Composition of the drug and dosage form
The drug is available in different doses. Accordingly, the names of medications differ. The drug with the lowest content of active substance (10 milligrams) is called Corinfar. A product containing 20 milligrams of the active ingredient already has the prefix Retard. The drug with the maximum concentration of the active substance (40 milligrams) is called Corinfar Uno.
The drug is available in the form of yellow-coated tablets. In addition to the active substance - nifedipine, the content of which is determined depending on the dose, the tablets contain:
- lactose;
- starch;
- microcrystalline cellulose;
- povidone;
- Magnesium stearate.
The mechanism of action on pressure, increases or decreases
The active ingredient of the drug lowers blood pressure and helps reduce the load on the heart.
When using the drug, there is also a decrease in the load on the heart muscle and vascular walls.
If blood pressure is high and heart rate is high, these levels are normalized in patients taking the drug by reducing the number and force of heart contractions.
The drug also has the following effects in patients with high blood pressure:
- improves blood flow in the coronary vessels;
- contributes to the normalization of the functioning of branching vessels;
- hypotensive effect;
- There is a significant improvement in the part of the heart muscle with poor blood supply.
Corinfar®
Pharmacokinetic interactions
Medicines that affect the metabolism of nifedipine
Nifedipine is metabolized by CYP3A4/5 isoenzymes, which are located in the intestinal mucosa and liver. Drugs that inhibit or induce this enzyme system may affect the first pass effect through the liver (after oral administration) or the clearance of nifedipine.
Inducers of the CYP3A4 isoenzyme
Rifampicin
Rifampin is a potent inducer of the CYP3A4 isoenzyme. When used simultaneously with rifampicin, the bioavailability of nifedipine is significantly reduced and, accordingly, its effectiveness is reduced. Therefore, the simultaneous use of nifedipine with rifampicin is contraindicated.
Antiepileptic drugs that induce CYP3A4 (eg, phenytoin, carbamazepine, phenobarbital)
Phenytoin induces the CYP3A4 isoenzyme. With the simultaneous use of nifedipine and phenytoin, the bioavailability of nifedipine is reduced and its effectiveness is reduced. When using this combination simultaneously, it is necessary to monitor the clinical response to nifedipine therapy and, if necessary, increase its dose. If the dose of nifedipine is increased with simultaneous use of both drugs, the dose of nifedipine should be reduced after discontinuation of phenytoin.
Clinical studies examining the potential interaction between nifedipine and carbamazepine or phenobarbital have not been conducted. Since both drugs reduce the concentration of nimodipine in the blood plasma, which is structurally similar to BMCC, the possibility of a decrease in the concentration of nifedipine in the blood plasma and a decrease in its effectiveness cannot be excluded.
CYP3A4 isoenzyme inhibitors
Macrolide antibiotics (for example, erythromycin)
Clinical studies on the interaction of nifedipine and macrolide antibiotics have not been conducted. Some macrolides are known to inhibit the CYP3A4 isoenzyme. As a result, the possibility of an increase in the concentration of nifedipine in the blood plasma cannot be excluded with the simultaneous use of nifedipine and macrolide antibiotics.
Azithromycin, a macrolide antibiotic, does not inhibit the CYP3A4 isoenzyme.
HIV protease inhibitors (eg, ritonavir)
Clinical studies examining the interaction of nifedipine and HIV protease inhibitors have not been conducted. It is known that drugs of this class inhibit the CYP3A4 isoenzyme. In addition, drugs of this class have been shown to suppress the metabolism of nifedipine mediated by the CYP3A4 isoenzyme in vitro. When used simultaneously with nifedipine, a significant increase in the concentration of nifedipine in the blood plasma cannot be ruled out due to a decrease in the effect of “first pass” through the liver and slower elimination.
Azole antifungals (eg, ketoconazole)
Clinical studies examining the interaction of nifedipine and azole antifungals have not been conducted. It is known that drugs of this class inhibit the CYP3A4 isoenzyme. When used simultaneously with nifedipine, a significant increase in the systemic bioavailability of nifedipine is possible by reducing the effect of “first pass” through the liver.
Cimetidine and ranitidine
It has been established that cimetidine and ranitidine inhibit the CYP3A4 isoenzyme and cause an increase in the concentration of nifedipine in the blood plasma (by 80% and 70%, respectively), thereby enhancing its antihypertensive effect.
Diltiazem
Diltiazem reduces the clearance of nifedipine. This combination should be used with caution. A dose reduction of nifedipine may be required.
