A blood test for biochemistry is the most frequently prescribed test in gynecology, urology, endocrinology, oncology, dermatology and surgery. If you correctly decipher the information received, you can quickly diagnose diseases and metabolic disorders, even in cases where they do not give clear symptoms. It’s not for nothing that doctors call a biochemical blood test “truth serum.”
The cost of a comprehensive biochemical analysis is 1,510 rubles. The analysis includes determination of ALT, AST, glucose, serum creatinine (with determination of GFR), urea, total protein, total bilirubin, total cholesterol. CONSULTATION WITH DOCTORS ON THE RESULTS OF ULTRASOUND AND ANALYSIS - 500 rubles. (optional)
CLICK TO SIGN UP
To ensure that the analysis results are truly useful, we recommend that you read this article before going to the laboratory.
What is a biochemical analysis and why is it prescribed?
The content of the article
Biochemical blood testing is the most important diagnostic measure, which makes it possible to obtain an accurate assessment of lipid, protein and carbohydrate metabolism. These indicators are important for a huge number of pathologies and diseases, and therefore blood biochemistry is considered one of the basic tests of laboratory diagnostics.
The content of biochemical substances is assessed by their concentration, which is compared with normal values. If the concentration of a particular factor deviates from the norm, conclusions are drawn about the likelihood of a particular disease.
Preparing for blood collection
A biochemical blood test, like any other, requires simple preparation. These measures must be taken very carefully, since any violation will affect the properties and composition of the blood. Conditions for accurate results:
- Have a low-fat dinner the night before donating blood, and do not drink coffee or strong tea. Immediately before donating blood in the morning, do not eat anything, you can only drink water.
- A day before the appointed date, refrain from visiting the bathhouse or sauna and do not overwork yourself.
- Donate blood for biochemistry before other procedures, if any have been prescribed (x-rays, injections, IVs, massage).
- To determine your sugar level most accurately, do not drink coffee in the morning or even brush your teeth.
- If you are taking medications that reduce lipid (fat) concentrations, you should stop taking them two weeks before the test, if possible.
- Limit the use of hormones, antibiotics, diuretics and other drugs for a while. The doctor referring you for the procedure will tell you for how long and which tablets will need to be postponed.
If a repeat examination is scheduled, take it in the same laboratory and at approximately the same time. Each laboratory uses its own methods and reagents, so results will vary between laboratories.
Definitive blood tests
These types of blood tests are very different from those listed above in that they do not diagnose any disease or health condition of a person, but simply indicate the peculiarity of his circulatory system. These include tests to determine blood type, Rh factor and coagulation. As a rule, these studies are mandatory for people in special professions, as well as for all pregnant women. Blood is taken for analysis from a vein and does not require special preparation of the patient.
What indicators are most important in a biochemical blood test?
The diagnostic markers of a biochemical blood test are the following indicators:
- Blood glucose
. The most important test demonstrating the functionality and normal functioning of the endocrine system, liver and pancreas. This indicator is the main diagnostic parameter in identifying diabetes mellitus. - Total bilirubin
. This substance is a pigment that is formed as a result of the destruction of hemoglobin. This happens with the active destruction of red blood cells, with disruption of the liver (jaundice, cirrhosis), as well as as a result of disturbances in the outflow of bile. - Direct and indirect bilirubin. This indicator represents a separate fraction of the total bilirubin level and increases with disturbances of bile outflow, which is primarily characteristic of jaundice. The difference between the values of total bilirubin and the fraction of direct bilirubin is called an indirect indicator.
- AST (AST) and ALT (ALT)
- these indicators are enzymes, the main place of production of which is liver cells. That is why an increase in the concentration of these substances in the blood may indicate destructive processes in the liver, heart and other internal organs. - Gamma-GT
(gamma-glutamyltransferase) is an enzyme whose increased concentration indicates pathology of the liver or pancreas. Alkaline phosphatase is another enzymatic factor that is normally detected in the blood in small quantities. An increase in alkaline phosphatase levels indicates diseases of the liver and bone structures. - Total cholesterol
is an important indicator that demonstrates liver function and the patient’s nutritional pattern, since this substance enters the body with food. Low-density lipoproteins (LDL) are the most important characteristic that can early signal a high risk of the formation of atherosclerotic plaques in blood vessels. - Triglycerides
are one of the main characteristics of fat metabolism in the body. - Total protein
- demonstrates the overall level of protein components in the blood, and allows you to identify disorders in the liver and the presence of an infectious-inflammatory process.
