Destruction of venous valves after thrombosis is the main cause of the development of circulatory failure and trophic ulcers in postthrombotic disease. Valvuloplasty (valve repair surgery) for incompetent deep vein valves is an effective method of improving venous outflow. Restoration of the valvular apparatus of the deep veins is possible in various ways, each of them has its own indications. This may involve replacing the affected venous segment with another section of the vein with preserved valves, or switching venous outflow through branches with preserved valves.
The best results are achieved through direct restoration of the valve apparatus using microsurgical valvuloplasty. Valvuloplasty allows for good compensation of venous outflow, which leads to a reduction in edema and healing of trophic ulcers. Deep vein valvuloplasty should be performed by experienced vascular surgeons who are proficient in microsurgical techniques and understand the pathology of venous outflow.
Preparation for surgery and anesthesia
Preparation for intervention on deep vein valves includes bowel cleansing and shaving the hair in the area of surgical access. The night before surgery, the patient is given a mild sedative. Immediately before entering the operating room, premedication is performed with a mild sleeping pill and analgesic.
In the operating room, a catheter is installed in the bladder and a subclavian intravenous catheter for infusion of solutions during surgery. For the purpose of anesthesia, we usually use an epidural catheter - an injection into the spine and prolonged administration of painkillers.
To monitor blood pressure and ECG indicators, a special monitor is connected to the patient.
Surgery
Direct surgical interventions
Surgery for varicose veins
The main method of treatment for varicose veins remains surgery. The purpose of the operation is to eliminate the symptoms of the disease, prevent the progression of varicose transformation of the saphenous veins, disrupt venous outflow by eliminating blood reflux, remove pathological venous capacity, and also eliminate the cosmetic defect caused by the disease. Surgical intervention in most cases includes several methods, performed simultaneously or in stages. The use of different combinations of methods should be justified by the characteristics and severity of pathological changes in the venous system. The indication for surgery is the presence of blood reflux in the superficial veins in patients with classes C2-C6. The presence of blood reflux along the trunks of the GSV, SVC and perforating veins in the absence of varicose transformation of the saphenous veins cannot be regarded as an indication for surgical treatment. In this situation, dynamic monitoring of the patient is necessary. The basis of surgery for VB of the veins of the lower extremities remains combined phlebectomy, which may include the following stages:
— high estial ligation and intersection of the GSV and/or SVC with all tributaries (crossectomy);
— removal of the trunks of the GSV and/or SSV;
— removal of varicose tributaries of the GSV and SSV;
— elimination of incompetent perforating veins.
Crossectomy and removal of the trunk of the great saphenous vein
The optimal approach for ligating the GSV is through the inguinal fold. The GSV must be ligated parietally to the femoral vein, all ostial tributaries must be ligated. There is no need for suturing of the oval window or subcutaneous tissue after crossectomy of the GSV. The GSV trunk is removed using probes of different designs. When determining the length of GSV stripping, it is necessary to take into account that in the vast majority of cases (80-90%), reflux along the GSV is recorded only from the mouth to the upper third of the leg, thus, in most patients, it is optimal to perform a “short” stripping - removal of the trunk from mouth to the level of the upper third of the leg. Removal of the GSV along its entire length (“total” stripping) is accompanied by a significantly higher incidence of damage to the saphenous nerves compared to removal of the GSV from the mouth to the upper third of the leg. However, the frequency of VD relapses does not differ significantly. Removal of the intact GSV trunk on the lower leg is not recommended. The remaining segment of the vein can later be used for reconstructive vascular operations. When choosing a safenectomy method, preference should be given to inversion techniques (including PIN stripping) or cryophlebectomy. Their advantage (less traumatic) compared to the classical Babcock technique is undeniable. When choosing the direction of vein removal, preference should be given to traction from top to bottom, i.e. retrograde, with the exception of cryophlebectomy, the technique of which involves antegrade removal of the vein.
Crossectomy and removal of the trunk of the small saphenous vein
Surgical interventions on the SVC should be performed with the patient in the prone position. The structure of the terminal section of the SVC is variable, so its crossectomy cannot be performed without preliminary ultrasound examination of the area of the saphenoplasty anastomosis. Before surgery, ultrasound scanning should be used to clarify the location of the anastomosis and the distribution of reflux. Ligation of the ostial part of the SVC is recommended to be performed from a transverse approach in the popliteal fossa. The vein should be removed only to the extent that reflux is determined to be present. In the lower third of the leg, reflux along the SVC is rare. Inversion methods should also be used for removal.
