In a healthy body, blood circulates freely. The arterial and venous systems, which are found throughout the body, including the central nervous system (CNS), are responsible for this. To ensure proper functioning of the central nervous system, both sufficient arterial inflow, which ensures the delivery of oxygen and nutrients necessary for the proper functioning of the brain, and venous outflow, which removes metabolic products from the central nervous system, are important. Metabolism in the nervous system is much faster than in most tissues of the body. Therefore, ensuring proper and sufficient blood flow is important for health.
What kind of pathology is this
The disease is accompanied by a slowdown in the speed of blood flow in the brain. Occurs due to outflow disturbances on the way to the heart.
Short-term impairment occurs in every person. For example, when coughing, physical activity, or sharply turning the head. This causes a dull headache.
Venous congestion of cerebral vessels is accompanied by severe disruption of blood flow from the brain through the central nervous system to the myocardium. Slow blood circulation leads to blood stagnation.
Against this background, various pathologies develop. In patients with this disease, venous congestion occurs in the head, and the general outflow is disrupted. The vessels are not saturated with oxygen and useful components.
This leads to their rapid defeat and decreased tone.
Violation of venous circulation in the brain
The brain is a complex structure, its normal functioning depends on the state of blood circulation. In addition to the need to deliver oxygen and glucose to the nervous tissue, the outflow of venous blood and the removal of toxins with it, the result of cell activity, is important. If this process is disrupted, chronic venous insufficiency of the brain is formed.
A peculiarity of the vessels of the brain is the course of the veins: it does not coincide with the direction of the arteries, and a network is formed that is independent of them. If the outflow of blood through one of the vessels is impaired, venous blood is directed to the other, and compensatory expansion occurs. A prolonged decrease in tone leads to vascular atrophy, they collapse, and the risk of thrombosis increases. Dilated vessels contribute to the development of venous circulation insufficiency, the functioning of the valves is disrupted, they do not close tightly, and the direction of blood flow is disrupted.
Stages of the pathological process
The following stages are distinguished during cerebral venous insufficiency:
- latent: no clinical symptoms, no complaints;
- cerebral venous dystonia: some symptoms are observed: headaches, weakness;
- venous encephalopathy: severe symptoms caused by organic lesions are observed, venous outflow is impaired in all areas of the brain, there is a high risk of hemorrhages from dilated vessels.
Classification
There are chronic and acute variants of venous circulation in the brain. Chronic include venous congestion and venous encephalopathy, acute include venous hemorrhage, thrombosis of the veins and venous sinuses, thrombophlebitis.
Causes and risk factors
Insufficiency of cerebral venous circulation can be caused by diseases or individual characteristics of the patient. The most common causes of pathology:
- neoplasms in brain tissue can cause disruption of venous outflow;
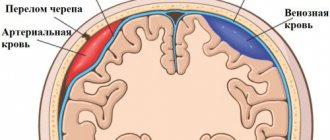
- head injuries that impair blood circulation to the brain;
- injuries during childbirth;
- hematomas formed as a result of stroke, atherosclerosis, bruises and other causes contribute to the formation of tissue edema, which complicates the outflow of blood from the affected area;
- blood clots and embolisms narrow the lumen of the vessel or completely close it, preventing the movement of blood;
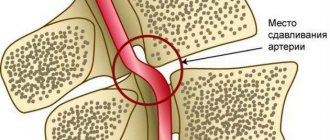
- diseases of the spinal column, in which deformed sections of the canals compress the vessels and disrupt blood flow, also cause venous insufficiency;
- vascular features: hereditary predisposition and impaired development of veins can provoke the development of a violation of the outflow of venous blood.
Circulatory disorders can be physiological and occur when coughing, sneezing, or physical strain. Such short-term deviations do not cause significant harm to health.