Fluoxetine
Clinical studies examining the interaction of nifedipine and fluoxetine have not been conducted. It is known that fluoxetine in vitro suppresses the metabolism of nifedipine, mediated by the action of the CYP3A4 isoenzyme. Therefore, the possibility of an increase in the concentration of nifedipine in the blood plasma cannot be excluded with the simultaneous use of nifedipine and fluoxetine.
Nefazodone
Clinical studies examining the interaction between nifedipine and nefazodone have not been conducted. Nefazodone is known to inhibit the metabolism of other drugs mediated by the CYP3A4 isoenzyme. Therefore, the possibility of increased plasma concentrations of nifedipine cannot be excluded with simultaneous use of nifedipine and nefazodone.
Quinidine
Increased plasma concentrations of nifedipine have been reported when administered concomitantly with quinidine. Therefore, careful monitoring of blood pressure is necessary when using quinidine and nifedipine simultaneously. If necessary, the dose of nifedipine should be reduced.
Quinupristin/dalfopristin
Concomitant use of quinupristin/dalfopristin may lead to increased plasma concentrations of nifedipine.
Valproic acid
Clinical studies examining the interaction of nifedipine and valproic acid have not been conducted. Since valproic acid increases the concentration of nimodipine in the blood plasma, which is structurally similar to BMCC, the possibility of increasing the concentration of nifedipine in the blood plasma and enhancing its effectiveness cannot be excluded.
Grapefruit juice
Grapefruit juice inhibits the CYP3A4 isoenzyme and suppresses the metabolism of nifedipine. The simultaneous use of the drug with grapefruit juice leads to an increase in the concentration of nifedipine in the blood plasma and a prolongation of its action due to a decrease in the “first pass” effect through the liver and a decrease in clearance. This may enhance the antihypertensive effect of nifedipine. With regular consumption of grapefruit juice, this effect can last for 3 days after the last consumption of the juice. Consumption of grapefruit/grapefruit juice during treatment with nifedipine is contraindicated.
CYP3A4 isoenzyme substrates
Substrates of the CYP3A4 isoenzyme (for example, cisapride, tacrolimus, benzodiazepines, imipramine, propafenone, terfenadine, warfarin), when used simultaneously with nifedipine, may act as CYP3A4 inhibitors and increase the concentration of nifedipine in the blood plasma.
Cisapride
Concomitant use of cisapride and nifedipine may lead to increased plasma concentrations of nifedipine.
Effect of nifedipine on other drugs
Quinidine
Nifedipine causes a decrease in the concentration of quinidine in the blood plasma. After discontinuation of nifedipine, a sharp increase in the concentration of quinidine in the blood plasma may occur. Therefore, when using nifedipine as additional therapy or discontinuing nifedipine, the concentration of quinidine in the blood plasma should be monitored and, if necessary, its dose should be adjusted.
Digoxin
The simultaneous use of nifedipine and digoxin may lead to a decrease in the clearance of digoxin and, consequently, to an increase in the concentration of digoxin in the blood plasma. The patient should be carefully monitored for symptoms of glycoside overdose and, if necessary, reduce the dose of digoxin, taking into account its concentration in the blood plasma.
Theophylline
Nifedipine increases the concentration of theophylline in the blood plasma, and therefore the concentration of theophylline in the blood plasma should be monitored. The clinical effect of both drugs when used together does not change.
Tacrolimus
Tacrolimus is metabolized with the participation of the CYP3A4 isoenzyme. Recently published data indicate the possibility of increased tacrolimus concentrations in selected cases when administered concomitantly with nifedipine. When using tacrolimus and nifedipine simultaneously, the concentration of tacrolimus in the blood plasma should be monitored and, if necessary, its dose should be reduced.
Vincristine
Nifedipine slows down the elimination of vincristine from the body and may cause increased side effects of vincristine. If simultaneous use is necessary, reduce the dose of vincristine.
Drugs that bind to blood proteins
Nifedipine can displace drugs characterized by a high degree of binding from protein binding (including indirect anticoagulants - coumarin and indanedione derivatives, anticonvulsants, non-steroidal anti-inflammatory drugs, quinine, salicylates, sulfinpyrazone), as a result of which their concentration in the blood plasma may increase .