Removal of varicose tributaries of the saphenous veins
Removal of varicose tributaries of the GSV and SSV should be performed using the miniphlebectomy technique using appropriate instruments through skin punctures that do not require sutures. In some cases, by agreement with the patient, it is possible to leave some varicose veins for subsequent phleboscleroobliteration or laser therapy. Other previously discussed surgical methods (stitching of veins, removal of venous tributaries from separate incisions) are more traumatic and lead to worse results. In conditions of trophic changes in the skin and subcutaneous tissue, one should not strive for the most complete removal of nodes through skin approaches.
Ligation of incompetent perforating veins
An indication for the removal of perforating veins can only be pathological venous reflux in them, objectively recorded using ultrasound scanning. An objective assessment of the consistency of perforating veins is possible only with ultrasound scanning in a vertical position of the patient. In this regard, the current practice of studying perforators in a horizontal position of the patient should be considered incorrect. Even when identifying the incompetence of a perforating vein, the particularities of the course of the disease in a particular patient, the location of the perforating vein and its characteristics should be taken into account. It is advisable to carry out interventions on veins with a diameter of more than 3.5 mm with a reflux duration of more than 0.5 s, localized in the area of an open or healed trophic ulcer (classes C5-C6). In all other cases, the advisability of surgical intervention on perforating veins is questionable, since there is no evidence of the effectiveness of this approach. In addition, before deciding to intervene on perforating veins in patients with VV, surgeons should take into account that after eliminating vertical reflux along the trunks and tributaries of the GSV and SVC, reflux is not recorded in most of the previously incompetent perforating veins. Currently, the main method of eliminating reflux through perforating veins in the absence of trophic changes in the skin is their suprafascial ligation, for which miniphlebectomy instruments should be preferred. In conditions of trophic changes in the skin, incisions in the affected area should be avoided. Sclerotherapy or laser obliteration of incompetent perforating veins, performed under ultrasound guidance, are minimally invasive methods for eliminating horizontal reflux. Their use has no restrictions on the localization of perforating veins, does not require delaying treatment due to the presence of edema, induration, or skin atrophy, and is feasible even against the background of an open trophic ulcer. However, the effectiveness of these interventions in the medium and long term has not been sufficiently studied. Indications for the use of endoscopic subfascial dissection of perforating veins have now been significantly narrowed; it should be used only when minimally invasive methods are ineffective or in situations where their use is impossible. Open dissection of perforating veins (Linton-Felder method) for crossing incompetent perforating veins should not be used in VB surgery due to high morbidity and the availability of alternative minimally invasive techniques.
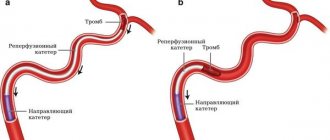
Correction of deep vein valves
Indications for correction of the valve apparatus of deep veins are currently under study. In a significant part of observations with VD, the complete elimination of vertical and horizontal reflux in the superficial veins in combination with compression treatment largely neutralizes the clinical significance of the incompetence of the deep vein valves; in many cases, ultrasound angioscanning shows the disappearance of reflux. That is why operations on the deep veins should not be performed simultaneously with interventions on the saphenous and perforating veins. Their implementation is possible only according to strict indications in patients with classes C5-C6 and reflux in the deep veins of III-IV degrees (to the level of the knee joint and below) according to the Kistner classification, as well as in case of ineffectiveness of all previously used methods of both surgical and conservative treatment Surgical methods for treating primary deep vein reflux can be divided into two groups. The first involves phlebotomy and includes internal valvuloplasty, the creation of new valves. The second group does not require phlebotomy and includes extravasal interventions, external valvuloplasty (transmural or transcommissural), angioscopically assisted extravasal valvuloplasty, and percutaneous installation of corrective devices. Intravasal correction of the valve apparatus is preferable. Operations to correct deep vein valves should be performed only in specialized centers with experience in such interventions.
Endovasal thermal obliteration (ablation)
Methods of thermal obliteration of veins are based on endovasal thermal damage to the venous wall, leading to its occlusion and transformation of the vein into a connective tissue cord, i.e. disappearance of the vein as a morphological and functioning structure. To do this, they use the energy of electromagnetic oscillations in the radio frequency range, laser radiation, and the energy of steam superheated under high pressure. The widespread introduction of thermal obliteration methods into clinical practice has demonstrated their effectiveness and safety, which has led to significant changes in the organization and structure of treatment for patients with VD. The use of thermoobliteration allows most patients to be treated on an outpatient basis under local anesthesia. The interventions are characterized by minimal trauma, rapid recovery of working capacity, good cosmetic results, and have a minimal negative impact on quality of life indicators. Modern endovasal techniques—laser and radiofrequency obliteration—can eliminate brainstem reflux, and therefore, in terms of their functional effect, can be called an alternative to crossectomy and stripping. These interventions are performed exclusively under ultrasound guidance from the moment of vein puncture until completion of the procedure. Their use in clinical practice is possible only with the availability of appropriate equipment and special training of the doctor. Currently, radiofrequency and laser obliteration are approved for use in Russia.