One-time attacks of cerebral circulatory disorders do not cause serious consequences for the body. However, prolonged blood stagnation can contribute to the development of serious consequences. The following risk factors increase the likelihood of cerebral venous insufficiency:
- frequent stress;
- smoking;
- alcohol abuse;
- prolonged dry cough;
- professional singing;
- hypertension;
- heart failure;
- reading in the wrong position
- professional swimming;
- frequent wearing of clothes that compress the neck;
- chronic rhinitis:
- work in high-altitude, underwater, underground professions;
- office work that involves staying in a position with the head tilted or turned;
- frequent physical activity of high intensity
Clinical manifestations
Disturbances of venous circulation, as a rule, are genetically determined. Currently, the role of the initial tone of the veins in the formation of venous discirculation is undeniable. Constitutional and hereditary factors are key for the development of venous dyshemia. Patients with a family “venous” history usually have several typical manifestations of constitutional venous insufficiency - varicose veins or phlebothrombosis of the lower extremities, hemorrhoids, varicocele, impaired venous outflow from the cranial cavity, esophageal varicose veins. Pregnancy is often the trigger.
Typical complaints:
- morning or afternoon headache of varying intensity;
- dizziness, depending on changes in body position;
- noise in the head or ears;
- visual disturbances (decreased visual acuity, photopsia);
- “tight collar” symptom - increased symptoms when wearing tight collars or ties;
- “high pillow” symptom - increased symptoms when sleeping with a low headboard;
- sleep disorders;
- feeling of discomfort, “fatigue” in the eyes in the morning (symptom of “sand in the eyes”);
- pastiness of the face and eyelids in the morning (with a pale, purple-cyanotic tint);
- mild nasal congestion (outside the symptoms of acute respiratory infections);
- darkening of the eyes, fainting;
- numbness of the limbs.
Signs of impaired cerebral venous blood flow are related to weather conditions. Headaches are poorly controlled by analgesics; often some relief is brought only by a change in body position - in a horizontal position, venous blood flow is redirected along collaterals - bypassing the affected vessel.
The patient’s psyche changes in such a way that minor experiences can lead to neuroses. Tearfulness increases, the patient often breaks into a scream. Mania and depression are observed. Severe damage leads to psychosis, accompanied by hallucinations and delusions; this can make the patient dangerous to himself and others.
Diagnostics:
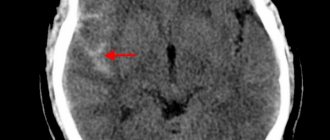
- radiography determines the strengthening of the pattern of the veins of the skull, which indicates the presence of a pathological process;
- angiography is a contrast method for diagnosing blood stagnation, determining the patency of blood vessels;
- computed tomography and magnetic resonance imaging make it possible to accurately determine the presence of a pathological process in the brain, as well as in surrounding tissues;
- ultrasound examination of the veins of the brain and neck;
- rheoencephalography is a functional diagnostic method that assesses the condition of blood vessels;
- An increased level of pressure in the ulnar vein allows one to suspect abnormalities in the vessels of the brain.
Therapy is complex and includes several areas
- drug treatment;
- non-drug treatment: physiotherapy, massage, physical therapy;
- surgery.
Drug therapy
The following drugs are used to normalize cerebral circulation:
- venotonics strengthen the vascular wall, reduce permeability, have an analgesic effect, and eliminate inflammation;
- diuretics to eliminate swelling;
- neuroprotectors improve nutrition and metabolism of the brain;
- anticoagulants to thin the blood and prevent thrombosis;
- vitamin therapy (vitamins B and PP).
Non-drug treatment
There are a number of non-drug therapies that are effective as an additional treatment method and improve vascular tone. However, before treating impaired cerebral venous outflow with their help, it is necessary to assess individual risks and contraindications: in some cases, such procedures can lead to the opposite effect and worsen the patient’s condition.
Applicable:
- head and neck massage;
- oxygen therapy;
- foot baths;
- physical therapy: breathing exercises, neck exercises, yoga classes.
Intern of the ophthalmology department Gurlo A.I.
Head of the department ophthalmological department Rudova
Types and classification
It has three main subspecies:
- dyshemia of the central brain;
- vertebral plexuses;
- dyshemia of the ICA basin.
The classification of the disease has 3 stages of development.
