This is a blood test to determine its clotting ability. A hemostasiogram (coagulogram) evaluates the state of blood flow in all organs and systems.
A blood test for a hemostasiogram is done within one day. In laboratories, a blood test for a hemostasiogram (coagulogram) differs in parameters, measurement methods and, accordingly, information content and cost. The state of the coagulation system is a functional analysis that reflects changes in blood coagulation or the hemostatic system. The hemostasis system changes depending on external or internal factors. Factors influencing changes in the hemostatic system include age over 40 years, taking OCs and HRT, smoking, surgery, trauma, pregnancy, IVF protocol, etc. Accordingly, the results of the hemostasiogram analysis with the above factors will change.
It is important to monitor the function of blood clotting in pregnant women, patients with oncology and disorders of the cardiovascular system, when prescribing OCs and HRT, when planning surgery; also in patients with a family history of thrombosis, etc.
Hemostasiogram and coagulogram
One may mistakenly think that a hemostasiogram does some additional research and includes an analysis of the plasma system, but this is not the case. Laboratory actions for hemostasiogram and coagulogram are identical. But hemostasiogram and coagulogram differ in parameters, measurement methods and information content among laboratories.
Why do you need to do a hemostasiogram? The hemostasiogram reflects normal blood flow; in case of abnormalities, a shift in blood flow towards thickening or the risk of hemorrhage. Based on the results, you can understand what a person may suffer from - increased blood clot formation or blood loss. This procedure must be carried out before surgery to assess the risk of possible complications. Analysis during pregnancy will allow you to avoid complications throughout the entire period and how to better prepare for the birth process.
Extended hemostasiogram RUB 1,100.
Coagulogram 650 rub.
D-Dimer 1,100 rub.
All prices Make an appointment
Fibrinogen is increased: what does this mean?
Elevated levels of fibrinogen in the blood may mean activation of the blood clotting system, the possibility of excessive thrombus formation, or the occurrence of an acute inflammatory process in the body.
Thus, high fibrinogen protein is observed in severe, abnormal conditions that affect vital organs and the entire body as a whole. Among these diseases are:
- inflammatory-immune damage to connective tissue;
- death of the heart muscle as a result of acute lack of blood supply;
- kidney diseases;
- infectious diseases;
- endocrine diseases (diabetes mellitus);
- pneumonia;
- mild forms of inflammatory process in the liver;
- initial stage of thrombohemorrhagic syndrome;
- tuberculosis;
- oncological diseases.
Also, an increase in fibrinogen levels occurs during pregnancy, which is due to the natural physiology of the female body. Increased rates are observed with oral contraception and taking steroid female sex hormones.
How to prepare for donating blood for a hemostasiogram
Blood is donated on an empty stomach, from a vein. 12 hours before hemostasis, you must adhere to a diet excluding fatty and protein foods. The last meal (light snack) is possible 4 hours before blood sampling. It is prohibited to drink alcohol the day before the test. It is recommended to replace any drinks with water. This is done so that sugar does not affect the overall picture.
If you are taking medications that may affect the results of the data, this must be indicated when taking the test. This will be taken into account when deciphering the testimony.
It is not recommended for women to undergo the procedure during menstruation.
It is also better to refrain from playing sports in the previous day, to avoid stress and overexertion. Smokers are advised to give up cigarettes during this time.
The process of drawing blood also affects the accuracy of the result. When collecting from a vein, it is better to use a vacuum system. If this is not possible, then a syringe is used and the blood is allowed to flow on its own.
Indicators
It is extremely problematic to independently understand the results obtained without special education. Based on the results of the hemostasiogram, you must make an appointment with a hemostasiologist or hematologist.
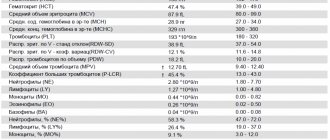
The form indicates the results obtained and the norms given in two columns. These are indicators of prothrombin, aPTT, prothrombin time, prothrombin index, fibrinogen, platelet function, thrombin time, RKMF, INR.
In a detailed analysis, an additional test for D-dimer, lupus anticoagulant, and antithrombin III is often prescribed.