Indications and contraindications
Indications for endovasal thermal obliteration are similar to those for direct surgical methods. Diseases and pathological conditions that are contraindications for planned traditional phlebectomy should now be considered as contraindications for thermal obliteration. Various disorders of the hemostasis system, as well as the fact of their drug treatment, while not an absolute contraindication for performing the endovasal procedure, require a strict assessment of the degree of risk of developing possible complications. Early activation of the patient after thermoobliteration is an important measure to prevent venous thrombosis and other systemic complications. When treating venous trophic ulcers, thermoobliteration is not advisable during the period of acute purulent exudation. The minimal invasiveness of this intervention makes it possible to perform both stem thermoobliteration and obliteration of incompetent perforating veins in the ulcer area when acute inflammation subsides, without waiting for epithelization of the ulcer. The so-called anatomical or “technical” contraindications to laser obliteration are discussed - a tortuous course and large size of the vein, doubling of the trunk, or aplasia of trunk fragments, superficial subcutaneous location of the vein, its aneurysmal expansion, the presence of multiple ostial tributaries. Such structural features of the venous system should be diagnosed at the preoperative stage; they can significantly complicate the procedure, but as experience is gained, they cannot serve as an obstacle to performing thermoobliteration. Currently, special technologies and instruments have been developed to perform endovasal obliteration in difficult anatomical and technical conditions.
General principles of endovasal thermoobliteration
— Venous puncture, insertion and positioning of a laser light guide or radiofrequency catheter are carried out under echo control.
— The end of the light guide or catheter should not be placed above the proximal ostial inflow.
— Around the segment of the vein that will be subjected to thermal influence, a solution containing an anesthetic (tumescent anesthesia) is injected, which provides anesthesia, external compression of the vein with a decrease in its diameter to ensure close contact of the venous wall with the source of thermal influence.
— The success of the procedure depends on the application of an adequate dose of energy for laser obliteration, which is calculated in advance and usually depends on the diameter of the vein; with radiofrequency obliteration, the impact parameters are determined in advance.
— Obliteration of the distal segments of the GSV and SVC is undesirable due to the same reasons that limit the total stripping of these veins.
Features of laser obliteration
For effective obliteration on devices with radiation in the range of 810-1064 nm, it is necessary to use energy at the rate of 10 J for each mm of vein diameter, measured with the patient in an upright position. Thus, the linear energy density is usually 70-120 J per 1 cm of vein. To deliver such energy, a power of 10–15 W is used at a speed of fiber extraction of 1 cm in 7–10 s (1–2 mm/s). When using laser devices operating in the range of 1470-1560 nm, a radiation energy of 6-7 J is used for each mm of vein diameter. Thus, the linear energy density is usually 30-80 J per 1 cm of vein length. To deliver such energy, a power of 5–10 W is used at a fiber extraction speed of 1 cm in 7–10 s (1–2 mm/s). The exposure time is determined by the formula: t=LEED P, where t is the radiation time, LEED is the linear energy density, P is the radiation power. Before starting work, it is advisable to measure the radiation power at the working end of the optical fiber. The use of a laser light guide with radial emission has advantages over other types of light guides due to better energy distribution within the vein. The choice of radiation mode is determined by the physician's preference. Considering the need for long-term uniform traction of the optical fiber, it is possible to use special devices for automatic programmable traction of the optical fiber.
Features of radiofrequency obliteration
When performing radiofrequency obliteration, the following rules should be followed. The end of the catheter is placed in the ostial region distal to the proximal inflow and the effect is carried out for at least 2 energy cycles. On the thigh, to influence the trunk of the GSV, 1-2 cycles are carried out, at the level of the knee and on the lower leg - 1 cycle per segment. If the diameter of the main vein is more than 10 mm, it is permissible to use more than 1 cycle. To influence the MPV trunk, 1 cycle per segment is used.