Also, a biochemical blood test takes into account the level of albumin, potassium, sodium, chlorine, iron, creatinine, uric acid, urea and C-reactive protein.
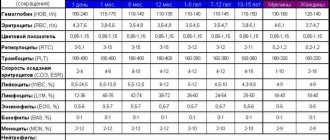
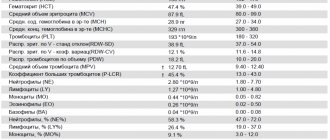
Clinical (general) blood test
It is carried out with the aim of identifying the general picture of the state of blood in the human body, including helping in the diagnosis of various infectious and hematological diseases. Blood sampling from a person must be done on an empty stomach from a finger and does not require special preparation from the patient. During the analysis, the number of red blood cells, leukocytes, platelets, hemoglobin is counted, and the erythrocyte sedimentation rate is calculated. There are certain standards according to which any deviation from the required number of blood cells will be considered a sign of some kind of inflammatory process in the body or a serious disease, so the results of such an analysis will depend on whether the blood cell counts are normal or not.
In addition, you need to take into account that each laboratory has its own “standards” for a general (clinical) blood test, so it is better to ask your doctor all your questions.
A general blood test helps a doctor of any specialty. Based on the results of a blood test (hemogram), the doctor can competently assess the condition of the body, make a preliminary diagnosis and promptly prescribe appropriate treatment.
Norms of blood parameters
| Blood indicator | Normal values |
| Hemoglobin, g/l Men Women | 130,0-160,0 120,0-140,0 |
| Red blood cells (RBC), *1012/l Men Women | 4,0-5,0 3,9-4,7 |
| Hematocrit, % Men Women | 40-48 36-42 |
| Average hemoglobin content in erythrocytes (MCH), pg | 27,0-31,0 |
| Mean erythrocyte volume (MCV), fl, µm3 | 80,0-100,0 |
| Mean erythrocyte hemoglobin concentration (MCHC), g/dL | 30,0-38,0 |
| Red blood cell distribution width by volume (RDW-CV), % | 11,5-14,5 |
| Reticulocytes, ‰ (or%) | 2,0-12,0 (0,2-1,2) |
| Leukocytes, *109/l | 4,0-9,0 |
| Neutrophils, % (109/l) Bands Segmented | 1,0-6,0 (0,04-0,30) 47,0-72,0 (2,0-5,5) |
| Eosinophils | 0,5-5,0 (0,02-0,3) |
| Basophils | 0-1,0 (0-0,065) |
| Lymphocytes | 19,0-37,0 (1,2-3,0) |
| Monocytes | 3,0-11,0 (0,09-0,6) |
| Platelets, *109/l | 180,0-320,0 |
| Mean platelet volume (MPV), fl | 7,4-10,4 |
| Platelet distribution width by volume, (PDW), % | 10-20 |
| Thrombocrit (PCT), % | 0,15-0,40 |
| Erythrocyte sedimentation rate (ESR), mm/h | 2,0-20,0 |
How to take a general blood test and what is needed for this?
There are no complex, strict regulations regarding this testing, but there are some rules:
- For this examination, capillary blood is used, which is taken from a finger. Less often, according to the doctor's instructions, blood from a vein can be used.
- The analysis is carried out in the morning. The patient is prohibited from consuming food or water 4 hours before taking a blood sample.
- The main medical supplies used for drawing blood are a scarifier, cotton wool, and alcohol.
What does a general blood test show?
A general (clinical) blood test shows:
- number of red blood cells,
- erythrocyte sedimentation rate (ESR),
- hemoglobin content,
- number of leukocytes,
- leukocyte formula
- and other indicators, each of which we will dwell on in detail.
blood cells are also known as red blood cells. In humans, 1 mm³ of blood contains 4.5-5 million red blood cells. Red blood cells contain hemoglobin and carry oxygen and carbon dioxide. An increase in the number of red blood cells is a sign of diseases such as leukemia, chronic lung diseases, and congenital heart defects. Anemia (decreased number of red blood cells) can be caused by stress, increased physical activity, and fasting. If you cannot immediately determine the cause of the decrease in the number of red blood cells, then it is better to go to a hematologist and undergo additional examination.