Tests during pregnancy
Hemostasiogram
Pregnancy management
Hemostasiologist during pregnancy
Normal indicators
According to APTT data, the rate at which blood clots is assessed. Ideally, it should be from twenty-four to thirty-six seconds, laboratory referents differ - ADD. With a lack of vitamin K, this time will be longer. In this case, you should be wary of severe blood loss from cuts and deeper wounds. If the time, on the contrary, is less, this means that there is a risk of a blood clot. In this case, during pregnancy the baby will not receive enough nutrients.
The line with data on prothrombin contains the same results, but in percentage equivalent. So prothrombin should be from 78 to 95 to 105 percent.
Fibrinogen should normally be from two to four grams per liter; during pregnancy it can increase.
With normal levels, antithrombin III ranges from 71 to 115 percent,
Exact standards in laboratory abstracts. If deviations are greater or lesser, blood clots or bleeding may appear.
Thrombin time should be from eleven to eighteen seconds, and prothrombin time should be from fifteen to seventeen.
Platelet function is from 30 to 50%, a decrease in function indicates the risk of bleeding or the effectiveness of antiplatelet therapy, an increase indicates an increase in the aggregation function of the blood.
Hemostasiogram in pregnant women
Pregnant women need to especially carefully monitor blood clotting. This will avoid complications during the birth process, as well as throughout pregnancy.
During pregnancy, a hemostasiogram is taken once per trimester or more often if indicated.
The attending physician may prescribe additional tests if there is a threat of miscarriage, also to assess the effectiveness of anticoagulant therapy. It is also recommended to do a hemostasiogram in case of high blood pressure, edema, the presence of protein in a urine test, before surgery, or when prescribing OCs and HRT.
If test results are poor, consultation with a hemostasiologist is necessary.
Do not be alarmed if you suddenly discover that the coagulation rate is slightly higher than required. In pregnant women, this may also be a normal option. This may happen due to changing hormonal levels. For women in an interesting position, it is unstable and can change more than once. The result may be affected by the appearance of an additional circulation that connects the uterus and placenta and an increase in blood volume.
APTT
Activated partial thromboplastin time (aPTT)
APTT reflects the activity of the internal and general pathways of blood coagulation. The division of the coagulation cascade into internal, external and general pathways is conditional and does not fully reflect the true mechanism of hemostasis (see Theories and models of blood coagulation), but nevertheless, it still remains a useful resource for interpreting laboratory results. The intrinsic coagulation pathway is activated when circulating f.XII comes into contact with and binds to a negatively charged surface. This causes a change in its molecular configuration and, when interacting with high molecular weight kininogen and prekallikrein, it becomes an active enzyme - f.XIIa, capable of activating f.XI. In turn, f.XIa promotes the activation of f.IX with the formation of f.IXa. F.IX can also be activated by the F.VIIa/tissue factor complex via the extrinsic coagulation pathway. Then the f.IXa complex and its cofactor f.VIIIa cause the activation of f.X with the subsequent formation of thrombin. Abnormalities of the internal coagulation pathway are the cause of many coagulopathies, in particular hemophilia A and B.
Principle of the method
Incubation of plasma with the optimal amount of phospholipids in the presence of a contact activator (kaolin, silica gel, ellagic acid) activates plasma coagulation along the internal pathway. The addition of calcium ions to the system stops plasma citrate and leads to the formation of a fibrin clot. During the APTT measurement process, the time from the moment of adding calcium ions until the formation of a clot is recorded (see link to the instructions for the APTT test).
The determination of APTT is one of the most informative and common screening tests, which reflects changes in the activity of factors of the internal coagulation pathway: f.VIII, f.IX, f.XI, f.XII, prekallikrein (Fletcher factor) and high molecular weight kininogen (Fitzgerald factor) . The test is sensitive to deficiency of all coagulation factors (except f.VII and f.XIII), to heparin, to specific and nonspecific inhibitors of coagulation factors.
When determining APTT, it should be taken into account that:
- The time from blood sample collection to analysis should be no more than 1 hour, since the half-life of unfractionated heparin (UFH) is about 1.5 hours.
- The blood sample for analysis should be selected in such a way as to prevent platelet aggregation and activation with subsequent release of the heparin-inactivating factor PF4.
