Antianginal drugs are a group of drugs that are used to treat coronary heart disease - angina and myocardial infarction.
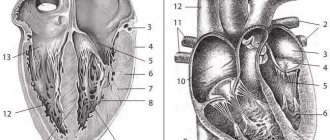
Coronary heart disease (CHD) is a pathological condition associated with oxygen starvation of the heart muscle (myocardium) due to insufficient blood supply to the vessels of the heart.
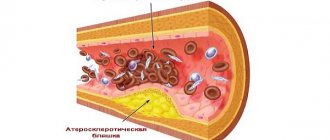
Chronic ischemic heart disease is manifested by angina pectoris. The causes of angina are usually narrowing of the lumen of the coronary (heart) vessels by atherosclerotic plaque (angina pectoris) or vasospasm (vasospastic angina).
Acute coronary heart disease is manifested by unstable angina and myocardial infarction. The cause of acute ischemic heart disease is partial or complete blockage of the lumen of blood vessels by a thrombus.
Unstable angina is considered a pre-infarction condition. Most often, it turns into an acute myocardial infarction, but if quickly recognized and treated, unstable angina can resolve quite safely.
The narrowing of the lumen of the coronary vessels leads to a decrease in the delivery of blood (and with blood, oxygen and nutrients) to the myocardium, which is manifested by oxygen starvation of the heart muscle, pain during physical activity or psycho-emotional stress.
Complete blockage of the lumen of the coronary vessels leads to a sharp lack of oxygen in the areas of the heart fed by these vessels and, in the absence of treatment, their death - necrosis.
Medicines used for angina are called antianginal drugs (from the old Latin name for angina: angina pectoris - angina pectoris).
Difficulties in risk stratification as a factor complicating the choice of therapy
It is well known that the intensity of preventive drug therapy for patients with coronary heart disease (CHD) should be directly determined by the level of cardiovascular risk.
Unfortunately, despite the many scales developed for this purpose, risk assessment for patients with coronary artery disease without a history of acute myocardial infarction (AMI) is today very difficult. In most cases, existing scales underestimate the risk level for patients in the high-risk group and overestimate it in the low-risk group [1]. The most significant practical difficulty here seems to be the impossibility of obtaining real information about the degree of stability of atherosclerotic plaques in the coronary vessels of a patient with coronary artery disease, which has primary prognostic value. Apparently, large atherosclerotic plaques that have a dense fibrous cap rupture less frequently, but at the same time cause pronounced clinical symptoms (in particular, anginal pain). At the same time, when they rupture and release a huge amount of procoagulant tissue factor into the vessel, the development of thrombotic occlusion of a large vessel is likely, the clinical equivalent of which is an extensive myocardial infarction with the formation of a Q wave [2].
Small plaques are less likely to lead to a significant decrease in coronary blood flow, which determines rarer and less intense attacks of anginal pain. But at the same time, small plaques can be much less stable; erosion or rupture of their thin fibrous cap can lead to the development of AMI, as a rule, without the formation of a Q wave (Fig. 1). As an illustrative example, we can cite the medical histories of patients with poorly compensated type 2 diabetes mellitus, who often have a history of several small focal infarctions and episodes of unstable angina.
According to new data, with unstable angina inside the coronary arteries, it is possible to form a kind of dynamic equilibrium, in which for a sufficiently long time small tears occur on the intimal surface or intimal erosions form, but the formation of a blood clot can be avoided due to the activation of the antithrombotic system. The use of methods for direct visualization of the structure of atheromas in vivo, such as optical coherence tomography/spectroscopy, makes it possible to identify such plaques [3].
Within the framework of this concept, it is easy to explain the results of the COURAGE study (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation), in which stenting of the coronary arteries did not lead to an improvement in prognosis, but significantly improved clinical symptoms. In all likelihood, despite the fact that anginal pain in these patients was associated with large, successfully stented plaques, the prognosis in this case was determined by small unstable plaques, the stenting of which, for obvious reasons, was not performed.
Today, assessment of the degree of stability of atherosclerotic plaques and interventions aimed at their stabilization, including through “hardening” the fibrous cap, are becoming a new paradigm in preventive cardiology. In fact, all traditional scales developed for patients with coronary artery disease solve the problem of risk assessment by analyzing factors that indirectly characterize the stability of atheromas.
Basics of treatment of coronary heart disease
Antianginal drugs are used both to relieve (eliminate) an attack of angina, and to prevent the occurrence of attacks systematically.
In addition to antianginal drugs, in the treatment of stable and vasospastic angina, drugs for the treatment of atherosclerosis (antiatherosclerotic) and the prevention of thrombus formation (antiplatelet agents) are used.
For the treatment of unstable angina and acute myocardial infarction, fibrinolytics (drugs that dissolve blood clots) and anticoagulants and antiplatelet agents (drugs that prevent recurrent thrombus formation) are used primarily not with antianginal drugs.
New non-invasive diagnostic options
One of the main directions in the development of modern cardiology is the search for minimally invasive methods for direct or indirect assessment of the stability of atherosclerotic plaques, which will make it possible to more accurately predict the risk of developing acute coronary syndrome (ACS). Their practical application seems especially important in the management of patients with average risk, for whom the choice of optimal treatment is often difficult. Today in the West, for this purpose, the most widely used integral indicator of the scale of coronary lesions is the calcium index, which is calculated when performing multislice computed tomography (MSCT) [4].
Another approach, which can also be implemented when performing MSCT, is the assessment of the distribution of contrast density in the coronary bed, which makes it possible to determine areas of the coronary arteries with low shear stress, where unstable atheromas can be expected to form [5].
Today, more and more experimental non-invasive techniques are appearing that are designed to specifically determine the state of atherosclerotic plaques.
These include the following diagnostic methods:
• MR imaging using intravascular coils and new contrast agents (eg, ultrasmall iron oxide particles that accumulate in macrophages);
• combined technologies MSCT/MRI (magnetic resonance imaging), PET/CT (positron emission tomography/computed tomography), CT/scintigraphy;
• molecular radiation diagnostics (for example, scintigraphy with 99Tc-annexin 5, 99Tc-IL-2, with labeled platelets and low-density lipoproteins).
Among the promising biochemical markers of instability of atherosclerotic plaques are lipoprotein-associated phospholipase A2, matrix metalloproteinase 9, soluble CD40 ligand, neopterin, as well as highly sensitive C-reactive protein, which is widely available for practical determination [6].
