- home
- Articles
- For a healthy lifestyle!
- Treatment of angina
If you have been diagnosed with coronary heart disease
,
angina pectoris
, your doctor will definitely prescribe you treatment - drug therapy, which he will recommend taking constantly, without interruptions. Why do you need to take medications regularly? And what drugs are used to treat angina pectoris, in what doses?
The first and most important thing in the presence of angina is to prevent complications of the disease ( myocardial infarction
, life-threatening heart rhythm disturbances, development of severe heart failure) and death, prolong your life.
Second and no less significant: improve the quality of your life, make it complete, eliminate pain. There are several main groups of drugs for the treatment of angina
. Let's figure out how they work and why doctors prescribe them for treatment.
Antiplatelet agents
Antiaggregates help prevent the formation of blood clots (thrombi), reduce the aggregation (sticking together) of platelets - blood cells that are responsible for the formation of a blood clot. The list of antiplatelet agents includes: aspirin, cardiomagnyl, thienopyridines.
Aspirin (acetylsalicylic acid)
Aspirin (acetylsalicylic acid)
– the main antiplatelet agent, it is prescribed to all patients suffering from angina pectoris (with the exception of those who cannot tolerate it, for example, allergy sufferers with the “aspirin triad”). The dose of aspirin is 75-150 mg daily. Taken once, every 20-30 minutes. after meal. Typically in the afternoon. Pay attention to the low dose! A typical aspirin tablet contains 500 mg, a dose that has been taken as an analgesic and antipyretic for over 100 years! For angina pectoris, no more than 1/4 tablet is recommended. This dose effectively prevents thrombosis and is quite safe for the stomach. When regularly taking higher doses of aspirin (acetylsalicylic acid), there is a risk of developing erosions and stomach ulcers. Since patients with angina pectoris require constant use of aspirin as treatment, special, safer forms for long-term use have been developed.
Cardiomagnyl (aspirin + magnesium hydroxide)
Cardiomagnyl (aspirin + magnesium hydroxide)
75 and 150 mg. Magnesium hydroxide, which is part of the tablet, stimulates the formation of special protective substances in the stomach wall of a patient with angina pectoris that prevent the formation of ulcers and erosions.
Enteric-coated aspirin (AspirinCardio 100 mg, ThromboAss 50 and 100 mg, CardiASK 50 mg, etc.)
. The special coating does not allow the tablet to dissolve in the stomach; absorption of aspirin occurs in the intestines. Important: these tablets must be taken whole, you cannot break them or chew them (otherwise you will damage the shell and the protective effect will disappear)!
Thienopyridines (clopidogrel, prasugrel, ticlopidine)
Thienopyridines (clopidogrel, prasugrel, ticlopidine)
– have a very pronounced antiplatelet effect, hundreds of times stronger than aspirin.
The prescription of these drugs (usually together with aspirin) is necessary in cases where the risk of thrombosis is very high: unstable angina
,
acute coronary syndrome
(“pre-infarction conditions”),
acute myocardial infarction
and cardiac surgery (
stenting
,
coronary artery bypass grafting
and etc.). Thienopyridines are also prescribed as a treatment for those patients who cannot take aspirin due to intolerance or contraindications.
Important:
Tell your doctor if you have previously had a stomach ulcer, duodenal ulcer (DU) or erosive gastritis, as well as unstable blood pressure with frequent crises, rises above 160-170/100 mm Hg. Art. This information will help your doctor make your antiplatelet treatment safe. It has been proven that regular use of antiplatelet drugs can reduce the incidence of myocardial infarction, strokes and death in patients with angina pectoris by up to 23% (in every 23 people out of 100)! After coronary angioplasty and stenting operations, doctors recommend taking aspirin and clopidogrel together for a certain period of time (from a month to several years).