- If possible, it is recommended to establish the patient's baseline aPTT before initiating UFH therapy.
- APTT values may vary depending on techniques, equipment, reagent lots, and heparin used, so each laboratory should adopt its own therapeutic ranges and review them if any of these factors change.
In this cascade diagram of blood coagulation, the hemostasis factors reflected in the APTT test are highlighted in white:
Reference values:
Normal aPTT test values depend on the reagent used and should be established in each clinical diagnostic laboratory.
Interpretation of results
Diagnostic significance of the method. Currently, in addition to testing the activity of intrinsic coagulation factors (including for the diagnosis and monitoring of hemophilia A and B), the APTT method is also recommended for determining lupus anticoagulant and monitoring anticoagulant therapy with unfractionated heparin. When interpreting the results of the APTT test, it must be borne in mind that increased activity of one of the coagulation factors (for example, f.VIII) may mask the existing functional deficiency of other factors (for example, f.IX or f.XI). Therefore, in the presence of clinical symptoms of bleeding and normal aPTT values, further research is necessary to determine the causes of coagulopathy.
The shortening of clotting time obtained in the APTT test may indicate activation of the internal blood coagulation pathway, disseminated intravascular coagulation syndrome (at the stage of hypercoagulation - more often in combination with a shortening of PT, TV, high levels of fibrinogen, etc.); f.V resistance to activated protein C in patients with thrombophilia; violations of the APTT test at the preanalytical stage.
Prolongation of APTT may indicate a congenital or acquired deficiency of the internal pathway of blood coagulation (including in hemophilia A and B) with normal PT results; deficiency of factors of the common blood coagulation pathway with prolongation of PT; DIC syndrome (in the hypocoagulation stage - more often in combination with prolongation of PT, TV, reduced fibrinogen levels, etc.); deficiency of von Willebrand factor or f.VIII in von Willebrand disease; the presence of lupus anticoagulant, heparin, hirudin, fibrin/fibrinogen degradation products; liver dysfunction.
If the aPTT is prolonged, a test should be performed mixing the patient's plasma with normal donor plasma in a 1:1 ratio. If the aPTT remains prolonged, this means that the sample contains heparin or antiphospholipid antibodies (lupus anticoagulant) or clotting factor specific inhibitors. If the plasma mixing test shows normal results, then a deficiency of clotting factors VIII, IX, XI or XII is likely. Additional studies should be carried out to identify the true cause of the prolongation of the APTT test.
(See table Interpretation of basic test indicators)
What you need to know about APTT:
- An aPTT activator, such as kaolin, should be selected so that the aPTT is sensitive to moderate deficiency of factors VIII, IX and XI. To date, there is no activator that is fully sensitive to very small deficiencies of coagulation factors, so a normal APTT level does not exclude the presence of small deficiencies of factors VIII, IX and XI.
- The term “partial thromboplastin” refers to the phospholipid component of complete thromboplastin, devoid of apoproteins (tissue factor). The presence of a contact activator (kaolin, ellagic acid, silica gel, etc.) in the test system accelerates the clotting time and increases the accuracy and reproducibility of the APTT method by preventing uncontrolled contact activation of coagulation.
- If the optical density method is used to monitor clot formation, a falsely normal APTT may be recorded if the plasma is turbid (eg, hyperbilirubinemia, hyperlipidemia).
- Factor XIII deficiency does not prolong APTT or PT.
- APTT can be used to detect antiphospholipid antibodies (i.e., lupus anticoagulant), but in these cases reagents with low phospholipid concentrations sensitive to lupus anticoagulant should be used.
- When choosing phospholipids for APTT, it is important to choose the right reagent that is sensitive to deficiencies in coagulation factors.
- APTT may be made more or less sensitive to certain clotting factors by shortening the incubation time. It should be noted that the degree of APTT prolongation can give an idea of the nature of hemostasiological disorders. For example, if the aPTT is very prolonged, for example, >120 sec, then most likely the cause of the prolongation lies in a deficiency of contact factors, and not in a deficiency of factors VIII or IX (hemophilia A and B). Conversely, an aPTT of 70–80 seconds is associated with a diagnosis of severe hemophilia A or B rather than with contact phase factor deficiency.