- Latent. Not accompanied by severe symptoms. A person does not observe deviations and does not suspect the development of such a pathology.
- Cerebrovenous discirculation. Symptoms appear, but do not affect the person’s normal life.
- Venous encephalopathy. Clinical manifestations cause discomfort to the patient. It is at this stage that pathology is usually diagnosed.
In addition, the disease is determined by its form of development. The primary form is accompanied by circulatory disorders that arise due to changes in venous tone.
The stagnant form is accompanied by the following symptoms: problems with blood outflow from the brain of mechanical etiology. In this case, surgical intervention cannot be avoided.
Diseases that can provoke the development of pathology
There are a number of diseases that can provoke the appearance of venous dysgemia in a child:
- Stenosis. A characteristic phenomenon of pathology is vasoconstriction, due to which the veins gradually begin to collapse. As a result, the natural process of blood outflow is disrupted, and vein blockage develops. It is incredibly difficult to identify the problem, since narrowing of blood vessels by less than half does not give any unpleasant symptoms.
- Deformation of organs that impede normal blood flow, pinching of valves or bridges. In such a situation, the direction of blood flow may be changed. It happens that a child is already born with an abnormal structure of the venous system - complete or partial closure of blood vessels.
- Even diseases completely unrelated to the blood flow can provoke venous dysgemia - problems in the spine, the presence of cancerous tumors, or previous trauma suffered by the child.
- Not the last place on the list is occupied by bad habits - overeating, teenage smoking, drinking alcoholic beverages.
- Osteochondrosis, as well as pathologies of the thyroid gland, are not the cause of improper venous outflow. These problems become a consequence of such a problem.
Symptoms of venous dysgemia sometimes appear immediately after the baby is born due to problems that appear during the perinatal period of fetal development.
Causes
Occurs for the following reasons:
- traumatic brain injuries, which are accompanied by internal hematomas and bone fractures;
- cerebral edema due to stroke;
- tumors;
- disruption of the development of the venous network;
- neoplasms in the cervical spine;
- congestion in the veins;
- injuries in the peritoneum or thoracic region;
- osteochondrosis, prolapsed discs.
Circulatory disorders are associated with direct and indirect causes.
Mechanism of disease development and localization
The difficulty may be due to the influence of physiological factors:
- when straining;
- chronic cough;
- singing;
- playing wind musical instruments;
- tilting the head during exercise;
- incorrect position of the head and neck during sleep.
The mechanism of development of the disorder is associated with a violation of the outflow of blood from the brain when the main, extracranial, and intracranial pathways are damaged. Also if stagnation occurs in the small circulation. The pathology is localized in any part of the brain.
Anatomical features
To understand the disease, it is important to understand the anatomy. Knowing the features of the structure of all parts of the head, both hemispheres of the brain and blood vessels, it will become easier to even identify this disease.
The venous wall of the brain does not have a valve apparatus, which is why the blood disperses freely through all adjacent vessels on different sides of the head. Almost all of them are located at a distance from each other and from the arteries. Venous sinuses are intermediate points for blood with cerebrospinal fluid from the ventricles. Vessels emerge from them. They come in two types: superficial and deep. The first are located inside the pia mater in the interlobar grooves; they are responsible for the flow of blood from the cerebral cortex to the cerebellum. The latter are formed due to the white matter with subcortical nodes.
Diploic and emissary veins are also distinguished, which conduct blood flow to the sinuses and are responsible for the connection between the superficial and deep vessels. There are also extracranial veins that provide blood supply to certain areas of the brain. In this case, all the vessels are intertwined into one, called a tank. Through it, blood flows to the central part of the brain, many sinuses and the basal plexus.
For the stable functioning of blood circulation, intervenous and intersinus anastomoses are of great importance. At the exit from the brain near the neck, three plexuses are formed: the foramen ovale of the skull, the canals of the hypoglossal nerve and the carotid artery.
Possible complications
The presence of such a pathology negatively affects the health and condition of the body as a whole. This is associated with a constant risk of complications. The main ones include:
- stroke;
- cerebral infarction;
- encephalopathy.