Prevention of venous thromboembolic complications after thermoobliteration
The most severe complication of thermoobliteration is the development of deep vein thrombosis, caused by a continuing increase in thrombotic occlusion of the GSV or SVC proximal to the anastomosis. So-called thermally induced thrombosis occurs in less than 7-8% of cases and can occur even with strict obliteration technology, which is accompanied by thermal damage to the venous wall and the formation of occlusive thrombosis over a significant period. Although the issue of the need to prescribe anticoagulants after thermoobliteration does not have a clear solution in the literature, comparing the risk of treatment and possible complications, it should be considered more appropriate to prevent venous thromboembolic complications in patients with moderate and high risk using prophylactic dosages of low molecular weight heparins or fondaparinux for 4– 5 days
Surgical treatment of postthrombotic disease
Surgical interventions for PTB are an integral part of the complex treatment of this disease, but they cannot lead to complete clinical recovery. Currently, the lack of effect of complex conservative treatment, manifested in the development of a trophic ulcer, should be considered as an indication for surgical intervention for PTB. Surgical intervention can be aimed at accelerating the healing of a trophic ulcer (patients with class C6) or at preventing its relapse (patients with class C5). Persistent swelling or the beginning formation of trophic disorders in patients with occlusion or stenosis of the iliac veins may be a relative indication for surgical intervention. Surgical interventions for PTB are aimed at:
- to restore or create additional pathways for blood outflow from the lower extremities in the occlusive form of the disease;
- to eliminate or minimize the symptoms of venous stagnation of blood, normalize the function of the muscular-venous pump of the leg during recanalization of deep veins and secondary varicose syndrome.
There is no standard set of operations for the treatment of PTB. The point of application and method are selected strictly individually, based on the clinical picture, the results of examining patients using ultrasound angioscanning, and, if necessary, taking into account the data of radiopaque venography, radioisotope phlebography, CT and MR angiography. A certain sequence of surgical methods should be followed. Thus, the primary goal of surgical treatment for PTB is to restore the patency of the proximal venous segments (inferior vena cava, iliac veins, femoral veins, popliteal vein). For this purpose, surgical open deobstruction, endovascular angioplasty with stenting, and bypass surgery (Palma-Esperon procedure) are used.
Shunt interventions and restoration of deep vein patency
The Palma-Esperon operation (crossed femoral-femoral autovenous bypass) is indicated for unilateral occlusion of the iliac veins. A prerequisite is the absence of post-thrombotic changes in the veins of the contralateral side and the presence of an autovein of at least 6-7 mm. In some cases, to ensure the patency of the shunt, prevent its thrombosis, and prevent rethmbosis of the recanalized vein, it becomes necessary to create an artificial arteriovenous fistula (temporary or permanent, in the proximal or distal segments). Indications for its creation remain the subject of debate. The patency of the iliac veins in case of their occlusion or hemodynamically significant stenosis can be restored by endovascular angioplasty with stenting. The criteria for hemodynamically significant (critical) stenosis are not clearly defined, and the effectiveness of endovascular interventions in the long term has not been sufficiently studied. In the immediate period after stenting, it is possible to achieve restoration of the patency of the iliac veins in almost 100% of cases. In the future, the risk of rethrombosis and occlusion of the stented area remains, especially in patients with extensive occlusion and thrombophilia.
Interventions on the subcutaneous venous system
The saphenous veins in PTB perform a collateral function in many patients, and their removal can lead to a worsening of the disease. In this regard, in PTB, phlebectomy (as well as laser or radiofrequency obliteration) cannot be used as a routine procedure. The decision on the need and possibility of removing saphenous veins in one volume or another should be made on the basis of a thorough analysis of clinical and anamnestic information, and the results of instrumental diagnostic tests. The conditions for performing phlebectomy for PTB are the patency of the proximal parts of the deep venous bed (femoral and iliac veins), the presence of pronounced varicose syndrome, pathological reflux along the GSV, SSV, their tributaries, and confidence that the veins planned for removal have exhausted their bypass role. A comment. Against the background of changes in the deep veins that cannot be corrected, the possibility of a long-term effect from interventions on the saphenous veins during PTB surgical treatment is very doubtful. The appearance of new incompetent saphenous and perforating veins in the long term after surgery is not uncommon. The patient must be informed about this.
Interventions on perforating veins
Reflux along the perforating veins in patients with PTB develops in the first weeks after acute venous thrombosis, thereby providing collateral blood flow through the saphenous veins. Over time, when the compensatory function of the superficial veins is depleted, perforating reflux acquires a pathological role and may require elimination. The indication for intervention on perforating veins in patients with PTB is the presence of a healed or open trophic ulcer (class C5-C6). Currently, laser or radiofrequency obliteration should be considered the method of choice due to its minimal invasiveness. The use of endoscopic techniques to eliminate incompetent perforating veins in the area of the posterior and medial surface of the leg is possible in patients of classes C5-C6 when endovasal methods for obliterating perforating veins are unavailable. The Linton-type operation as a method of correcting the incompetence of the perforating veins of the leg should be excluded from the arsenal of PTB surgery.
Correction of incompetent valve apparatus of deep veins, transplantation and transposition of vein segments with normally functioning valves
Postthrombotic damage to the valve apparatus in most cases is not amenable to direct surgical correction. Various options for creating artificial valves have been proposed. The effect of these operations is often unpredictable, so the indications for them require careful discussion and usually arise:
— in the presence of classes C5-C6;
- if adequate conservative treatment is ineffective for 3-6 months;
— if previously performed interventions (bypass, saphenous and perforating veins) are ineffective.