A significant increase in the content of red blood cells may indicate erythremia (one of the blood diseases). In addition, an increase in the number of red blood cells (erythocytosis, polycythemia) is observed in acute poisoning, when due to severe vomiting and diarrhea there is a large deficiency of fluid in the body; with acidosis (due to metabolic disorders during exacerbation of certain diseases); when losing fluid for various reasons (heat, illness, heavy physical activity); with long-term cardiovascular or pulmonary diseases, when the body is not sufficiently supplied with oxygen and increases the number of red blood cells in an attempt to still deliver oxygen to the tissues; or when a person is in the highlands, when he no longer has enough oxygen.
Color index - its normal value for people of any age is 0.85-1.15. The blood color index is an indicator of the degree of saturation of red blood cells with hemoglobin and reflects the relationship between the number of red blood cells and hemoglobin in the blood. When its values differ from the norm, this generally indicates the presence of anemia. In this case, anemia is divided into: - hypochromic - color index less than 0.85; - hyperchromic - color index greater than 1.15.
However, anemia can also be normochromic - when the color indicator remains within the normal range.
Reticulocytes are young forms of red blood cells. Children have more of them, adults have less, because the formation and growth of the body has already been completed. An increase in the number of reticulocytes can be observed in anemia or malaria. A decrease in the number of reticulocytes or their absence is an unfavorable sign in anemia, indicating that the bone marrow has lost the ability to produce red blood cells.
The erythrocyte sedimentation rate (ESR) determines how quickly red blood cells settle in a test tube and separate from the blood plasma. In women, the ESR rate is slightly higher than in men; during pregnancy, the ESR increases. Normally, the ESR value in men does not exceed 10 mm/hour, and in women - 15 mm/hour . The ESR indicator may change depending on various factors, including due to various diseases.
An increase in ESR in a blood test is one of the indicators that makes the doctor assume that the patient has an acute or chronic inflammatory process (pneumonia, osteomyelitis, tuberculosis, syphilis), and an increase in ESR is characteristic of poisoning, myocardial infarction, trauma, bone fractures, anemia, kidney diseases, cancer. It is observed both after operations and as a result of taking certain medications. A decrease in ESR occurs during fasting, with a decrease in muscle mass, and when taking corticosteroids.
Hemoglobin is a complex iron-containing protein found in red blood cells - erythrocytes - of animals and humans, capable of reversibly binding with oxygen, ensuring its transfer to tissues. The normal content of hemoglobin in human blood is considered to be: for men 130-170 g/l, for women 120-150 g/l; in children - 120-140 g/l. Blood hemoglobin is involved in the transport of oxygen and carbon dioxide and maintains pH balance. Therefore, determining hemoglobin is one of the most important tasks of a general blood test.
Low hemoglobin (anemia) can be the result of large blood loss; a decrease in hemoglobin occurs when there is a lack of iron, a necessary material for the construction of hemoglobin. Also, low hemoglobin (anemia) is a consequence of blood diseases and many chronic diseases not associated with them.
A hemoglobin level higher than normal can be an indicator of many blood diseases, and a complete blood count will also show an increase in red blood cells. Increased hemoglobin is typical for people with congenital heart defects and pulmonary heart failure. An increase in hemoglobin can be caused by physiological reasons - in pilots after flights, mountain climbers, after significant physical activity, the hemoglobin level is higher than normal.
Leukocytes are the protectors of our body from foreign components. The blood of an adult contains an average of 4-9x10 9/l leukocytes . White blood cells fight viruses and bacteria and cleanse the blood of dying cells. There are several types of leukocytes (monocytes, lymphocytes, etc.). The leukocyte formula allows you to calculate the content of these forms of leukocytes in the blood.
If leukocytes are found in increased numbers in a blood test, this may mean the presence of viral, fungal or bacterial infections (pneumonia, tonsillitis, sepsis, meningitis, appendicitis, abscess, polyarthritis, pyelonephritis, peritonitis), and also be a sign of poisoning of the body (gout ). Previous burns and injuries, bleeding, postoperative condition of the body, myocardial infarction, lung, kidney or spleen, acute and chronic anemia, malignant tumors - all these “troubles” are accompanied by an increase in the number of blood leukocytes.