Basic principles of pharmacotherapy
IHD is a chronic “benign” disease, and therefore the main goals of its treatment are to reduce the number, duration and severity of attacks of anginal pain and improve the prognosis, which is determined by the risk of developing cardiovascular complications such as AMI, life-threatening arrhythmias and chronic heart failure (CHF).
Currently, the effect on the prognosis of patients with coronary artery disease has been proven only for statins, angiotensin-converting enzyme inhibitors - ACE inhibitors (ramipril and perindopril), antiplatelet drugs and β-blockers (after AMI). In this review, we will focus on therapies that can primarily alleviate the condition of patients with exertional angina.
Antianginal and anti-ischemic therapy of chronic ischemic heart disease
Beta-blockers (BABs) are rightfully considered the cornerstone of the treatment of coronary artery disease. In the absence of absolute contraindications, selective β1-blockers should be prescribed without fail to all patients with a history of AMI due to their ability to increase the survival of such patients and reduce the incidence of recurrent AMI.
Cardioselective beta blockers serve as the main tool for the treatment of angina pectoris, and antianginal drugs of other groups should be used only after the potential of the beta blocker is maximally used [7].
It is extremely important to achieve target heart rate values (HR, 55–60 beats per minute), without which antianginal therapy cannot be considered optimal. If, while using beta blockers, a patient with stable angina continues to experience attacks of anginal pain, an attempt should be made to reduce the heart rate to 50 beats per minute, unless atrioventricular (AV) block develops against this background [7]. In this case, heart rate should be measured in the morning before taking the next dose of the drug.
Today, one can often find patients taking large doses of nitrates due to severe anginal pain, but not receiving optimal beta blocker therapy.
In most cases this is due to the following factors:
• unjustified fears regarding the development of side effects, which are rare (primarily various blockades and broncho-obstructive syndrome);
• the desire to prescribe a low dose of beta blocker as part of combination antianginal therapy (the real effectiveness of which may be significantly inferior to full-dose beta blocker therapy);
• difficulties in comparing dosages of different beta blockers (today doctors often use bisoprolol at a dose of 10 mg, but avoid using metoprolol at doses above 150 mg/day, and therefore patients receiving metoprolol often have a higher heart rate);
• difficulties associated with titrating beta blockers (this especially applies to the lipophilic carvedilol, which has a difficult to predict relationship between dosage and effectiveness);
In case of intolerance to beta blockers, they can be replaced with calcium channel blockers (CCBs). It should be especially noted that none of the controlled studies of CCBs showed their effect on the survival of patients with angina pectoris.
In patients with bronchial asthma, extended-release verapamil, which has a pulse-sparing effect, can be considered the drug of choice. It should be remembered that, compared with beta blockers, its use in elderly patients is associated with a higher risk of developing AV block of II–III degrees. If a significant slowdown in AV conduction occurs during the use of verapamil, Holter ECG monitoring is justified, including to exclude second-degree AV block at night.
Dihydroperidine CCBs have a weaker antianginal effect than non-dihydroperidine CCBs, but can be successfully used by patients with conduction disorders. In a number of patients, these drugs can lead to the development of subendocardial ischemia [7].
If there are contraindications to the administration of beta blockers, primarily in the presence of AV conduction blockade of the 1st degree or bronchial asthma, the If-channel inhibitor ivabradine can be used as a pulse-lowering drug. The antianginal effect of ivabradine is realized only due to a decrease in heart rate, which is why it is “in strength” inferior to beta blockers, which have a multifaceted mechanism of anti-ischemic and cardioprotective actions. It should be noted that in a large clinical trial that included more than 10 thousand patients with coronary artery disease and heart failure, ivabradine did not show an effect on cardiovascular mortality and the frequency of hospitalizations caused by AMI and heart failure [8].
Classification of antianginal drugs
Depending on the mechanism of action, antianginal drugs are classified into:
- drugs that increase oxygen delivery to the heart: menthol, validol (menthol in isovaleric acid menthyl ester), dipyridamole;
- drugs that reduce the heart's need for oxygen: β-blockers (propranolol, metoprolol, atenolol, betaxolol, bisoprolol, nebivolol, carvedilol);
- bradycardic drugs (ivabradine);
- organic nitrates and nitrate-like agents - sydnonimines (nitroglycerin, isosorbide mononitrate, isosorbide dinitrate, pentaerythrityl tetranitrate, molsidomine);
Combined antianginal therapy
The presence of complaints of anginal pain in patients with coronary artery disease receiving first-line therapy dictates the need to add additional anti-ischemic drugs. The algorithm for their application is presented in Fig. 2.
Before initiating combination antianginal therapy, it is necessary to ensure that the target heart rate is achieved with the use of beta blockers. In case of intolerance to beta blockers, not associated with the presence of blockades, an attempt should be made to prescribe verapamil or diltiazem in monotherapy.
Adding ivabradine to a beta blocker is justified only if the heart rate with the maximum dose of beta blocker (20 mg bispoprolol or 400 mg metoprolol) exceeds 70 beats per minute or if titration of the beta blocker dose is impossible (for example, due to chronic obstructive pulmonary disease or clinically significant vascular atherosclerosis lower extremities). The use of ivabradine together with small doses of beta blockers to reduce heart rate in patients who tolerate beta blockers well, due to the lack of evidence, should be considered irrational.
If, against the background of the target heart rate, the patient continues to be bothered by anginal pain, it is optimal to prescribe a CCB as a “second” drug [11]. In some cases, long-acting nitrates/NO donors or nicorandil can also be used.
Complaints about the presence of anginal pain in patients with coronary artery disease receiving therapy with two antianginal drugs serve as a direct indication for coronary angiography with subsequent decision on the tactics of revascularization. Currently, daily combination therapy with three or more antianginal drugs can be considered justified only for those patients in whom revascularization is not possible for any reason.
results
Study A
28 patients completed the study completely. Two patients dropped out of the study due to failure to appear for examination. The crossover design of the study ensured that the groups were completely identical in age (mean 47 [41–54] years), gender (12 men and 16 women), duration of hypertension (2 [0–6] years) and body mass index (29 [25–6] years). 32] kg/m2). In table Figure 1 shows the initial characteristics of hemodynamics in the groups according to office, “home” and monitor blood pressure measurements.
. Initial characteristics of central hemodynamics (Me [AI]).