Sources
- Arkhipova N.V., Argunova YA., Pomeshkina E.E. . // Vopr Kurortol Fizioter Lech Fiz Kult - 2021 - Vol98 - N2 - p.65-69; PMID:33899454
- Nenna A., Nappi F., Spadaccio C., Greco SM., Pilato M., Stilo F., Montelione N., Catanese V., Lusini M., Spinelli F., Chello M. Advanced measurements of coronary calcium scores: how does it affect current clinical practice? // Future Cardiol - 2021 - Vol - NNULL - p.; PMID:33885330
- Yang S., Shao Y., Yan Q., Wu C., Yang H., Zou J. Differential Diagnosis Strategy between Lower Extremity Arterial Occlusive Disease and Lumbar Disc Herniation. // Biomed Res Int - 2021 - Vol2021 - NNULL - p.6653579; PMID:33884268
- Yang Y., Xiao F., Wang J., Song B., Li XH., Zhang SJ., He ZS., Zhang H., Yin L. [One-stage surgery in patients with both cardiac and non-cardiac diseases ]. // Beijing Da Xue Xue Bao Yi Xue Ban - 2021 - Vol53 - N2 - p.327-331; PMID:33879906
- Dang W., Wang J., Zhang Q., Liu N., Li W., Yao Z. Analysis of individualized antiplatelet therapy for patients of acute coronary syndrome after percutaneous coronary intervention under the guidance of platelet function: A one-center retrospective cohort study. // Medicine (Baltimore) - 2021 - Vol100 - N16 - p.e25601; PMID:33879725
- Cao S., He T., Xie J., Feng H., Liu K., Qu B., Wu X. Drug-coated balloon angioplasty versus balloon angioplasty for treating patients with in-stent restenosis in the femoropopliteal artery: A meta -analysis. // Medicine (Baltimore) - 2021 - Vol100 - N16 - p.e25599; PMID:33879723
- Zhang J., Jing R., Liu JJ., Di CY., Lu YJ., Gao P., Wang YJ., Yang RF., Lin WH. . // Zhonghua Yi Xue Za Zhi - 2021 - Vol101 - N15 - p.1064-1070; PMID:33878833
- Koskinas KC., Mach F., Räber L. Lipid-lowering therapy and percutaneous coronary interventions. // EuroIntervention - 2021 - Vol16 - N17 - p.1389-1403; PMID:33875408
- Byrne L., Wheen P., O'Connor S. Emergency TAVI in cardiogenic shock and cardiorenal syndrome secondary to severe bicuspid aortic stenosis. // BMJ Case Rep - 2021 - Vol14 - N4 - p.; PMID:33863765
- Karbasiafshar C., Sellke FW., Abid MR. Mesenchymal stem cell-derived extracellular vesicles in the failing heart: past, present, and future. // Am J Physiol Heart Circ Physiol - 2021 - Vol - NNULL - p.; PMID:33861149
Statins
Statins – antiatherosclerotic drugs
, reduce the level of “bad” cholesterol in the blood (total cholesterol, LDL, triglycerides), increase the level of “good” cholesterol (HDL). With long-term use of the drug in a dose that allows you to control cholesterol at the target level, they can stop the growth of atherosclerotic plaques and even reduce their size. Target cholesterol levels depend on the prevalence of atherosclerosis in the body and associated diseases (for example, diabetes). Ask your doctor what your target levels should be and monitor the effectiveness of treatment (blood tests for cholesterol and lipids) at least 4 times a year. There is no habituation to statins or development of dependence; treatment with statins should be carried out continuously. If you stop taking it on your own, then within one month after stopping the drug, your blood lipid levels return to baseline.
Statins
can reduce the risk of
myocardial infarction
and stroke by up to 30-40% (in every 30-40 people out of 100), and this effect is more pronounced in diabetics!
The fact that statins save lives became known after several large studies, which involved thousands and tens of thousands of patients with angina pectoris
, diabetes mellitus, and peripheral atherosclerosis.
Today, statins are recommended for treatment not only for patients with angina
, but also for people without coronary artery disease, with several risk factors, for the prevention of atherosclerosis, heart attack and stroke.
Four drugs in this group are registered in Russia: simvastatin (Zocor), rosuvastatin (Crestor), atorvastatin (Liprimar) and fluvastatin (Leskol).
How to take statins
Take statins in the evening (before bedtime). There are medications that can be taken at any time of the day. Nausea and stool disturbances are possible. The use of statins is not recommended for persons with active liver disease or during pregnancy and breastfeeding. A very rare side effect is muscle pain. If you start taking the drug and notice soreness in all the muscles of your body, be sure to tell your doctor to avoid unwanted complications. If you do not tolerate statins well or taking the maximum therapeutic dose does not allow you to control lipid levels, then it is possible to reduce the dose and add a cholesterol absorption inhibitor, ezetimibe. Your doctor may also recommend the use of other lipid-lowering drugs for treatment: fibrates, delayed-release nicotinic acid.