The presence of an occlusive lesion in the proximal parts is an obstacle to operations to correct valvular insufficiency of the deep veins. If surgical valvuloplasty is ineffective, the possibility of transplantation or transposition of veins with functioning valves can be considered. For transplantation, veins of the upper limb are usually used, which are transplanted to the position of the femoral vein. Technical difficulties and limitations are caused by significant differences in vein diameters. Transplantation of vein segments containing valves shows good success in the immediate months after surgery. In the long term, dilatation of the transplanted segments with resumption of reflux is possible. The compensatory capabilities of a fragment with replaced valves in cases of extensive damage to the deep venous system are questionable. The purpose of venous transposition is to direct blood flow through a segment of the main vein with normally functioning valves. Thus, in the presence of an intact GSV, an anastomosis is formed between the GSV and the SSV after its resection. In other cases, given the rare lesion of the valve apparatus of the deep femoral vein, it is proposed to form an anastomosis between the resected SMV and the deep femoral vein distal to its healthy valve. Optimal conditions for performing these operations are rare. The small number of observations and the lack of analysis of long-term results do not allow us to evaluate the effectiveness of these operations and recommend them for practical use.
Surgical treatment of phlebodysplasia
Treatment of patients with venous forms of dysplasia should be carried out on the principles of an interdisciplinary approach, which involves both a thorough diagnosis based on predominantly non-invasive methods, and the integration of surgical and non-surgical treatment methods:
— compression therapy;
— surgical intervention;
— sclerotherapy (alcohol, liquid sclerosants, foam form);
— laser obliteration (endovasal, percutaneous) and thermal destruction;
— cryotherapy;
— electrocoagulation;
— microwave hyperthermia;
- drug therapy.
The extreme variability of the clinical picture in these forms of damage makes it necessary to individualize treatment tactics in each specific case.
Indications for surgical treatment of venous dysplasia are:
- bleeding;
- localization that poses a threat to life and an increased risk of complications;
- pain syndrome;
— CVI;
— functional limitations;
- pronounced cosmetic defect.
There are no effective methods for radical correction of hemodynamics in patients with phlebodysplasia. The main method of surgical treatment is excision of vein conglomerates in order to reduce local venous stagnation. In patients with obstructive deep vein disease, surgery is aimed at improving blood flow. Currently, positive results have been obtained in the treatment of a certain type of dysplasia using foam sclerotherapy, and local pathological formations of a capillary nature can be successfully treated using laser systems.
Surgeries for CVD can be performed in outpatient and/or inpatient departments by surgeons or angiosurgeons trained in phlebology. Operations on deep veins are the prerogative of vascular surgeons. Some types of interventions (reconstructive - valvuloplasty, bypass surgery, transposition, transplantation) should be performed only in specialized centers according to strict indications.
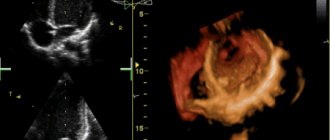
Direct valvuloplasty
It involves dissection of the venous wall above the valve and direct elimination of the anatomical and functional defect. The advantage of the method is the clear identification of the defect, ideal opportunities for restoration of the venous valve leaflets under visual control.
The disadvantages are the risks of damage to the valve apparatus during vein dissection, which can be eliminated by preliminary transverse venotomy followed by dissection of the vein above the valve under visual control. Direct valvuloplasty is a complex surgical procedure, which prevents its widespread use and must be performed under a microscope.
External valvuloplasty
It involves narrowing the vein around the valve in order to achieve closure of the valves. This operation has only two advantages: there is no need to cut the vein and it is easy to perform. It is significantly less effective than direct intervention.
The technique of such an operation can be different:
- Using an outer ring or coil on a vein (Vvedensky method)
- An enveloping suture of the vein above the valve without opening the lumen (extravasal valve correction)
- Wrapping the vein with bovine pericardium or a flap from a vascular prosthesis
The main disadvantage of this technique is the uncontrolled effect and the possibility of persistent narrowing of the vein.
Functions of the leg veins
The veins of the legs have a difficult task - without contractility, they must deliver a mass of blood from the most distant parts of the body to the heart.
This is what predetermined the structure of the network, divided into superficial and deep vessels, connected by a network of perforating ducts. Their walls consist of three layers:
- Intima is the inner layer of endothelium, separated from the middle layer by a thin membrane.
- The medial layer is the middle “layer” of the tube, represented by elastic fibers and a small proportion of muscle fibers. It is this layer that gives them strength and stretchability.
- The outer layer, consisting of connective tissue bordering the membrane that separates the blood tubes from the muscle tissue.