The selected groups were comparable in terms of initial hemodynamic parameters and daily blood pressure profile. After two weeks of therapy, the dose of bisoprolol was increased to 10 mg in 14 patients in the Concor group (50.0%) and 15 in the Bidopa group (53.6%). The proportions of patients with an increased dose of the drug did not differ between groups (рχ2 = 0.79). Over the next four weeks of therapy, in 2 (7.1%) patients taking the original bisoprolol, the dose of the latter was reduced to 5 mg due to the development of bradycardia <55 beats/min. By the end of the study, the average dose of Concor was 7.0 ± 2.5 mg, Bidopa – 7.8 ± 2.5 mg (p = 0.25).
The dynamics of blood pressure and heart rate according to office measurements while taking the study drugs are presented in Table. 2.
. Dynamics of office blood pressure and heart rate during treatment with bisoprolol (Me [II]).
Taking both drugs for 2 and 6 weeks resulted in a statistically significant decrease in clinical blood pressure and heart rate compared to baseline values. The average heart rate by the 6th week of the study in the original drug group was lower than in the generic group.
The dynamics of blood pressure and heart rate according to self-monitoring while taking the study drugs are presented in Table. 3.
. Dynamics of home blood pressure and heart rate during treatment with bisoprolol (Me [II]).
Blood pressure and heart rate decreased significantly in both groups starting from the 2nd week of taking the drugs. In the Concor group, a further decrease in DBP was noted in the interval of 2–6 weeks. The average DBP level by the 2nd week of the study was lower in the Bidop group (at the border of significance).
ABPM was performed twice during the first stage of treatment. Data from 12 patients in the first group and 13 in the second group were suitable for analysis. In table Figure 4 shows the dynamics of ABPM parameters while taking bisoprolol drugs.
. Dynamics of ABPM parameters during treatment with bisoprolol (Me [II]).
The data presented in table. 4 indicate a significant decrease in average daily blood pressure and heart rate during treatment with both drugs. Taking generic bisoprolol, in contrast to the original one, also led to a decrease in the time index of hypertension and an increase in the time index of hypotension according to DBP. In Fig. 1–3 display the degree of hypotensive and pulse-lowering effects of Concor and Bidop. With office and monitor measurements of blood pressure and heart rate, the drugs turned out to be equally effective in both hypotensive and pulse-suppressing effects. During home blood pressure monitoring, the degree of reduction in SBP by the 6th week and heart rate by the 2nd week of treatment was greater in the Bidopa group.
Target BP < 140/90 mm Hg. Art. at the end of the 6-week course of treatment, 20 patients of the first group (71.4%) and 18 patients of the second group (64.3%; pχ2 = 0.57) achieved it. Two patients in the Concor group (7.1%) received a dose of 10 mg/day. bradycardia <55 beats/min was recorded, which was not accompanied by clinical symptoms, but required a reduction in the dose of the drug. No other adverse reactions associated with the study drugs were recorded.
Study B
All included patients (18 patients) completed the study. When randomizing the sequence of drug prescriptions for 10 patients, the first drug was Concor, the second was Bidop, for 8, on the contrary, the first drug was Bidop, the second was Concor. For 11 patients, the dose of bisoprolol was 10 mg, for 6 – 20 and for 1 – 5 mg (13.5 ± 2.8 mg). Analysis of the number of angina attacks in the control period and while taking Concor and Bidopa showed a significant reduction in attacks during the use of both drugs. The total number of attacks in the control period was 3.8 ± 1.1, while taking Concor - 1.2 ± 0.3 (p < 0.01), while taking Bidopa - 1.0 ± 0.2 (p < 0.01), the number of attacks did not differ between each drug (p = 0.21).
While taking Concor and Bidop, SBP, DBP and heart rate at rest significantly decreased compared to these indicators in the control period. There were no significant differences in these indicators between the groups (p > 0.05; Table 5).
. Levels of blood pressure and heart rate at rest in the control period and during treatment with bisoprolol (Me [II]).
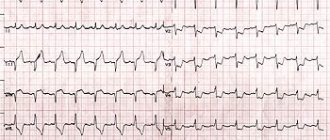
During the initial stress test, ischemic depression of the ST segment was registered in all patients. When conducting a stress test while taking Concor and Bidop, ischemic depression of the ST segment was also recorded for all patients examined. At the same time, a significant (p < 0.001) decrease in the degree of depression of the ST segment was noted at the same minute of load compared to the test conducted during the control period. While taking Concor, the degree of ST segment depression decreased on average by 29%, while taking Bidopa - by 34%; the difference between these indicators is not significant (p > 0.05). An increase in the duration of exercise while taking Concor and Bidopa by more than 2 minutes was observed in all patients. When using Bidop, the increase in load was 186 ± 12 seconds, while taking Concor – 179 ± 11 seconds (p > 0.05).
Despite the increase in the duration of physical activity and the work performed, the pulse pressure index at the height of the load did not change. In the control period, it was 18,612 ± 87 units, while taking Concor – 18,423 ± 98, while taking Bidopa – 18,512 ± 85 units (p > 0.05).
Management of patients with refractory angina when revascularization is impossible
The concept of refractory angina includes the following three factors:
1. Myocardial ischemia;
2. Anginal pain;
3. Impossibility of revascularization [12].
The following categories of patients are usually considered “inappropriate” candidates for revascularization [12]:
• patients with vasospastic angina;
• patients with suspected microvascular dysfunction (with objective signs of myocardial ischemia in the absence of significant coronary artery stenosis or with normally functioning bypass grafts);
• patients with a small volume of ischemic myocardium, when it is impossible to perform angioplasty (for example, with a hemodynamically significant symptom-related distal single-vessel lesion), stratified into the low-risk group;
• patients with diffuse, “thread-like” coronary atherosclerosis (typically damage to two or more coronary arteries, involving the distal bed with arteries < 1 mm in diameter);
• persons with a very high perioperative risk (due to severe concomitant diseases, this group often includes elderly people with multi-vessel disease).
It must be emphasized that the conclusion about the impossibility of revascularization should be made by a multidisciplinary team and this status can be revised taking into account changes in the patient’s condition and the possibility of attracting an experienced surgical team capable of operating on high-risk patients.
Next, we will consider drugs that can be used in “maximized” antianginal therapy regimens for such patients.
One of the highly effective antianginal drugs is nicorandil, an activator of ATP-dependent potassium channels in the plasma and mitochondrial membranes with nitrate-like properties. Usually, nicorandil is used in cases of intolerance to beta blockers and cCBs, but it can also be used as part of combination therapy. In a double-blind study involving patients with stable angina, nicorandil was shown to lead to a significant increase in exercise capacity, time to onset of anginal pain and ST depression ≥ 1 mm [13]. In the IONA randomized clinical trial (RCT), which included more than 5000 patients with chronic ischemic heart disease, nicorandil, prescribed at a dose of 20 mg twice daily, demonstrated superiority over placebo in terms of its effect on the incidence of hospitalization, which was regarded as a reduction in the risk of developing unstable angina. In approximately a third of cases, a headache may occur in the first days after taking nicorandil [13], and there is also a risk of developing tolerance to its action.