Prevention
Preventing a disease is much easier than curing it. To maintain healthy arteries and blood vessels, it is necessary to eliminate risk factors that negatively affect your health:
- To give up smoking;
- Monitoring blood pressure levels
- Normalization of the level of “bad” cholesterol (low-density lipoproteins)
- Fighting stress and depression
- Minimize alcohol consumption;
- Refusal of smoked, fatty, fried and salty foods.
Spend more time on an active lifestyle: moderate physical activity, therapeutic exercises, morning exercises, walking, swimming, dancing. Physical activity will help strengthen the walls of blood vessels and maintain normal weight, and if necessary, reduce it.
The most important thing in prevention is timely observation by a specialist. In order not to visit medical institutions several times to undergo all the necessary tests and examinations, contact our cardiology center. Federal Research Center FMBA offers patients several programs for comprehensive heart research. You can find them here.
Beta blockers
Beta blockers
– reduce the heart rate (pulse), thereby reducing the work performed by the heart and the need of the heart muscle (myocardium) for oxygen, improving blood supply to the heart, reducing the number of
angina attacks
and increasing exercise tolerance.
Beta blockers prevent and treat abnormal heart rhythms (arrhythmias). This is especially important after a myocardial infarction
, when the arrhythmia often becomes life-threatening.
Regular use of beta blockers can prevent the death of patients who have had a heart attack by up to 40% (in every 40 people out of 100!). Therefore, they are recommended to be prescribed to all patients after a heart attack
, in the absence of contraindications.
Beta blockers normalize blood pressure. In most patients, angina is combined with arterial hypertension
, in this case, taking a beta blocker “kills two birds with one stone” -
we treat hypertension and angina
at the same time. Some beta blockers have been shown to prevent the development of heart failure. These include metaprolol succinate (BetalokZOK), bisoprolol (Concor), nebivalol (Nebilet), carvedilol (Dilatrend). This effect, just like all of the above, is possible only with regular long-term use of the drug.
How to take beta blockers
Take a beta blocker daily, in the morning (long-acting drugs, about 24 hours) or twice a day (morning and evening). The dose of the beta blocker is selected individually. The dose is considered effective if your resting heart rate is 50-60 beats per minute while taking the drug. In this case, all the therapeutic effects of the drug are manifested. You should not suddenly stop taking the beta blocker - in the first days, your pulse may reflexively increase sharply and your health will worsen. In those patients with angina
who take a beta blocker to maintain the correct rhythm and prevent arrhythmia, after discontinuation, interruptions in heart function may resume. Undesirable effects of beta blockers are characteristic mainly of non-cardioselective drugs (for example, decreased potency), and in modern highly cardioselective drugs they occur rarely, usually with increasing doses. It is undesirable to prescribe beta blockers to patients with bronchial asthma and chronic obstructive pulmonary disease COPD), atherosclerotic lesions of the arteries of the lower extremities (atherosclerosis obliterans).
Observation
Duration of treatment
Treatment of coronary artery disease lasts a lifetime and must be carefully planned. During the observation period, it is necessary to strictly adhere to the developed treatment regimen, and if side effects occur or the condition worsens, immediately contact your doctor.
Many medications must be taken for life. These include aspirin (or analogs), blood pressure medications, medications to normalize blood sugar and cholesterol, and in some cases other medications. Sudden withdrawal of medication at will or even a reduction in dose can lead to a sharp deterioration in health and decompensation, and this increases the likelihood of fatal complications (heart attack, cardiac arrest, etc.).
Changes regarding lifestyle and routine must be decisive and unconditional. Often, small mistakes in the diet, such as eating too much herring, can lead to a sharp rise in blood pressure and worsening of the disease.
Doctor visits
Usually the doctor himself sets the date for the next visit. If he didn't, ask him about it. Careful medical supervision and regular checks are a necessary and important component of treatment. If you are unsure or doubt the adequacy of your doctor’s prescriptions, or want to get additional advice, contact a specialized advisory or diagnostic cardiology center.
Preventive hospitalizations
In the former USSR, the phenomenon of hospitalization for prevention was common. In the case of coronary artery disease, such a treatment strategy is not optimal either from the point of view of the quality of disease control or from the point of view of the patient's adherence to treatment, and should be avoided.