Cephalosporins
With the simultaneous administration of cephalosporins (for example, cefixime) and nifedipine in probands, the bioavailability of the cephalosporin increased by 70%. Pharmacodynamic interactions
Blood pressure lowering drugs
The antihypertensive effect of nifedipine may be enhanced when used simultaneously with antihypertensive drugs, such as diuretics, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists (ARI), other BMCCs, alpha-blockers, phosphodiesterase-5 inhibitors, methyldopa.
When using nifedipine and beta-blockers simultaneously, it is necessary to carefully monitor the patient's condition, since in some cases the course of chronic heart failure may worsen.
The severity of the decrease in blood pressure increases with the simultaneous use of inhalational anesthetics and tricyclic antidepressants.
Nitrates
When used simultaneously with nitrates, tachycardia increases.
Antiarrhythmic drugs
BMCCs can enhance the negative inotropic effect of antiarrhythmic drugs such as amiodarone and quinidine. Nifedipine should be co-administered with disopyramide and flecainide with caution due to a possible increase in negative inotropic effect.
Magnesium sulfate
It is necessary to carefully monitor blood pressure in pregnant women while using nifedipine with intravenous magnesium sulfate due to the possibility of an excessive decrease in blood pressure, which poses a danger to both the mother and the fetus.
Fentanyl
The simultaneous use of nifedipine and fentanyl can lead to severe arterial hypotension. If possible, it is recommended that nifedipine be discontinued at least 36 hours before fentanyl-based anesthesia.
Calcium preparations
Reduced effectiveness of nifedipine.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs reduce the antihypertensive effect of nifedipine due to suppression of prostaglandin synthesis, as well as sodium and fluid retention in the body.
Sympathomimetics
Sympathomimetic agents reduce the antihypertensive effect of nifedipine.
Estrogens
Estrogens reduce the antihypertensive effect of nifedipine due to fluid retention in the body.
Lithium preparations
When BMCC is used together with lithium drugs, it is possible to increase the manifestation of the neurotoxicity of the latter (nausea, vomiting, diarrhea, ataxia, tremor, tinnitus).
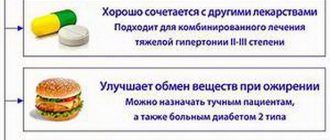
Indications for use and dosage
Indications for the use of Corintar are the following diseases:
- chronic sore throat;
- hypertension;
- Prinzmetal oil seal.
The dosage of the drug is determined in each specific case individually and depends on the course of the disease, the patient’s blood pressure level, tolerability of the drug, the presence of contraindications and other factors.
Instructions for use are prescribed by a doctor; general recommendations must be taken into account.
The drug should be taken only after meals. The tablets should be swallowed without chewing and washed down with plenty of water.
In the acute stage of a hypertensive crisis, 1 or 2 tablets should be placed under the tongue until completely absorbed. This method of using the drug promotes the rapid passage of the active substance into the bloodstream and its effect on the body.
In some situations, the following usage patterns are recommended:
- Chronic angina requires the use of 1 tablet at a dose of 10 milligrams. Corinfar should be taken at least 3 times a day. In the absence of a therapeutic effect, it is allowed to increase the dose by 2 times, but not more than 4 tablets per day.
- For essential hypertension, it is recommended to take 1 tablet 3 times a day. In the absence of therapeutic effects, it is allowed to increase the dose to 2 tablets per 1 dose. However, it is not recommended to take more than 4 pieces during the day. The interval between taking the drug should be at least 4 hours.
Corinfar Retard is recommended to be used no more than 2 times a day, 1 tablet. Only in emergency cases can you take 2 tablets at a time.
Corintar Uno is prescribed 1 tablet after breakfast. The maximum dose of Corintar Uno can reach 80 milligrams during the day.
The duration of the therapeutic course is determined in each case individually by the attending physician.
If the patient has severe liver failure, the dose of the drug should be adjusted.
Features of taking medicine by children and pregnant women
The drug can be prescribed to pregnant women if pregnancy is complicated by chronic arterial hypertension or toxemia in late pregnancy.
To avoid the risk of premature birth, it is not recommended to prescribe Corinfar before 18 weeks of pregnancy. Experience with prescribing to pregnant women indicates that the vast majority of patients have been well tolerated. The specialists did not notice any complications.
The duration of the course of treatment should not exceed 14 days. During this time, the pregnant woman's condition should be constantly monitored.
During the breastfeeding period, the use of Corinfara is contraindicated, since the active substance will be excreted from milk. Therefore, if the drug is indicated, breastfeeding should be discontinued.
Use by children
The effectiveness and safety of Corinfar in children have not been established, so it should be taken in children only when necessary and under the strict supervision of a physician.