Another promising drug is ranolazine, which partially inhibits fatty acid oxidation and blocks late sodium channels (operating in diastole). Ranolazine is able to neutralize ischemia-induced sodium and calcium “overload” of cardiomyocytes, improving perfusion and diastolic function of the myocardium. In addition, it has an antiarrhythmic effect and is able to reduce the level of glycosylated hemoglobin in patients with a combination of coronary artery disease and diabetes.
Several randomized, double-blind studies (MARISA, ERICA, CARISA) have shown that ranolazine reduces the frequency of angina episodes, nitrate intake and increases exercise tolerance without clinically significant effects on heart rate and blood pressure [14]. However, in the MERLIN TIMI 36 (Metabolic Efficiency With Ranolazine for Less Ischemia in Non-ST Elevation Acute Coronary Syndromes) study, in which patients with ACS were observed for a year, ranolazine did not show an effect on the risk of AMI and cardiovascular mortality. When treating angina in people with microvascular dysfunction, it is also possible to use drugs with analgesic properties, such as the phosphodiesterase inhibitor aminophylline, the antidepressant imipramine. Methods of psychotherapy and cardiac rehabilitation can also be used [15].
Non-drug methods that can alleviate the condition of some patients with refractory angina include enhanced external counterpulsation, shock wave therapy and electrical stimulation of the spinal cord [16]. An invasive procedure such as transmyocardial laser revascularization, according to a meta-analysis of 7 studies (n = 1137), cannot be recognized as an effective treatment for refractory angina [17].
Currently, the effectiveness of such experimental methods for treating resistant angina is being clarified, such as cell therapy and the use of growth factors that activate angiogenesis, including granulocyte-macrophage colony-stimulating factor, which can “mobilize” bone marrow stem cells to participate in coronary angiogenesis.
Modern approaches to antianginal therapy for coronary heart disease: focus on sydnonimines
Hippocrates pointed out that “pain in the region of the heart, which appears with a certain frequency in old people, is an omen of sudden death.” Bartoletti (1576–1630), Harvey (1527–1658), Morgagni (1684–1771) described cases of severe acute pain in the left half of the chest in elderly and old people, accompanied by anxiety, fear, suffocation, and fainting during an attack. The first description of classical angina belongs to W. Heberden (1772), who first used the term “angina pectoris” to refer to it in his report to the Royal Society of London and described in detail and accurately the clinical picture of angina pectoris (“Heberden’s angina pectoris”). Parry (1799) was the first to point out the connection between angina pectoris and changes in the structure of the heart and damage to the coronary arteries. He was the first to suggest that anginal (angina) pain occurs due to a decrease in the blood supply to the heart. In 1909, at the first congress of Russian therapists, a classic description of the clinical picture of myocardial infarction was given in the fundamental work of V.P. Obraztsova and N.D. Strazhesko “On the symptomatology and diagnosis of coronary artery thrombosis.” (Nikolai Dmitrievich Strazhesko - later a prominent Soviet therapist, organizer of science, academician of the USSR Academy of Sciences and the Ukrainian Academy of Sciences, Hero of Socialist Labor). Currently, cardiovascular diseases firmly hold 1st place among all causes of mortality in economically developed countries, being one of the most common pathologies among chronic non-communicable diseases. Despite this, starting from the second half of the 20th century. Countries in Western Europe and North America have seen a steady decline in mortality from cardiovascular diseases. This trend has been observed in recent years in Eastern European countries [1,2]. In the Russian Federation, more than 1 million people die from cardiovascular diseases, i.e. approximately 700 people per 100 thousand population. IHD often develops in able-bodied, creatively active individuals, significantly limiting their social and work activity, exacerbating socio-economic problems in society [1–4]. The basis for reducing morbidity and mortality in coronary artery disease is the fight against controllable risk factors for the disease. Thus, even in the classic Framingham study, launched in the USA in 1949, it was shown that the risk of developing coronary artery disease is associated with high blood pressure, high cholesterol levels, smoking, impaired glucose tolerance and left ventricular hypertrophy (results of the Framingham study are available on the Internet – website of the US National Heart Institute - www.nhlbi.nih.gov/about/framingham, 1998). 1. Non-modifiable (unchangeable) risk factors (RF) for IHD [5–7]: • age over 50–60 years; • gender (male); • burdened heredity. 2. Modifiable (changeable) risk factors [5–7]: • dyslipidemia (increased blood levels of cholesterol, triglycerides and atherogenic lipoproteins and/or decreased levels of anti-atherogenic HDL); • arterial hypertension (AH); • smoking; • obesity; • carbohydrate metabolism disorders (hyperglycemia, diabetes mellitus); • physical inactivity; • chronic stress; • poor nutrition; • hyperhomocysteinemia, etc. The combination of several risk factors in one person significantly increases the risk of IHD and, as a rule, aggravates its course. Pharmacotherapy for IHD involves mandatory preventive measures aimed at eliminating modifiable risk factors for IHD. An important role in this regard is given to the correction of hypertension, normalization of glucose levels in patients with diabetes mellitus, smoking cessation, comprehensive diet modification, control of excess weight, and physical training [1–3]. Treatment of angina pectoris involves the use of various groups of drugs that affect certain parts of the pathogenesis of coronary artery disease [3]. The main pathogenetic factor of IHD is impaired blood flow in the coronary arteries, leading to an imbalance between perfusion and metabolic needs of the myocardium. Myocardial oxygen demand is determined by the tension of the myocardial wall, heart rate and myocardial contractility and depends on metabolic processes, including those associated with transmembrane currents of calcium ions, on the volume of the ventricles of the heart and on the value of systolic blood pressure. Contractility depends on the nature of organic damage to the heart. The supply of oxygen to the heart muscle is directly related to the state of coronary blood flow, and the value of the latter depends on coronary resistance, and on the activity of the sympathetic nervous system, and on the level of perfusion pressure, and on the hemorheological properties of blood, in particular on the level of platelet aggregation [3,8– eleven]. The main