Treatment intermittently, from time to time, does not provide the necessary control over risk factors and the course of the disease for ischemic heart disease. Patients begin to be inclined to think that they will be “treated”, after which they will go back to their previous lives, and everything will be as before. This is a big misconception, which leads to refusal to take medications on a regular basis, large fluctuations in blood counts and pressure, and lack of control over the disease.
In one or two weeks spent in hospital every six months, it is impossible to achieve any real change in the course of the disease, other than some symptomatic improvement. Many patients perceive this improvement as a small victory over the disease and continue to live their previous lives. However, this is not at all true: coronary artery disease continues to progress without lifestyle changes and maintenance medications, ending in sudden death or heart attack. You can reduce your risk and prolong your life only with long-term, and not periodic, therapeutic effects.
Calcium agonists
Calcium agonists - are able to dilate the blood vessels of the heart, increasing the flow of blood to the heart muscle (myocardium), thereby reducing the number of angina attacks
.
They are divided into three main groups with characteristic features. Drugs from the group of dihydropyridine calcium antagonists
(nifedipine) can be prescribed together with beta blockers, or instead of beta blockers (if intolerance or contraindications to the latter).
The first generations (nifedipine) increase the heart rate, so short-acting tablets (nifedipine 10 mg) are prohibited for angina pectoris. There are special prolonged forms (osmo-adalat, corinfar-retard, nifecard) containing from 20 to 60 mg of nifedipine. The third generation of drugs (amlodipine, felodipine) practically does not increase the pulse rate and is taken once a day. Drugs from the verapamil and diltiazem group
reduce the heart rate; combined use with beta blockers is contraindicated due to the risk of bradycardia and other complications. It has been proven that regular use of calcium antagonists can reduce the incidence of strokes.
If-channel inhibitors (coraxan)
If-channel inhibitors, the only representative today is ivabradine (Coraxan)
.
The drug is able to reduce the heart rate (pulse), thereby reducing the number of angina attacks
. Unlike beta blockers, this inhibitor is effective only in sinus rhythm, does not affect heart rhythm disturbances and blood pressure, and is a symptomatic drug (eliminates symptoms of the disease). The effect on the prognosis has not yet been proven (research is ongoing). An inhibitor can be prescribed instead of beta blockers (if intolerance or contraindications to the latter) or together with beta blockers to achieve the target heart rate (50-60 beats per minute).
How to take Coraxan
Coraxan
take 2.5-5-7.5 mg 2 times a day (morning and evening). Ivabradine is not recommended if: resting heart rate is below 60 beats/min (before treatment), severe arterial hypotension (SBP below 90 mmHg and DBP below 50 mmHg), severe hepatic insufficiency, sick sinus syndrome was diagnosed, sinoatrial block or AV block of the third degree, a permanent form of atrial fibrillation, chronic heart failure stage III-IV according to the NYHA classification (there is not enough clinical data yet), an artificial pacemaker was implanted.
Factors contributing to the development of ischemic heart disease
The main causes of the development of coronary heart disease can be identified:
- Arterial hypertension (increases the likelihood of developing ischemia by 2-6 times);
- smoking (in tobacco addicts, the risk of developing coronary heart disease is 1.5-6 times higher than in non-smokers);
- disturbance of lipid and lipoprotein metabolism (promotes the development of atherosclerosis and increases the risk of ischemia by 2-5 times);
- physical inactivity and obesity (obese, inactive people get sick at least 3 times more often than thin and athletic people);
- disorders of carbohydrate metabolism, diabetes mellitus (with both types of diabetes, the risk of developing coronary heart disease increases by 2-4 times).
Risk factors also include family history, being of the stronger sex, and old age. When two or more of the listed positions are combined, the risk of developing IHD increases significantly.
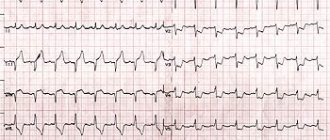
1 ECG for cardiac ischemia
2 ABPM in the diagnosis of ischemia
3 ECHO-CG for ischemic heart disease
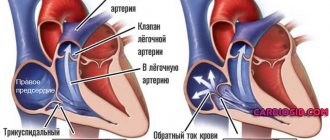
Angiotensin-converting enzyme inhibitors (ACEIs)
Angiotensin-converting enzyme inhibitors (ACEIs)
–
for angina pectoris,
they are prescribed to prevent the development of heart failure.