In women, a slight increase in leukocytes in the blood is also observed in the period before menstruation, in the second half of pregnancy and during childbirth.
A decrease in the number of white blood cells, which a blood test can show, may be evidence of viral and bacterial infections (influenza, typhoid fever, viral hepatitis, sepsis, measles, malaria, rubella, mumps, AIDS), rheumatoid arthritis, kidney failure, radiation sickness, some forms of leukemia, bone marrow diseases, anaphylactic shock, exhaustion, anemia. A decrease in the number of leukocytes can also be observed while taking certain medications (analgesics, anti-inflammatory drugs).
Platelets - these cells are also called blood plates. They are the smallest blood cells. The main role of platelets is participation in blood clotting processes. In blood vessels, platelets can be located near the walls and in the bloodstream. At rest, platelets have a disc-shaped shape. If necessary, they become like a sphere and form special outgrowths (pseudopodia). With their help, blood platelets can stick to each other or stick to a damaged vascular wall.
A decrease in the number of platelets is observed in women during menstruation and during normal pregnancy, and an increase occurs after physical activity. Also, the number of platelets in the blood has seasonal and daily fluctuations. Typically, platelet monitoring is prescribed when taking certain medications, when a person has burst capillaries for no reason, has frequent nosebleeds, or when being examined for various diseases.
An increase in the number of platelets in the blood (so-called thrombocytosis) occurs during: - inflammatory processes (acute rheumatism, tuberculosis, ulcerative colitis); - acute blood loss; - hemolytic anemia (when red blood cells are destroyed); — conditions after removal of the spleen; - observed during treatment with corticosteroids; - some rarer diseases.
A decrease in the number of platelets (thrombocytopenia) is observed in a number of hereditary diseases, but appears much more often in acquired diseases. The number of platelets decreases with: - severe iron deficiency anemia; - some bacterial and viral infections; - liver diseases; - diseases of the thyroid gland; - the use of a number of medications (vinblastine, chloramphenicol, sulfonamides, etc.); - systemic lupus erythematosus.
Hematocrit is the percentage (percentage) of the total blood volume that is made up of red blood cells. Normally, this figure is 40-48% for men, 36-42% for women.
The volume of red blood cells compared to plasma increases with: - dehydration (dehydration), which happens with toxicosis, diarrhea, vomiting; - congenital heart defects, accompanied by insufficient oxygen supply to the tissues; — a person being in high altitude conditions; - insufficiency of the adrenal cortex.
The volume of red blood cells relative to plasma decreases with blood thinning (hydremia) or with anemia.
Hydremia can be physiological if a person immediately drinks a lot of liquid. After significant blood loss, compensatory hydremia occurs when blood volume is restored. Pathological hydremia develops when water-salt metabolism is disturbed and occurs with glomerulonephritis, acute and chronic renal failure, and with heart failure during the period of swelling.
Blood formula . The study of the leukocyte formula has important diagnostic value, showing characteristic changes in a number of diseases. But these data should always be assessed together with other indicators of the blood system and the general condition of the patient.
For various diseases, a combination of the following signs is looked at: the total number of leukocytes; the presence of a nuclear shift of neutrophils (the so-called “shift according to the formula to the left”, that is, the appearance of young, immature forms of neutrophils in the blood); percentage of individual leukocytes; the presence or absence of degenerative changes in cells.