Despite the fact that in the lower extremities the drainage network is represented by tubes of different diameters (from 1.5 to 11 mm), the anatomy of the veins is almost the same. The only difference is the thickness of each layer and the number of valves. For example, the veins of the lower leg have more valves, but their diameter is 2 times smaller than that of the great saphenous vein.
In addition to blood pressure, superficial vessels experience significant stress due to external influences, so the thickness of their middle layer is much greater than that of deep-lying tubes. For example, the walls of the great saphenous vein are 1.3 times thicker and stronger than those of the deep vein.
The main functions of the VNK are:
- Ensuring uninterrupted outflow of blood, in which carbon dioxide and waste products of tissues located within their reach are dissolved.
- Delivery to tissues of hormones, organic compounds (enzymes, amino acids, proteins), vitamins and microelements coming from the intestines.
- Regulation of general blood pressure.
It is the variety of tasks assigned to the VNK that has led to close attention to the condition of the blood vessels. Any deviation in their functionality can cause irreparable harm to health.
Creation of a new venous valve
The principle is to construct a new valve using the patient's venous tissue. The technique for creating the valve depends on the situation with the venous wall. If it is thickened, then it can be stratified, then the resulting flap is fixed in the form of a sail directed with the convex side in the distal direction. You can make a bicuspid valve, which is the most physiological and effective. If there are fibrous cords in the lumen of the vein after thrombosis, then they can be used as leaflets of the valve being created. In the absence of such conditions, you can create a valve using your own venous wall, immersed in the lumen.
Transplantation (transplantation) of a normal venous segment
In order to restore the valve apparatus in veins that are not suitable for direct valvuloplasty, replacement of the venous segment with a section of the axillary or brachial vein with valves can be used. Using an incision in the shoulder, a section of a healthy vein with valves is removed and sutured into the femoral vein. Thus, a full-fledged valve apparatus is restored.
The disadvantage of this technology is the possibility of developing secondary expansion or, conversely, scarring of the transplanted segment, since the veins are somewhat different in structure.
Deep veins of the legs
The inferior vena cava system originates from the veins of the fingers, the venous arch of the sole and the dorsum of the foot.
- Varicose veins of the lower extremities: stages, causes, symptoms and treatment
From the venous arch of the dorsum of the foot, blood flows into the deep anterior tibial veins (DATIVs).
From the venous arch of the sole, the posterior tibial veins (PTV) and peroneal veins (MPV) are born.
The deep veins of the leg follow with the artery two, rarely four or more; merge before PKV.
PBBV lie in the anterior muscle bed of the leg; through the interosseous membrane they merge into the BBBV.
The internal and external marginal veins of the sole in the calcaneal canal will form two trunks of the BBBV.
ZBBV on n/3 of the leg immediately behind the muscular fascia, then between the flexors and the triceps muscle.
The MBV arises from the posterolateral calcaneus, superiorly between the MBV and the flexor pollicis longus.
On the third third of the leg, the deep veins merge, thus giving rise to the short trunk of the popliteal vein (PCV).
Drainage of the soleus and gastrocnemius muscles into the soleus and gastrocnemius (sural) veins.
- The structure of the human heart and its functions
Close to the joint space of the knee joint, the soleus and gastrocnemius veins merge into the PCV.
The SVC lies posterior to the RCA, from its junction with the thigh, called the superficial femoral vein (SFE).
The SMV from its confluence with the deep femoral vein (DFE) is called the common femoral vein (CFV).
The EIVs collect blood from the lower extremities and continue into the external iliac veins (ELVs).
At L5, the iliac vein and internal iliac vein (Iiliac vein) join to form the common iliac vein (CIV).
At L4, the IVCs drain into the inferior vena cava (IVC); The IVC runs to the right of the aorta and has no valves.
Possible complications after valvuloplasty
As after any major surgical operation, after valvuloplasty there are complications associated with the intervention itself:
- Bleeding
- Damage to the lymphatic ducts (lymphorrhea)
- Damage to cutaneous and deep nerves
- Postoperative wound suppuration
In our clinic, such complications are extremely rare.
Specific complications of this intervention are:
- Thrombosis of the reconstructed segment
- Ascending venous thrombosis
- Pulmonary thromboembolism
Fortunately, these complications are rare, their frequency does not exceed 1% of all operations performed.
Prognosis after valvuloplasty
The main goal of the intervention is to improve venous hemodynamics in the limb, which should ultimately lead to healing of trophic ulcers, reduction of edema and tissue hardening.
The result of treatment depends primarily on the correct determination of indications for surgery. Such a complex intervention as valvuloplasty should be performed only after all less complex methods of correcting venous outflow have been exhausted - eliminating reflux through the saphenous veins and perforators, the ineffectiveness of compression hosiery and venotonic drugs.