goals of treatment for patients with coronary artery disease are: improving the patient’s quality of life by reducing the frequency of angina attacks and other symptoms relevant to the patient; prevention of acute myocardial infarction; improved survival. Drugs used for the treatment of coronary artery disease: • Antianginal agents: – nitric oxide donors – nitrates (nitroglycerin, isosorbide dinitrate, isosorbide-5-mononitrate); – sydnonimines (molsidomine (Sidnopharm)); – β-blockers (atenolol, bisoprolol, propranolol, etc.); – calcium antagonists (verapamil, diltiazem, etc.). • Antiatherosclerotic (hypolipidemic) agents. • Antiplatelet drugs (acetylsalicylic acid, clopidogrel). • Metabolic agents (trimetazidine). The goal of antianginal therapy for coronary artery disease is to reduce the number of angina attacks during the day until they are completely eliminated. This allows the patient to be quite active in everyday life and not feel discomfort in life due to many restrictions that preceded treatment. Such changes in the physical and psychological status of the patient objectively lead to a significant improvement in the quality of his life. In addition, in many cases, symptomatic therapy allows the patient to continue professional activity if it does not involve heavy physical labor. Antianginal treatment is considered successful in the case of complete or almost complete elimination of angina attacks and the patient’s return to normal activity (angina pectoris no more than functional class I - FC, when painful attacks occur only under significant loads) and with minimal side effects of therapy [13–15]. Nitrates. Nitrate preparations for “angina pectoris” have been used for about a century and a half. Nitroglycerin was discovered by Ascanio Sobrero in 1847 in Turin. Sobrero was also the first to draw attention to the severe headache caused by testing small amounts of nitroglycerin on the tongue. In 1849, K. Hering, studying the pharmacological effect of nitroglycerin on volunteers, confirmed that its use quite naturally causes headaches. In 1851, William Murrell first used nitroglycerin for angina pectoris in 1876, although at that time nitroglycerin was listed in the British Pharmacopoeia only as a drug for high blood pressure. Merrell, a medical practitioner who worked in two London hospitals at the same time, experimentally determined the optimal dosage from the balance of effectiveness and safety: a 1% alcohol solution of nitroglycerin, 3 drops with half an ounce of water, three times a day. In this form, the drug acted much longer than amyl nitrite, and more gently. Merrell's publication, summing up the results of several years of research, first on himself and then on patients with angina, entered the golden fund of medicine. A year later, pharmacist William Martindale developed a solid form of the drug: 1/100 grain of nitroglycerin in chocolate - which, in addition to being easier to use, had better digestibility. In 1882, the famous company Parke, Davis & Co. in the USA. began to produce nitroglycerin in five different dosages. The nitroglycerin industry boomed in 1900, with workers exposed to significant amounts of organic nitrate fumes. The results of exposure manifested themselves in the form of addiction to nitrates (as evidenced by the symptoms of “Monday disease”, disappearing by the end of the week) and withdrawal syndrome (Sunday heart attacks, “Sunday Heart Attacks”). The mechanism of the antianginal action of nitrates is to reduce the myocardial oxygen demand, which is caused by a decrease in ventricular wall tension, systolic blood pressure and ventricular volume. In addition, the antianginal effect is realized by improving the supply of oxygen to the myocardium: by increasing coronary blood flow, reducing coronary resistance, reducing spasm of the coronary arteries and increasing collateral blood flow. They also have platelet adhesion and aggregation inhibitory properties and, apparently, antithrombotic properties. The antiaggregation effects of nitrates can be considered as an important addition to their anti-ischemic action [1,2,12,14,15]. Nitrates easily penetrate all mucous membranes, as well as through the skin, so they are available in numerous dosage forms. These dosage forms can be divided into the following (Table 1) [2]: 1. Absorbed through the oral mucosa. These include: a) Classic nitroglycerin tablets for administration under the tongue, the so-called buccal (i.e., intended for application to the mucous membrane of the cheek or gum) dosage forms of nitroglycerin and isosorbitol dinitrate. b) Aerosols of nitroglycerin and isosorbitol dinitrate, which can have the same rapid effect as sublingual nitroglycerin tablets (the effect begins within 60–90 s), but are much more convenient to use. 2. For oral administration. These are various tablets and capsules of isosorbitol dinitrate, isosorbitol mononitrate and nitroglycerin. Tablets can be regular or special, made in such a way as to prolong the effect of the drug. 3. For cutaneous use. Nitroglycerin ointments and special nitroglycerin stickers (plasters) for application to the skin. Such patches are designed to last for 24 hours. 4. For intravenous administration. Ampoules with a solution of nitroglycerin and isosorbitol dinitrate. β-blockers. Drugs of this group have been used in the treatment of patients with coronary artery disease for more than forty years. β-blockers are the first choice drugs for the treatment of angina pectoris, especially in patients who have had a myocardial infarction, as they have a rapid antianginal effect and also lead to a reduction in mortality and the incidence of recurrent infarction with long-term use [1–3,14–15] . β-blockers cause an antianginal effect by reducing the myocardial oxygen demand (due to a decrease in heart rate - heart rate, lowering blood pressure and myocardial contractility), increasing the delivery of oxygen to the myocardium (due to increased collateral blood flow, its redistribution in favor of the ischemic layers of the myocardium - subendocardium), antiarrhythmic and antiaggregation effects, reducing calcium accumulation in ischemic cardiomyocytes. Calcium channel blockers (calcium antagonists). The main point of application of drugs of this group at the cellular level are slow calcium channels, through which calcium ions pass into the smooth muscle cells of blood vessels and the heart. In the presence of calcium ions, actin and myosin interact, ensuring contractility of the myocardium and smooth muscle cells. In addition, calcium channels are “involved” in generating pacemaker activity of sinus node cells and conducting impulses through the atrioventricular node. It has been established that the vasodilating effect caused by calcium antagonists occurs not only through a direct effect on the smooth muscles of the vascular wall, but also indirectly through potentiation of the release of NO by the vascular endothelium. This phenomenon