Corinfar® retard
Pharmacokinetic interactions
Medicines that affect the metabolism of nifedipine
Nifedipine is metabolized by CYP3A4/5 isoenzymes, which are located in the intestinal mucosa and liver. Drugs that inhibit or induce this enzyme system may affect the first pass effect through the liver (after oral administration) or the clearance of nifedipine.
Inducers of the CYP3A4 isoenzyme
Rifampicin
Rifampin is a potent inducer of the CYP3A4 isoenzyme. When used simultaneously with rifampicin, the bioavailability of nifedipine is significantly reduced and, accordingly, its effectiveness is reduced. Therefore, the simultaneous use of nifedipine with rifampicin is contraindicated.
Antiepileptic drugs that induce CYP3A4 (eg, phenytoin, carbamazepine, phenobarbital)
Phenytoin induces the CYP3A4 isoenzyme. With the simultaneous use of nifedipine and phenytoin, the bioavailability of nifedipine is reduced and its effectiveness is reduced. When using this combination simultaneously, it is necessary to monitor the clinical response to nifedipine therapy and, if necessary, increase its dose. If the dose of nifedipine is increased with simultaneous use of both drugs, the dose of nifedipine should be reduced after discontinuation of phenytoin.
Clinical studies examining the potential interaction between nifedipine and carbamazepine or phenobarbital have not been conducted. Since both drugs reduce the concentration of nimodipine in the blood plasma, which is structurally similar to BMCC, the possibility of a decrease in the concentration of nimodipine in the blood plasma and a decrease in its effectiveness cannot be excluded.
CYP3A4 isoenzyme inhibitors
Macrolide antibiotics (for example, erythromycin)
Clinical studies on the interaction of nifedipine and macrolide antibiotics have not been conducted. Some macrolides are known to inhibit the CYP3A4 isoenzyme. As a result, the possibility of an increase in the concentration of nifedipine in the blood plasma cannot be excluded with the simultaneous use of nifedipine and macrolide antibiotics.
Azithromycin, a macrolide antibiotic, does not inhibit the CYP3A4 isoenzyme.
HIV protease inhibitors (eg, ritonavir)
Clinical studies examining the interaction of nifedipine and HIV protease inhibitors have not been conducted. It is known that drugs of this class inhibit the CYP3A4 isoenzyme. In addition, drugs of this class have been shown to suppress the metabolism of nifedipine mediated by the CYP3A4 isoenzyme in vitro.
When used simultaneously with nifedipine, a significant increase in the concentration of nifedipine in the blood plasma cannot be ruled out due to a decrease in the effect of “first pass” through the liver and slower elimination.
Azole antifungals (eg, ketoconazole)
Clinical studies examining the interaction of nifedipine and azole antifungals have not been conducted. It is known that drugs of this class inhibit the CYP3A4 isoenzyme. When used simultaneously with nifedipine, a significant increase in the systemic bioavailability of nifedipine is possible by reducing the effect of “first pass” through the liver.
Cimetidine and ranitidine
It has been established that cimetidine and ranitidine inhibit the CYP3A4 isoenzyme and cause an increase in the concentration of nifedipine in the blood plasma (by 80% and 70%, respectively), thereby enhancing its antihypertensive effect.
Diltiazem
Diltiazem reduces the clearance of nifedipine. This combination should be used with caution. A dose reduction of nifedipine may be required.
Fluoxetine
Clinical studies examining the interaction of nifedipine and fluoxetine have not been conducted. It is known that fluoxetine in vitro
suppresses the metabolism of nifedipine mediated by the action of the CYP3A4 isoenzyme. Therefore, the possibility of an increase in the concentration of nifedipine in the blood plasma cannot be excluded with the simultaneous use of nifedipine and fluoxetine.
Nefazodone
Clinical studies examining the interaction between nifedipine and nefazodone have not been conducted. Nefazodone is known to inhibit the metabolism of other drugs mediated by the CYP3A4 isoenzyme. Therefore, the possibility of increased plasma concentrations of nifedipine cannot be excluded with simultaneous use of nifedipine and nefazodone.
Quinidine
Increased plasma concentrations of nifedipine have been reported when administered concomitantly with quinidine. Therefore, careful monitoring of blood pressure is necessary when using quinidine and nifedipine simultaneously. If necessary, the dose of nifedipine should be reduced.
Quinupristin/dalfopristip
Concomitant use of quinupristin/dalfopristin may lead to increased plasma concentrations of nifedipine.