Team of Doctors
One of the methods for eliminating varicose veins of the lower extremities and symptoms of chronic venous insufficiency is sclerotherapy. It was first used in the last century.
This method is difficult to classify as surgical, since no incisions are made when using it. The technology of sclerotherapy is as follows. From a special solution, it is called a sclerosant, foam is made under sterile conditions. The resulting foam is injected into the lumen of a varicose vessel or node using a syringe through a thin needle under the control of an ultrasonic sensor. The foam pushes blood out of the lumen of the vein and, filling it with contents, sticks the walls together. Blood stops passing through the vein and over time the vessel undergoes involution and resolves. To remove spider veins and spider veins, laser removal through the skin is used. To do this, EMLA anesthetic cream is applied to the affected area of skin and a percutaneous laser vein removal procedure is performed. Surgical methods are aimed at excluding the affected main or tributary veins from the bloodstream. The Babcock operation is still used in many institutions. When an incision in the groin and above the ankle allows access to the great saphenous vein. A metal Babcock probe is inserted into its lumen, after which the vein is removed by pulling it out using a probe. Gentle modern methods of surgical treatment are being actively introduced into surgical practice. These are Endovasal Laser Ablation (EVLA) and miniphlebectomy. With EVLA, a laser probe is inserted into the lumen of the great saphenous vein and laser energy is applied. The inner walls of the vein then stick together and the vein turns into a cord, which dissolves over time.
Miniphlebectomy is performed when it is necessary to remove small sections of tributary veins. These veins are removed through small punctures using special phlebological instruments. There are no puncture marks left. Since there are several options for the structure of the venous system, and therefore the symptoms of varicose veins are so varied, after assessing the variant of the anatomical structure of the venous system, and the venous vessels are located at different depths and changes in them can be insignificant or occupy a fairly large surface of the skin, the phlebologist will choose the most appropriate a method of surgical treatment, taking into account the patient’s age, stage of development of the disease, symptoms of varicose veins and the severity of complications.
Observation after surgery
The patency of the restored venous segment must be monitored after surgery before discharge from the hospital using venous ultrasound.
Subsequently, examinations by a vascular surgeon with ultrasound should be performed at least once every 6 months. After a year, it is advisable to perform MRI venography.
The patient will be prescribed medications to reduce the likelihood of blood clots. Most often it will be warfarin (under the control of an INR analysis), sometimes we prescribe Prodaxa. It is unacceptable to stop taking these medications on your own without consulting your doctor.
Advantages of the Innovative Vascular Center
The Innovative Vascular Center is one of the few medical institutions in Russia where reconstructive operations on the deep venous system are successfully practiced. We have technologies and experience in microsurgical operations on the valves of the veins of the lower extremities in post-thrombotic disease, methods of endovascular correction of venous outflow (angioplasty and stenting of the iliac veins), and bypass operations on the deep veins.
The clinic has worked out in detail the diagnosis of venous outflow disorders and indications for reconstructive surgery on the deep veins.
Anatomy of the veins of the lower extremities
The veins of the lower extremities are divided into superficial and deep.
Superficial veins of the lower limb
The superficial venous system of the lower extremities begins from the venous plexuses of the toes, forming the venous network of the dorsum of the foot and the cutaneous dorsal arch of the foot. From it originate the medial and lateral marginal veins, which pass into the greater and lesser saphenous veins, respectively. The plantar venous network anastomoses with the deep veins of the fingers, metatarsals and the dorsal venous arch of the foot. Also, a large number of anastomoses are located in the area of the medial malleolus.
The great saphenous vein is the longest vein in the body, contains from 5 to 10 pairs of valves, and its normal diameter is 3-5 mm. It originates in front of the medial epicondyle and rises in the subcutaneous tissue behind the medial border of the tibia, bends around the medial femoral condyle behind and passes to the anteromedial surface of the thigh, parallel to the medial border of the sartorius muscle. In the area of the oval window, the great saphenous vein pierces the ethmoidal fascia and flows into the femoral vein. Sometimes the great saphenous vein on the thigh and leg can be represented by two or even three trunks. From 1 to 8 large tributaries flow into the proximal portion of the great saphenous vein, the most constant of which are: the external genital, superficial epigastric, posteromedial, anterolateral veins and the superficial vein surrounding the ilium. Typically, tributaries flow into the main trunk in the area of the fossa ovale or somewhat distally. In addition, muscle veins can flow into the great saphenous vein. The small saphenous vein begins behind the lateral malleolus, then it rises in the subcutaneous tissue, first along the lateral edge of the Achilles tendon, then along the middle of the back surface of the leg. Starting from the middle of the leg, the small saphenous vein is located between the layers of the fascia of the leg (N.I. Pirogov’s canal) accompanied by the medial cutaneous nerve of the calf. That is why varicose veins of the small saphenous vein are much less common than the large saphenous vein. In 25% of cases, the vein in the popliteal fossa pierces the fascia and flows into the popliteal vein. In other cases, the small saphenous vein can rise above the popliteal fossa and flow into the femoral, large saphenous vein, or into the deep vein of the thigh. Therefore, before the operation, the surgeon must know exactly where the small saphenous vein flows into the deep one in order to make a targeted incision directly above the anastomosis. The constant estuarine tributary of the small saphenous vein is the fenopopliteal vein (vein of Giacomini), which flows into the greater saphenous vein. Many cutaneous and saphenous veins flow into the small saphenous vein, most in the lower third of the leg. It is believed that the small saphenous vein drains blood from the lateral and posterior surface of the leg.