was found in most dihydropyridines and isradipine, and to a lesser extent in nifedipine and non-hydropyridine drugs. For long-term treatment of angina from dihydropyridine derivatives, it is recommended to use only prolonged dosage forms or long-acting calcium antagonist drugs. Calcium channel blockers are powerful vasodilators; they reduce myocardial oxygen demand and dilate coronary arteries. The drugs can be used for vasospastic angina and concomitant obstructive pulmonary diseases [1–2.15]. Any practicing physician is well aware of the high effectiveness of nitrates for angina. At the same time, nitrates often cause various side effects - headache (sometimes unbearable), nausea, facial flushing, arterial hypotension, palpitations; With regular use, it is possible to develop tolerance to this group of drugs. In addition, it has been established that the use of nitrates is not indicated for all patients with coronary artery disease. According to the results of the ISIS-4 and GISSI-3 studies (58,050 and 19,394 patients, respectively), the use of nitrates in patients with myocardial infarction does not improve their prognosis. Moreover, the less representative but longer studies MSMI (1072 patients) and MDPIT (1779 patients) demonstrated that long-term use of nitrates after myocardial infarction leads to a significant deterioration in prognosis in these patients. In recent years, another circumstance has emerged that complicates the use of organic nitrates in men suffering from coronary artery disease: they are incompatible with the use of phosphodiesterase type 5 (PDE5) inhibitors, which include sildenafil, tadalafil and vardenafil, used for erectile dysfunction often combined with coronary artery disease [ 16]. Perhaps only drugs from the sydnonimine group can be considered as a serious alternative to nitrates; The first and typical representative is Sidnopharm, one of the widely used molsidomine drugs, its distinctive characteristic is the cost-effectiveness ratio. Molsidomine is an antianginal agent from the sydnonimine group. Not being a nitrate in chemical structure, Sydnopharm (molsidomine) has a similar effect to them, since it is capable of splitting off the nitric oxide molecule – NO; Sydnonimines and nitrates are now often combined into the group of antianginal drugs - nitric oxide donors. When ingested, molsidomine is metabolized in the liver, turning into its active derivative, SIN-1. The latter, entering the blood, is activated (SIN-1A), and the NO-group is split off from it, affecting the process of activation of guanylate cyclase. As a result, GTP is converted to cGMP, which leads to relaxation of the vascular muscle cells and vasodilation. Thus, the vasodilating effect of Sydnofarm is close to the effect of the endothelial relaxing factor. In the coronary system, it is mainly the epicardial arteries that dilate. In the venous system, molsidomine dilates mainly small and medium-sized vessels, which promotes the deposition of blood in it, reduces blood flow to the heart and preload on the heart. In large doses, molsidomine has a dilating effect on the arteries and arterioles, which helps reduce peripheral resistance, blood pressure and afterload. Unlike organic nitrates, which activate guanylate cyclase only after the formation of S-nitrosothiol, Sidnopharm stimulates the formation of cGMP without prior interaction with SH groups. Since the action of molsidomine does not depend on SH groups, tolerance to it does not develop, while depletion of SH groups causes the development of tolerance to nitrates. The resistance of the coronary arteries decreases and blood flow increases by 20%, which improves blood supply to ischemic areas of the myocardium. In this case, the phenomenon of myocardial stealing is not observed. Platelet aggregation decreases, thromboxane formation decreases, platelet adhesion to the vascular wall is suppressed, and the synthesis of prostaglandin (prostacyclin) increases, which inhibits platelet aggregation and has a vasodilatory effect [2,3]. The hemodynamic effects of SIN-1 include a decrease in left ventricular systolic and end-diastolic pressure, stroke volume, mean arterial pressure and systemic vascular resistance, an increase in heart rate and diastolic coronary blood flow [17]. In addition, SIN-1 inhibits intracoronary platelet aggregation in vitro [18] and upon intracoronary administration [19], and also promotes the release of prostacyclin, which also prevents thrombus formation [20]. At the same time, take molsidomine orally at a dose of 8 mg 3 times a day. did not significantly affect blood rheology in patients with coronary artery disease [21]. It is also possible that the molsidomine metabolite SIN-1C has immunomodulatory properties, which may have a beneficial effect on the course of immune processes in the focus of necrosis during myocardial infarction. With long-term use of sydnonimines, tolerance to them or to nitrates does not develop [16,22]. The effect of molsidomine appears after 15–20 minutes, the duration of action is from 1 to 6 hours (on average 4 hours). To prevent angina attacks, tablets of 2–4 mg are taken 2–3 times a day. after meals or use a prolonged-release form - 8 mg tablet (retard) 1 time / day. In more severe cases, you can use a 4 mg tablet (Forte) 3 times a day. or 8 mg (retard) 2 times/day. To stop the attacks of angina pectoris with poor tortoglycerin tolerance, you can take a sublingually 1-2 mg of molsidomin (1/2–1 tablet of 2 mg). The bioavailability of the drug when oral administration is 44–59%, the concentration in plasma reaches the maximum within 1-2 hours, further metabolism with the release of nitrogen oxide and the formation of metabolites is quickly; The half -life (T1/2) Sin -1 is 1-2 hours. The drug is not excreted in unchanged form, 90% of metabolites are excreted from the body with urine. In old age, with liver and heart failure, the effect of the first passage through the liver decreases, and the half -life increases [23]. In severe liver failure (an increase in bromisulfalein test to 20-50%), a slowdown in the excretion and an increase in the concentration of molsidomin in blood plasma was noted. The drug does not cumulates (including in patients with renal failure). Molsidomin expands the peripheral venous vessels, has an anti -aggregate, analgesic and anti -anginal effect. Its venuvial activity is due to the release of nitrogen oxide (No) after a series of metabolic transformations, which stimulates soluble guanilantcyclase, in connection with this, the malaxidomin is considered as the Donator of the NO. As a result of this, the accumulation of the CGMF, which helps to relax the smooth muscles of the vessel wall (to a greater extent - veins). A decrease in preloading even without a direct impact on the contractility of the myocardium leads to the restoration of the violation of the myocardium in oxygen and its receipt that violated during the IBS (the need for oxygen is reduced