiac enteropathy. Approaches to the treatment of celiac enteropathy in general are quite clear, although in some cases, in the presence of abdominal syndrome, we also always think whether this is an overlap with IBS or whether abdominal syndrome is somehow associated with the actual course of enteropathy, although in general this is not the most characteristic of this pathology symptom. If we talk about inflammatory bowel diseases, here, in fact, there may also be two classic situations, and mainly when we are faced with Crohn's disease due to obstruction or deep inflammation affecting the mucous membrane, submucosal layer, reaching the muscle layer, there may be a reaction with side of nociceptive receptors, so pain may occur, and the second option is, of course, crossover, the coexistence of these two nosological units. Here is the coexistence of two nosological units - studies have shown that in the population 30% of patients with ulcerative colitis suffer from IBS-like syndromes, with Crohn's disease this situation is more common.
And in one of Drossman’s latest reviews on inflammatory bowel diseases, IBS-like syndrome, in addition to the fact that we are trying to relieve pain by prescribing specific therapy for the treatment of inflammatory bowel diseases, we also use a different approach to treat pain, namely - inclusion of antidepressant drugs, antispasmodics and drugs that affect motor skills. The next nosological form that we include in the range of differential diagnosis is the syndrome of bacterial overgrowth in the small intestine. If we look and remember once again the symptoms that are associated with this pathology, we see many similar symptoms to irritable bowel syndrome. This is the same visceral pain, in most cases chronic, and symptoms of anxiety are not always present in these patients. In any case, a lot is now being said and written about the intersection of IBS with bacterial overgrowth syndrome, and it occurs in a large percentage of cases, and the important point is that, of course, there is specific treatment directly aimed at this bacterial overgrowth, but in a number of cases, we must also stop the manifestation of an IBS-like symptom complex in these patients.
The next situation, which is by no means rare, is diverticular disease, and at the same time, of course, in a number of patients it can be asymptomatic, in some cases we may encounter diverticulitis or other complications of diverticular disease, and finally, there is the term “symptomatic diverticular disease.” disease" is the presence of chronic abdominal pain, a violation of intestinal passage, which is very similar to the manifestation of irritable bowel syndrome. If we talk about the features of abdominal pain with diverticulitis, then we understand that this pain is visceral, with the addition of a parietal component, if we are talking about significant thinning of the walls of this diverticulum. As a rule, there are symptoms of anxiety - these are such as fever, such as accelerated ESR, such as increased levels of C-reactive protein. The pain, as a rule, is local, intensifies with movement, which indicates that the parietal component of this pain is attached, and, of course, age, without a doubt, is very important.
If we talk about symptomatic diverticular disease, the question is debated - whether it is segmental colitis, or whether it is simply concomitant irritable bowel syndrome. There are a lot of ideas expressed, but, indeed, it is very similar to irritable bowel syndrome in its manifestations, except, of course, for age. Since we understand that diverticular disease is the lot of people in older age groups, here, of course, age plays a very significant role in order for us to suspect this particular pathology in our patients. If we talk about approaches to treatment, then in uncomplicated acute diverticulitis, pain relief is an important section, and it is discussed in the guidelines that exist in individual countries. It should be understood that non-steroidal anti-inflammatory drugs worsen the course of acute diverticulitis, therefore the emphasis in treatment was placed on predominantly selective anticholinergic drugs - they reduce the pressure in the intestinal lumen - and drugs of the 5-aminosalicylic series.
As for the symptomatic form of management of diverticular disease, management is essentially no different from the management of patients with irritable bowel syndrome. And then there is a large list of various other inflammatory, allergic diseases of the intestines, both the small and large intestines. This group of diseases can never be discounted, and we have repeatedly encountered colitis, making a differential diagnosis of inflammatory bowel diseases, and there, for example, it turned out to be yersiniosis, and it, too, may not have a subacute, but a chronic relapsing course, and, of course, ischemic colitis , and, of course, associated with drugs, which we often forget about, and microscopic colitis. Despite the fact that, in general, I have not made many of these diagnoses in my life, it is certainly impossible to completely discount them. I demonstrate here some points, without focusing on particulars, that for each of the forms of colitis there are its own diagnostic features, and in many ways they are associated with features, including morphological histological conclusions. But as for, for example, some forms of microscopic colitis, here is a review from ten years ago, which suggests that distinguishing it from irritable bowel syndrome is not always really easy.
Well, and finally, new nosological forms appear, such as intestinal syndrome of drug addicts. Today, this form claims to be an independent nosological form, it occurs in people dependent on drugs, and this is associated with a change in the threshold of pain sensitivity, and, of course, we understand perfectly well that if it does not, then in the near future it will give us very There are many problems from the point of view of both managing these patients and making a diagnosis, among other things. Thus, in general, if we talk about approaches to the treatment of abdominal pain in intestinal diseases, of course, we should, in those cases in which we can, try to eliminate the cause. Although, alas, we cannot always do this. Next, of course, we must eliminate abdominal pain. It reduces the quality of life and makes it difficult to examine patients. There are a number of different approaches to this, and in general, if you arrange them in stages, then these are non-steroidal anti-inflammatory drugs, analgesics, antispasmodics, then more intense, let’s say, more complex opioid drugs and surgical interventions, these are, of course, antidepressants , and speaking here about antispasmodic therapy, we must understand: on the one hand, the combined prescription of drugs is indeed considered as one of the ways to relieve pain, but in this regard, hyoscine butyl bromide has its strengths, since it has a tropism for the enteric nervous system, and besides, here is a study that is good because for abdominal pain, the effect of paracetamol, the No. 1 drug in the world for pain relief, specifically for providing symptomatic assistance, showed almost completely similar results, and therefore we consider this drug as a drug for relief abdominal pain.
Moreover, taking into account that the frequency of side effects practically does not exceed the frequency of side effects when taking a placebo, and bearing in mind that pain of any origin is alleviated or stopped when using this drug, plus quickly, plus a small number of side effects, and that’s all , of course, we must take into account. Of course, we can use anticonvulsants, but it must be said that more research on this matter has been carried out specifically in chronic pancreatitis. In some cases, we can resort to laparoscopic treatment in situations where we suspect the presence of adhesions as the cause of pain, but we understand that these are not adhesions as such, but are either a reaction from the mesentery or changes in motility from the intestines. But if we look at the studies that are more or less rigorous today, then in no more than 60-70% of cases we have any lasting effect from this manipulation.
Thus, today we must clearly understand, and we know this with you, that abdominal pain is one of the most important symptoms of intestinal pathology, certainly not the only one, but very important. One of its causes, if we talk about statistics, the most common, is irritable bowel syndrome, and it can either be an independent nosological form, or it can hide an organic disease, or it can simultaneously coexist with an organic pathology. The mechanisms of pain are different, therefore they use different drugs, different combinations in pain relief, but it seems to me that we must clearly understand that pain relief in the 21st century is an independent clinical task, and we must do everything so that our patients, Living in this world, one should not experience this pain, including those suffering from serious illnesses. A large number of drugs are used, and various other approaches, including surgical, endoscopic, and one of the well-studied group of drugs that can relieve pain both in monotherapy and in complex therapy is a group of antispasmodics, and among them, of course, the important hyoscine butyl bromide takes its place due to its safety, fairly good study and thanks to those studies that have shown the safety of its use over long periods of time, up to 3 months. Thank you very much for your attention.