Deep veins of the lower limb
The deep veins begin as the plantar digital veins, which become the plantar metatarsal veins, which then drain into the deep plantar arch. From it, blood flows through the lateral and medial plantar veins into the posterior tibial veins. The deep veins of the dorsum of the foot begin with the dorsal metatarsal veins of the foot, which drain into the dorsal venous arch of the foot, from where blood flows into the anterior tibial veins. At the level of the upper third of the leg, the anterior and posterior tibial veins merge to form the popliteal vein, which is located lateral and somewhat posterior to the artery of the same name. In the area of the popliteal fossa, the small saphenous vein and the veins of the knee joint flow into the popliteal vein. Then it rises in the femoral-popliteal canal, now called the femoral vein. The femoral vein is divided into the superficial vein, located distal to the deep vein of the thigh, and the common vein, which is located proximal to it. The deep vein of the thigh usually flows into the femoral vein 6-8 cm below the inguinal fold. As you know, the femoral vein is located medial and posterior to the artery of the same name. Both vessels have a single fascial sheath, while doubling of the trunk of the femoral vein is sometimes observed. In addition, the medial and lateral veins surrounding the femur, as well as muscular branches, flow into the femoral vein. The branches of the femoral vein widely anastomose with each other, with the superficial, pelvic, and obturator veins. Above the inguinal ligament, this vessel receives the epigastric vein, the deep vein surrounding the ilium and passes into the external iliac vein, which merges with the internal iliac vein at the sacroiliac joint. This section of the vein contains valves, in rare cases, folds and even septa, which causes thrombosis to be frequently localized in this area. The external iliac vein does not have many tributaries and collects blood mainly from the lower limb. Numerous parietal and visceral tributaries flow into the internal iliac vein, carrying blood from the pelvic organs and pelvic walls. The paired common iliac vein begins after the confluence of the external and internal iliac veins. The right common iliac vein, somewhat shorter than the left, runs obliquely along the anterior surface of the 5th lumbar vertebra and has no tributaries. The left common iliac vein is slightly longer than the right and often receives the median sacral vein. The ascending lumbar veins flow into both common iliac veins. At the level of the intervertebral disc between the 4th and 5th lumbar vertebrae, the right and left common iliac veins merge to form the inferior vena cava. It is a large vessel without valves, 19-20 cm long and 0.2-0.4 cm in diameter. In the abdominal cavity, the inferior vena cava is located retroperitoneally, to the right of the aorta. The inferior vena cava has parietal and visceral branches, which supply blood from the lower extremities, lower torso, abdominal organs, and pelvis. Perforating (communicating) veins connect the deep veins with the superficial ones. Most of them have valves located suprafascially and thanks to which blood moves from the superficial veins to the deep ones. About 50% of the communicating veins of the foot do not have valves, so blood from the foot can flow from deep veins to superficial ones, and vice versa, depending on the functional load and physiological conditions of outflow. There are direct and indirect perforating veins. Direct ones directly connect the deep and superficial venous networks, indirect ones connect indirectly, that is, they first flow into the muscular vein, which then flows into the deep vein. The vast majority of perforating veins arise from tributaries rather than from the trunk of the great saphenous vein. In 90% of patients, there is incompetence of the perforating veins of the medial surface of the lower third of the leg. On the lower leg, incompetence of the perforating veins of Cockett, which connects the posterior branch of the great saphenous vein (vein of Leonardo) with the deep veins, is most often observed. In the middle and lower thirds of the thigh there are usually 2-4 most permanent perforating veins (Dodd, Gunter), directly connecting the trunk of the great saphenous vein with the femoral vein. With varicose transformation of the small saphenous vein, incompetent communicating veins of the middle, lower third of the leg and in the area of the lateral malleolus are most often observed. In the lateral form of varicose veins, the localization of perforating veins is very diverse.