by 26%). The drug relieves coronary arteries spasm, improves collateral blood circulation, increases the tolerance of loads, reduces the number of angina attacks during physical exertion, suppresses the early phase of platelet aggregation, reduces the release and synthesis of serotonin, thromboxan and other pro -groups. In patients with chronic heart failure, mallicidomin, reducing preload, helps to reduce the size of the heart chambers. It reduces the pressure in the pulmonary artery, reduces the filling of the left ventricle and the tension of the myocardial wall, the stroke of the blood. The clinical efficiency of molsidomin under coronary heart disease is evaluated in a number of clinical studies. In particular, Messin R. et al. [24] conducted a multicenter randomized dual -blind -controlled 6 -weekly study of the effectiveness of conventional (4 mg) and retarded (8 mg) forms of the drug in 90 patients with stable angina pectoris. Against the background of therapy, a reliable increase in the load tolerance and a decrease in the depression of the ST segment during load samples, a decrease in the frequency of sore throat and need for nitroglycerin, and the prolonged form turned out to be somewhat more effective. In 1997, an Accord study was conducted in France, which studied the effect of gratonism on the lumen of the coronary arteries and the prognosis in 700 patients who underwent cylinder transluminal angioplasty. The drug comparison was diltiazem. As a primary point, a six -month mortality in comparison groups was monitored, the secondary points were the frequency of restenoses and a change in the lumen of the coronary arteries with repeated coronarography after six months. The study establishes that lincidomin and molsidomin are more increased by the lumen of the coronary arteries, reduce the frequency of restenoses compared to diltiazem, but do not affect the forecast of the life of coronary patients. This data is partly contrary to the results of a double blind placebo -controlled study conducted by Wohrle J., Hoher M. et al. [25]. The study included 166 patients after coronary angioplasty, receiving within 6 months. Molsidomin 8 mg/day. or placebo. Against the background of pharmacotherapy, the frequency of restenoses was the same as in the placebo group, but the functional class of angina pectoris was noticeably reduced. Along with nitrates, gatelessness can be used in patients with heart failure. So Spring A. et al. We studied the dynamics of changes in the ejection fraction in 30 patients with heart failure. Against the background of basic therapy (ACE inhibitors, diuretics, cardiac glycosides), the release fraction was 33.8%, and after 3 months. After adding mallicidomine (6 mg/day) to the therapy, it increased significantly (up to 44.8%). A comparison of the influence of a 24 -hour infusion of mallicidomine and isosorbide 5 -mononitrate (IS - 5 - 5 - MN) on the pressure level in the pulmonary artery in a randomized double -blind, controlled cross examination in 15 patients with NYHA II - III showed that the malliper to a greater extent Reduces pressure in the pulmonary artery. An interesting observation was made by Lee S. - D. et al. (2001), who described three patients with non -specific aortoarthterity and pulmonary hypertension, in which nitric oxide inhalation effectively reduced the pressure in the pulmonary artery and pulmonary vascular resistance. Molsidomin (unlike Nifedipine) at a dose of 4 mg had the same effect, reducing shortness of breath for a long time, improving hemodynamic parameters and increasing the load tolerance. Recently, data have also appeared about the possibility of using molsidomin in the treatment of primary pulmonary hypertension in newborns. Also, one of the indications for the use of molsidomin can be cirrhosis of the liver with phenomena of portal hypertension. It is known that the use of nitrates and B - blockers allows you to reduce the pressure in the system of the gate vein. Hori N. et al. In 1996, the results of an experimental study on rats were published, during which it was shown that the mallicidomine is more effective than propranolol, reduces the pressure in the porcine vein in experimental animals, and the combination of these drugs has a complete additive effect. The data obtained create the prerequisites for continuing the study of the effectiveness of molsidomin (vice -pharma) with pulmonary and portal hypertension. Thus, Siddhadarm (Molsidomin) can be used in the following clinical conditions. - Stable voltage angina pectoris - with angina of voltage II FC, the drug can be used episodically at a dose of 2–4 mg in 30-60 minutes. to physical activity (or other situation, stereotypically causing an attack of angina pectoris). With angina pectoris III - IV FC, the drug can be prescribed in a daily dose of 16 mg (4 mg 4 times/day). - Acute coronary syndrome - the use of chinfarm is advisable in cases of intolerance to organic nitrates or the rapid development of tolerance to them. Siddom should not be used in the presence of unstable hemodynamics. - Early postinfarct angina pectoris - Siddopharm no less effective than organic nitrates, reduces the number of angina attacks in a daily dose of 16 mg (simple or retarded forms). - stagnant heart failure - vice -power can be used as an addition to standard therapy (IAC, diuretics, cardiac glycosides, b - b -anxis) in cases of insufficient efficiency. In addition, Siddhadarm (Molsidomin) can be prescribed at night with the development of night attacks of heart asthma. Against the background of therapy with molsidomin, the development of side effects is possible, including arterial hypotension (especially with simultaneous intake of alcohol), headache at the beginning of treatment; Dizziness, nausea, allergic reactions in the form of skin rashes, bronchospasm are rarely observed. Possible headache, slowdown in the velocity of psychomotor reactions, nausea, loss of appetite, diarrhea. Contraindications to the use of the drug are cardiogenic shock; arterial hypotension; glaucoma (especially closed); I trimester of pregnancy and lactation; decrease in central venous pressure; hypersensitivity to the components of the drug. The simultaneous use of vascular, antihypertensive drugs and ethanol increases the severity of the antihypertensive effect. When Sidnofarm is used simultaneously with acetylsalicylic acid, its antiplatelet effect is enhanced. Thus, the advantages of the drug include proven effectiveness for coronary heart disease, stenard of stress and congestive heart failure, the best tolerance compared to nitrates and lack of tolerance to the drug with regular use for a long time. All this determines the broad prospects for the use in the wide clinical practice of the antianginal drug Molsidomin (Sidnopharm), especially in the conditions of an increase in the incidence of cardiovascular pathology, an increase in resistance to nitrates and often their poor tolerance.