- APTT is often used to monitor the effects of unfractionated heparin (UFH). However, APTT is also very sensitive to the level of f.VIII, which is an acute phase protein. If f.VIII levels rise, the aPTT may be misleadingly short and may not reliably reflect the degree of anticoagulation. In these cases, monitoring of UFH should be carried out by measuring anti-Xa activity.
- The APTT forms the basis for analyzing the levels of factors VIII, IX, XI and XI. Factors II, V and X can also be analyzed by APTT, although they are more often analyzed by PT.
- APTT is used to detect the presence of FVIII clotting inhibitors.
- In patients receiving very high doses of UFH, for example during cardiopulmonary bypass, the aPTT will not be recorded (as a clot will not form at all). In these cases, monitoring the degree of heparinization is usually carried out using activated clotting time (ACT).
- When receiving UFH, when aPTT is used to monitor the degree of heparinization, it is important to separate the plasma within 1 hour after drawing blood from the patient. This recommendation is due to the fact that 1 hour after blood collection, platelet factor 4 is released from platelets and neutralizes heparin. Neutralization of heparin may lead to insufficient prolongation of aPTT and underestimation of the degree of heparinization, which ultimately can lead to an overdose of prescribed heparin with possible hemorrhagic complications.
When preparing this section, data from the scientific website www.practical-hemostasis.com was used.
If fibrinogen is below normal
If your blood fibrinogen content is below the established norm, then its clotting occurs slowly, which will cause prolonged bleeding. This may be an acquired condition as a result of concomitant diseases or congenital.
The main reasons for the decrease in the amount of fibrinogen in the blood:
- thrombohemorrhagic syndrome - acute destruction of hemostasis, leading to the appearance of a huge number of microthrombi in the smallest vessels;
- severe hepatology;
- intoxication of the body during pregnancy;
- hypovitaminosis of group C and B12;
- genetic disorders;
- poisoning with toxic substances;
- use of medications that inhibit blood clotting and prevent blood clots;
- increase in the number of blood leukocytes;
- use of anabolic drugs, steroid sex hormones, valproic acid;
- taking Omega-3.
Low fibrinogen levels also occur:
- in people who have given up food of animal origin;
- when consuming antioxidants,
- with low blood alcohol levels.
If the volume of fibrinogen is less than 0.5–1 g/l, then there is a possibility of bleeding of the vessels of the internal organs.
Actions for low fibrinogen
As with increased fibrinogen, the first priority is to contact a qualified specialist who will promptly detect the causes of low protein and prescribe quality treatment. In addition, additional treatment can be carried out aimed at increasing the amount of fibrinogen, the essence of which is to take the following drugs:
- 6-aminohexanoic acid;
- transescam;
- ethamsylate;
- dicasol.
It is also necessary to change your diet and add more high-protein foods to it.
What to do if there is elevated fibrinogen?
The first thing to do if you have high levels of fibrinogen protein 0 is to immediately consult a doctor for further examination of the body. The specialist’s responsibility in this case is to prescribe high-quality therapy to eliminate the underlying disease, which will lead to a gradual independent decrease in protein levels to an acceptable level.
If there is an urgent need, fibrinogen levels can return to normal by taking medications that prevent blood clotting and the formation of blood clots. These include antiplatelet agents, anticoagulants, thrombolytics, fibrinolytics.
Filling your diet with fresh vegetables, seafood, red berries, dark chocolate or cocoa helps reduce the amount of protein in the blood. If all the specialist’s instructions are followed, increased fibrinogen does not pose a threat to the life and health of the patient.
Additional facts about fibrinogen
- The fibrinogen index, as a rule, is deciphered in conjunction with other tests, for example, PT and APTT.
- In the absence of a superficial reason for a decrease in the fibrinogen index and in the presence of some general clinical or medical history data, an immunological analysis of colorless protein is used to determine the basis of the disorders.
- To avoid incorrect results, blood testing for fibrinogen levels should not be performed on old specimens collected within 4 hours after administration of therapeutic doses of unfractionated heparin.
- High concentrations of unfractionated heparin may result in incorrect measurements of true fibrinogen levels.