Valproic acid
Clinical studies examining the interaction of nifedipine and valproic acid have not been conducted. Since valproic acid increases the concentration of nimodipine in the blood plasma, which is structurally similar to BMCC, the possibility of increasing the concentration of nifedipine in the blood plasma and enhancing its effectiveness cannot be excluded.
Grapefruit juice
Grapefruit juice inhibits the CYP3A4 isoenzyme and suppresses the metabolism of nifedipine. The simultaneous use of the drug with grapefruit juice leads to an increase in the concentration of nifedipine in the blood plasma and a prolongation of its action due to a decrease in the “first pass” effect through the liver and a decrease in clearance. This may enhance the antihypertensive effect of nifedipine. With regular consumption of grapefruit juice, this effect can last for 3 days after the last consumption of the juice. Consumption of grapefruit/grapefruit juice during treatment with nifedipine is contraindicated.
CYP3A4 isoenzyme substrates
Substrates of the CYP3A4 isoenzyme (for example, cisapride, tacrolimus, benzodiazepines, imipramine, propafenone, terfenadine, warfarin), when used simultaneously with nifedipine, may act as CYP3A4 inhibitors and increase the concentration of nifedipine in the blood plasma.
Cisapride
Concomitant use of cisapride and nifedipine may lead to increased plasma concentrations of nifedipine.
Effect of nifedipine on other drugs
Quinidine
Nifedipine causes a decrease in the concentration of quinidine in the blood plasma. After discontinuation of nifedipine, a sharp increase in the concentration of quinidine in the blood plasma may occur. Therefore, when using nifedipine as additional therapy or discontinuing nifedipine, the concentration of quinidine in the blood plasma should be monitored and, if necessary, its dose should be adjusted.
Digoxin
The simultaneous use of nifedipine and digoxin may lead to a decrease in the clearance of digoxin and, consequently, to an increase in the concentration of digoxin in the blood plasma. The patient should be carefully monitored for symptoms of glycoside overdose and, if necessary, reduce the dose of digoxin, taking into account its concentration in the blood plasma.
Theophylline
Nifedipine increases the concentration of theophylline in the blood plasma, and therefore the concentration of theophylline in the blood plasma should be monitored. The clinical effect of both drugs when used together does not change.
Tacrolimus
Tacrolimus is metabolized via the CYP3A4 isoenzyme. Recently published data indicate the possibility of increased tacrolimus concentrations in selected cases when administered concomitantly with nifedipine. When using tacrolimus and nifedipine simultaneously, the concentration of tacrolimus in the blood plasma should be monitored and, if necessary, its dose should be reduced.
Vincristine
Nifedipine slows down the elimination of vincristine from the body and may cause increased side effects of vincristine. If simultaneous use is necessary, reduce the dose of vincristine.
Drugs that bind to blood proteins
Nifedipine can displace drugs characterized by a high degree of binding from protein binding (including indirect anticoagulants - coumarin and indanedione derivatives, anticonvulsants, non-steroidal anti-inflammatory drugs, quinine, salicylates, sulfinpyrazone), as a result of which their concentration in the blood plasma may increase .
Cephalosporins
With the simultaneous administration of cephalosporins (for example, cefixime) and nifedipine in probands, the bioavailability of the cephalosporin increased by 70%.
Pharmacodynamic interactions
Medicines that lower blood pressure
The antihypertensive effect of nifedipine may be enhanced when used simultaneously with antihypertensive drugs, such as: diuretics, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists (ARA II), other BMCCs, alpha-blockers, phosphodiesterase-5 inhibitors, methyldopa .
When using nifedipine and beta-blockers simultaneously, it is necessary to carefully monitor the patient's condition, since in some cases the course of chronic heart failure may worsen.
The severity of the decrease in blood pressure increases with the simultaneous use of inhalational anesthetics and tricyclic antidepressants.
Nitrates
When used simultaneously with nitrates, tachycardia increases.
Antiarrhythmic drugs
ICHCs may enhance the negative inotropic effects of antiarrhythmic drugs such as amiodarone and quinidine. Nifedipine should be co-administered with disopyramide and flecainide with caution due to a possible increase in negative inotropic effect.
Magnesium sulfate
It is necessary to carefully monitor blood pressure in pregnant women while using nifedipine with intravenous magnesium sulfate due to the possibility of an excessive decrease in blood pressure, which poses a danger to both the mother and the fetus.