Literature 1. Shchukin Yu.V., Ryabov A.E. Chronic ischemic heart disease in old and senile age. A manual for doctors. - Samara: Volga-Business Publishing House, 2008. - 44 p. 2. Kosarev V.V., Babanov S.A. Clinical pharmacology of drugs used for cardiovascular diseases. – Samara. – “Ofort”. – 2010. – 140 p. 3. Kosarev V.V., Babanov S.A., Astakhova A.V. Pharmacology and drug therapy. Ed. V.K. Lepakhina. M.: Eksmo, 2009. 4. Shalnova S.A., Deev A.D., Oganov R.G. Factors influencing mortality from cardiovascular diseases in the Russian population. Cardiovasc. ter. and prof. 2005; 4(1):4–9. 5. Russian recommendations “Diagnostics and correction of lipid metabolism disorders for the purpose of prevention and treatment of atherosclerosis.” Section of atherosclerosis VNOK // Cardiovascular therapy and prevention. 2004. No. 2 (appendix).36 p. 6. The Cholesterol and Recurrent Events Trail Investigators. The 14. effect of pravastatin on coronary events after myocardial infarction in patientd with average cholesterol levels. N Engl J Med 1998; 335:1001–9. 7. Athyros 15. VG, Papageorgiou AA, Mercouris BR. The Greek Atorvastatin and acoranary heart disease Evaluation (GREECE) Study. Curr Med Res Opin 2002; 18: 220–8. 8. Serruys PW, de Feuter P, Macaya C et al. Intervention Prevention 16. Study (LIPID) Investigators. Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trail. JAMA 2002; 287:3215–2. 9. Shepherd J, Cobbe SM, Ford I et 17. al., for the West of Scotland Coronary Prevention Study Group. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med 1995; 333:1301–7. 10. Downs JR, Clearfield M, Weis S et al., for the 18. AFCAPS/TexCAPS Research Group, (1998). Primary Prevention of Acute Coronary Events With Lovastatin in Men and Women With Average Cholesterol Levels: Results of AFCAPS/TexCAPS. JAMA 279:1615–22. 11. Kleemann R., Kooistra T. HMG–CoA Reductase Inhibitors: Effects on Chronic Subacute Inflammation and Onset of Atherosclerosis Induced by Dietary Cholesterol. Curr Drug Targets Cardiovasc Haematol Disord. 2005 Dec;5(6):441–53. 12. Oganov R. G., Maslennikova G. Ya. Cardiovascular diseases in the Russian Federation in the second half of the twentieth century: trends, possible causes, prospects. – Cardiology, 2000. – No. 6. – P. 4–8. 13. Olbinskaya L. I., Lazebnik L. B. Nitric oxide donors in cardiology. – M., 1998. – 172 p. 14. Aronov D.M., Lupanov V.P. Diagnosis and treatment of chronic coronary heart disease. The quality of life. Medicine. 2003; 2: 16–24. 15. Lupanov V.P. Stable angina: tactics of treatment and management of patients in hospital and outpatient settings. Rus. honey. magazine 2003; 11 (9): 556–63. 16. Agvald P, Adding LC, Gustafsson LE, Persson MG. Nitric oxide generation, tachyphylaxis and cross-tachyphylaxis from nitrovasodilators in vivo. Eur J Pharmacol. 1999. 1999; 385(2–3):137–45. 17. Arkonac BM, Kersten JR, Wynsen JC, Nijhawan N, Warltier DC. Differential hemodynamic effects of the nitric oxide donor pirsidomine in comparison to SIN–1, nitroprusside, and nitroglycerin. Pharmacology. 1996; 52:92–100. 18. Darius H, Ahland B, Rucker W, Klaus W, Peskar BA, Schror K. The effects of molsidomine and its metabolite SIN–1 on coronary vessel tone, platelet aggregation, and eicosanoid formation in vitro: Inhibition of 12–HPETE biosynthesis . J Cardiovasc Pharmacol. 1984; 6:115–121. 19. Ovize M, Lorgeril M, Cathignol D, Delaye J, Renaud S. Inhibition of coronary artery thrombosis by SIN-1, a donor of nitric oxide. J Cardiovasc Pharmacol. 1990; 16:641–645. 20. Salvemini D, Currie MG, Mollace V. Nitric oxide–mediated cyclooxygenase activation: A key event in the antiplatelet effects of nitrovasodilators. J Clin Invest. 1996; 97:2562–2568. 21. Wohrle J, Nusser T, Hoffmeister A, Kestler HA, Grebe OC, Hoher M, Hombach V, Koenig W, Kochs M. Dtsch Med Wochenschr. 2003; 128(24):1333–7. 22. Schror K, Forster S, Woditsch I. On–line measurement of nitric oxide release from organic nitrates in the intact coronary circulation. Naunyn–Schmiedeberg's Arch Pharmacol. 1991, 344:240–246. 23. Rosenkranz B, Winkelmann BR, Parnham MJ. Clinical pharmacokinetics of molsidomine. Clin Pharmacokinet. 1996; 30(5):372–84. 24. Messin R, Karpov Y, Baikova N, Bruhwyler J, Monseu MJ, Guns C, Geczy J. Short– and long–term effects of molsidomine retard and molsidomine nonretard on exercise capacity and clinical status in patients with stable angina: a multicenter randomized double–blind crossover placebo–controlled trial. J Cardiovasc Pharmacol. 1998; 31(2):271–6. 25. Wohrle J, Hoher M, Nusser T, Hombach V, Kochs M. No effect of highly dosed nitric oxide donor molsidomine on the angiographic restenosis rate after percutaneous coronary angioplasty: a randomized, placebo controlled, double–blind trial. Can J Cardiol. 2003; 19(5):495–500. 26. Lee S.–D., Kim D.–S., Shim T.–S., Lim C.–M., Koh Y., Kim W.–S., Kim W.–D. Nitric Oxide and Molsidomine in the Management of Pulmonary Hypertension in Takayasu's Arteritis. Chest, 2001; 119(1): 302 – 307.
Metabolic and antioxidant therapy
“Antioxidant therapy” fits harmoniously into traditional treatment regimens for coronary heart disease thanks to the use of drugs such as statins, ACE inhibitors, and carvedilol, which have a pronounced antioxidant effect. At the same time, the beneficial anti-ischemic, cardioprotective and anti-atherosclerotic effects of “pure” antioxidants (bioflavonoids, polyphenols, vitamins, glutathione, emoxypine, ethylmethylhydroxypyridine), shown in various biological models, have not currently been demonstrated in any large clinical study. Several prospective placebo-controlled RCTs have shown neutral and even negative effects of vitamins [18]. It was recently discovered that a number of experiments in which the positive effects of quercetin were shown were carried out with gross violations of biomedical ethics [19]. Thus, the use of antioxidants by patients with coronary artery disease, including as part of dietary supplements, is not justified.
Metabolic drugs also have a rather poor evidence base. In this regard, the European Agency for the Evaluation of Medicines has reduced the range of indications for the use of the drug trimetazidine, which can only be used as an additional antianginal agent in case of intolerance or insufficient effectiveness of first-line therapy [20]. Angina caused by microvascular dysfunction can be indicated as an area of rational use of trimetazidine as part of complex antianginal therapy.
In Russia, the drug meldonium, an analogue of γ-butyrobetaine, is also used in the treatment of patients with coronary artery disease. Meldonium inhibits the enzyme γ-butyrobetaine hydroxylase, which leads to a slowdown in the biosynthesis of carnitine and the transport of long-chain fatty acids across the mitochondrial membrane in vitro (at the same time, β-oxidation of fatty acids slows down, and intracellular metabolism “switches” to glycolysis). The drug L-carnitine has the opposite effect, accelerating the transport of long-chain fatty acids into mitochondria, the β-oxidation of which is much more energetically beneficial, but also requires larger amounts of oxygen. The question of which of these strategies can be considered optimal in clinical practice, when long-term chronic myocardial ischemia can give way to acute with the development of ACS, remains open.