Therefore, drug doses are usually lower than for the treatment of hypertension. If after a MI you develop symptoms of heart failure or doctors identify impaired LV function, adding an ACE inhibitor to your therapy will significantly reduce the risk of death and the likelihood of a recurrent MI. The effect of drugs such as ramipril, trandolapril, zofenopril, enalapril has been proven. If these drugs are poorly tolerated, it is possible to replace them with angiotensin receptor antagonists. ACE inhibitors can be prescribed for angina pectoris without a history of heart attack
- their ability to slow the progression of atherosclerosis has been proven. The effect of the drugs ramipril and perindopril has been proven.
Nitrates
Nitrates
– used
to relieve anginal pain due to angina pectoris
for more than 100 years!
They are symptomatic (pain-relieving) drugs and do not affect mortality or life expectancy. The effect of nitrates is a short-term dilation of the blood vessels supplying the heart. There are many forms of nitrate release available for different situations. For example, short-acting nitrates, nitroglycerin in the form of sublingual tablets (under the tongue), spray (Isoket, Nitromint, etc.) for quick relief of an attack of angina. Instantly relieves pain, lasts for 10-15 minutes. They are used not only to relieve an attack that has already occurred, but also to prevent it (for example, before starting physical activity or in other situations in which, in your opinion, an angina attack
). Capable of sharply reducing blood pressure for a short time.
Rules for using short-acting nitroglycerin:
- Sit or lie down.
- Take nitroglycerin (put a tablet under your tongue or spray the drug under your tongue).
- You can take 1-3 doses of nitroglycerin, with a break of about 5 minutes between doses.
- Let others know that you are having an attack and are not feeling well.
- If the pain does not stop after 15 minutes, call an ambulance.
Nitrates
moderate duration of action (nitrosorbitol, isosorbide mononitrate and dinitrate 20 and 40 mg, etc.) act for several hours (up to 6 hours) and are used
to prevent angina attacks
.
As a rule, these forms of nitrates are prescribed 2-3 times a day. Remember - if nitrates enter your body continuously, then after a few days the sensitivity of your blood vessels to nitroglycerin will significantly decrease and the drug will no longer prevent angina attacks
. Therefore, when treating with nitrates of average duration of action, “nitrate-free intervals” of up to 6-8 hours are necessary. Your doctor will prescribe you to take the drug in the morning and afternoon (before 17.00), or in the afternoon and evening, etc. Long-acting nitrates (retarded forms of nitrates, 50 mg) will help avoid the development of tolerance to nitrates. Such drugs are taken once a day, the effect lasts up to 10 hours, providing the necessary intervals to restore vascular sensitivity.
Remember:
Long-acting nitrates cannot be the main method of treatment!
It is recommended to prescribe nitrates only if you are taking the main groups of drugs in an effective dose, but you continue to have angina attacks
. Short-acting nitrates - used as required. Taking nitrates is relatively often associated with the appearance of side effects (primarily headaches), the development of addiction (tolerance) to the drug when taken regularly, and the possibility of “rebound” syndrome when the drug is abruptly stopped entering the body.
Diagnosis of coronary heart disease
The success of preventive and therapeutic measures depends on the timely detection of the disease and correct diagnosis.
Of course, the initial stage of diagnosing IHD is the collection and analysis of the patient’s complaints. This is followed by an examination, during which the cardiologist measures the patient’s blood pressure, visually assesses his condition (degree of swelling, skin tone, sweating, behavioral characteristics, etc.), listens to his heart with a stethoscope for murmurs, rhythm disturbances, etc.
Next, the specialist may prescribe the following tests and studies:
- clinical and biochemical blood tests;
- blood test for markers of myocardial infarction;
- electrocardiography (ECG);
- echocardiography (Echo-CG);
- ABPM;
- ECG with stress;
- coronary angiography (x-ray contrast examination of the coronary arteries).
1 Ultrasound of the heart for ischemic heart disease
2 Diagnostics of coronary artery disease in "MedicCity"
3 ABPM for ischemic heart disease
Cytoprotectors
Cytoprotectors
– protects against the death of heart muscle cells during episodes of acute and chronic oxygen deprivation (ischemia), allowing the cells to produce energy to pump the heart using less oxygen.
There is an evidence base for the drug trimetazidine (Preductal MV). The drug has no contraindications (except for individual intolerance) and side effects. Partnership between doctor and patient is the key to successful treatment of angina pectoris.
Still have questions? Make an appointment! Using materials from the article by N.S. Veselkova