Fentanyl
The simultaneous use of nifedipine and fentanyl can lead to severe arterial hypotension. If possible, it is recommended that nifedipine be discontinued at least 36 hours before fentanyl-based anesthesia.
Calcium preparations
Reduced effectiveness of nifedipine.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs reduce the antihypertensive effect of nifedipine due to suppression of prostaglandin synthesis, as well as sodium and fluid retention in the body.
Syptomimetics
Sympathomimetic agents reduce the antihypertensive effect of nifedipine.
Estrogens
Estrogens reduce the antihypertensive effect of nifedipine due to fluid retention in the body.
Lithium preparations
When BMCC is used together with lithium drugs, it is possible to increase the manifestation of the neurotoxicity of the latter (nausea, vomiting, diarrhea, ataxia, tremor, tinnitus).
Side effects and contraindications
Side effects on the body can be expressed as follows:
- The occurrence of nausea or severe, unloaded vomiting;
- Drug-induced hepatitis;
- Feeling of pulling on the right under the ribs;
- increased serum transciplinase concentration;
- tightening of the chest tuft;
- Autumn;
- tachycardia;
- Disposal rash;
- peripheral edema;
- Cramps in the limbs;
- Paresthesia;
- thrombocytopenia;
- dizziness, headaches;
- Decrease in the number of leukocytes.
Contraindications for using Corinfar include:
- Individual intolerance to the components of the drug;
- Cardiogenic shock of various origins;
- Recurrent attacks of unstable thoracic transmission;
- 4 weeks after a major myocardial infarction;
- First 8 weeks of pregnancy;
- lactation;
- Aortic stenosis;
- renal failure, liver;
- hemodialysis;
- hypotension;
- Heart failure of a chronic nature.
Corinfar, 100 pcs., 10 mg, extended-release film-coated tablets
During the treatment period it is necessary to refrain from taking ethanol.
It is recommended to stop treatment with the drug gradually.
It should be borne in mind that angina pectoris may occur at the beginning of treatment, especially after recent abrupt withdrawal of beta-blockers (the latter should be withdrawn gradually).
The simultaneous administration of beta-blockers must be carried out under conditions of careful medical supervision, as this may cause an excessive decrease in blood pressure, and in some cases, aggravation of symptoms of heart failure.
In case of severe heart failure, the drug is dosed with great caution.
Diagnostic criteria for prescribing the drug for vasospastic angina are: a classic clinical picture, accompanied by an increase in the ST segment, the occurrence of ergonovine-induced angina or coronary artery spasm, detection of coronary spasm during angiography or identification of an angiospastic component without confirmation (for example, with a different voltage threshold or with unstable angina, when data ECGs indicate transient vasospasm).
For patients with severe obstructive cardiomyopathy, there is a risk of increased frequency, severity and duration of angina attacks after taking nifedipine; in this case, discontinuation of the drug is necessary.
In patients with irreversible renal failure who are on hemodialysis, have high blood pressure and a reduced total blood volume, the drug should be used with caution, as a sharp drop in blood pressure is possible. Patients with impaired liver function are closely monitored; if necessary, reduce the dose of the drug and/or use other dosage forms of nifedipine.
If surgery under general anesthesia is necessary, the anesthesiologist must be informed about the patient's treatment with nifedipine.
During in vitro fertilization, in some cases, BMCC cause changes in the head part of the sperm, which can lead to dysfunction of the sperm. In cases in which repeated in vitro fertilization has not been carried out for an unclear reason, the use of BMCC, including nifedipine, can be considered a possible reason for failure.
During treatment, it is possible to obtain a false positive result from the direct Coombs test and laboratory tests for antinuclear antibodies. In the spectrophotometric determination of vanillylmandelic acid in urine, nifedipine may cause a falsely elevated result, however, nifedipine does not affect the results of tests performed using high-performance liquid chromatography.
Caution should be exercised during simultaneous treatment with nifedipine, disopyramide and flecainamide due to a possible increase in inotropic effect.
Impact on the ability to drive a car and other mechanisms
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
What can be replaced
Corinfar can be replaced with drugs such as Osmo-Adalat, Cordipin, calcigar, adalat. The basis of each of these drugs is the same active substance - nifedipine, so the effect of these drugs on the patient's body is the same. Pharmacological products differ only in price and manufacturer.
If you are not intolerant to Nifedipine, the drug can be replaced with the following drugs: Concount, Co-Diovan, CaptoPril, Amprilan. These drugs are also intended to lower blood pressure, but their active ingredient is a different substance.