Any of these conditions can cause irreparable consequences. The disease also often leads to the development of thrombosis.
Manifestations
Signs of venous discirculation can be varied. Initially, a mild headache appears, which intensifies over time. Then it becomes stable.
Discomfort appears in a certain area - the temples, the crown of the head, the back of the head. Such manifestations require immediate medical attention.
Heaviness in the head leads to a decrease in the clarity of speech, the ability to think and learn is impaired. This often disrupts orientation in space.
If the disease is ignored in the initial stage, the symptoms will appear more pronounced and severe. Headaches will become constant, especially in the morning. With a sharp turn of the head or prolonged physical activity, the pain may intensify.
Characteristic symptoms of venous stagnation in the head:
- severe headache when blood pressure changes;
- increased body temperature;
- increased or onset of pain when turning the head sharply;
- chills;
- nausea;
- numbness in the limbs;
- dizziness;
- vomit.
If the disease is severe, nerve cells are quickly damaged. The patient may be diagnosed with neurological and psychological disorders.
In childhood, symptoms are the same as in adults.
The main manifestations of a severe form of pathology:
- paralysis;
- paresis;
- disorders of the musculoskeletal system;
- decreased sensitivity;
- pain in some parts of the body;
- convulsions;
- speech disorder;
- loss of ability to read, write;
- the occurrence of epilepsy attacks;
- impaired coordination and orientation in space.
Any signs may appear in varying degrees of severity. It all depends on dysfunction of the brain due to a lack of oxygen and nutrients.
Every patient who suffers from this disease is faced with the occurrence of aggression and excessive irritability. You can observe a change in habits and preferences. Interest in hobbies is often lost.
Patients with such disorders generally deteriorate. The condition is accompanied by processes that lead to the gradual death of brain cells. They are usually involved and responsible for vital processes.
Symptoms
The first and main sign of a problem is the occurrence of acute pain where the blood outflow is blocked. Such points can be easily identified through palpation on the chest, neck, shoulders and head. Painful discomfort is caused by the fact that stagnant blood gradually destroys the tissues surrounding it, trying to “break through” the road.
Children's venous dysgemia is often accompanied by dizziness and spontaneous headaches. The baby often has a fever, causing a sharp increase in temperature. In an advanced state, the severity of symptoms is much more serious, it is manifested by the following parameters:
- violation of natural coordination of movement;
- dysfunction of the main sensory organs;
- performing involuntary movements;
- development of complete or partial paralysis;
- convulsions;
- nosebleeds;
- constant sensations of pain;
- impaired motor skills, slurred speech.
At the very beginning of the development of the disease, it practically does not manifest itself at all. Only sometimes the child complains of short-term impairment of motor coordination and headaches. In addition, venous problems cause metabolic disorders and lack of oxygen. These disruptions provoke constant chills, surges in blood pressure, and the limbs periodically go numb.
Diagnostics
It is very difficult to detect difficulty in the venous outflow of the brain in the initial stage. Diagnosis in most cases is accidental, during routine or preventive examinations. Signs of the severe stage are similar to other pathologies.
To establish a diagnosis, the following methods are used:
- MRI;
- triplex scanning;
- Doppler ultrasound.
The doctor must examine the patient's medical history to rule out disorders that could lead to the development of this disease.
Treatment
In the initial stages, it is often possible to do without medications, with the help of additional non-drug interventions. It is possible to prescribe physiotherapeutic procedures, osteopathy, reflexology. The results of treatment are assessed using ultrasound.
But the first step that needs to be taken to treat a violation of venous outflow is to consult a neurologist. In case of serious disorders and complications, treatment begins with drug therapy. Restoration of the nervous system, increased vascular tone, and elimination of vein compression are required. Treatment with medications is carried out in parallel with non-drug treatment. Therefore, in parallel, the patient is prescribed a visit to an osteopath and physiotherapy sessions.
Treatment continues until the problem is resolved. This may take several weeks or months depending on the severity of the disease and the individual characteristics of the body.