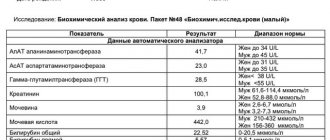
Explanation: normal biochemical blood test indicators in the table
| Index | Norm |
| Albumin | 35-45 g/l |
| Total protein | 63-87 g/l |
| Globulins | 21.2-34.9 g/l |
| Creatinine | 44-97 µmol/l in women and 62-124 µmol/l in men |
| Urea | 2.5-8.3 mmol/l |
| Glucose | 3.5-6.2 mmol/l |
| Uric acid | 0.24-0.54 mmol/l in women and 0.12-0.43 mmol/l in men |
| LDL | up to 3 mmol/l |
| Total cholesterol | 3.3-5.8 mmol/l |
| HDL | from 1.2 mmol/l in women and 1 mmol/l in men |
| Direct bilirubin | 2.2-5.1 µmol/l |
| Total bilirubin | 8.49-20.58 µmol/l |
| Alkaline phosphatase (ALP) | up to 260 units/l |
| Triglycerides | up to 1.7 mmol/l |
| Alanine aminotransferase (ALT) | up to 38 units/l |
| Creatine kinase (CK) | up to 180 units/l |
| Aspartate aminotransferase (AST) | up to 42 units/l |
| Gamma glutamyl transferase (GGT) | up to 33.5 units/l in men and up to 48.6 units/l in women |
| A-amylase | up to 110 units/l |
| Sodium | 130-155 mmol/l |
| Potassium | 3.35-5.35 mmol/l |
Concentration of protein and its fractions in a biochemical blood test
The role of protein (proteins) for the human body is invaluable. This is the main building material in the body, without which new cells, humoral immunity and transfer of substances do not occur. Typically, protein contains at least 20 amino acids; laboratory assistants also detect other elements - lipid residues, carbohydrates, vitamins and substances of inorganic origin (metals).
There are approximately 165 different types of proteins in the blood. The structure and functions of each are individual. However, all proteins can be divided into three groups: fibrinogen, globulins and albumins.
Biochemical analysis reveals two most important conditions:
- Hypoproteinemia
. When the amount of total protein decreases abnormally, we speak of hypoproteinemia. This phenomenon can occur due to poor nutrition (vegetarianism, protein-free diets), excessive blood loss, protein excretion in the urine due to kidney disease, burns, accumulation of large amounts of plasma in the abdomen, treatment with steroid drugs, impaired protein formation, and insufficient absorption of substances. - Hyperproteinemia
. Hyperproteinemia is an increase in the concentration of total protein in the blood. This phenomenon can be absolute and relative. An increase in protein levels due to the loss of the liquid component of blood plasma is considered relative. For example, with cholera and vomiting. An absolute increase in protein concentration is often observed in inflammation and multiple myeloma.
Blood biochemistry: indications for testing
A diagnostic test is required in the following cases:
- The presence of persistent pain in patients in the head, back, muscles, joints, and so on.
- Frequent disruptions in the functioning of the digestive tract: dyspeptic syndrome, heaviness and bloating in the abdomen, belching, difficulty swallowing.
- Respiratory system disorders: shortness of breath, chronic cough syndrome, bronchospasm.
- Pathological symptoms from the cardiovascular system: hypo- or hypertension, chest pain, brady- or tachycardia, coldness of the extremities, heart rhythm disturbances.
- Problems with the urinary system: poly-, oligo- or anuria, nocturia, pain, cramps and other discomfort during urination.
- Weakening of the immune system and frequent ARVI.
- Reproductive function disorders: decreased libido, menstrual irregularities, infertility.
- Hormonal imbalances: constant feeling of thirst, hunger, cold or heat, sudden weight loss or spontaneous weight gain, drowsiness during the day and insomnia at night, dry skin, increased sweating, irritability, unreasonable attacks of panic or fear.
- Pregnancy. Expectant mothers are required to donate blood twice before the baby is born, in the first and third trimester.
Disturbed pigment metabolism
In the human body there are specifically colored proteins. These are peptides that contain a metal (for example, copper or iron). Such peptides include cytochrome, hemoglobin, myoglobin, etc. As a result of the breakdown of peptides, bilirubin and its fractions are formed.
Free bilirubin appears after the breakdown of red blood cells in the spleen. This bilirubin is very toxic, especially to the human brain. However, the body is not poisoned due to the rapid connection of free bilirubin with albumin. In liver diseases such as cirrhosis and hepatitis, the concentration of bilirubin in the body increases due to a decrease in the amount of albumin and the predominance of glucuronic acid.
Indirect bilirubin binds to this acid, which loses its toxicity. It then enters the bile and is converted into urobilinogen. This enzyme, in turn, penetrates through the small intestine into the blood and then into the kidneys. It is urobilinogen that colors urine yellow.
Why does jaundice appear?
There are several mechanisms for the occurrence of jaundice.
| Cause of jaundice | What's happening? |
| Increased breakdown of hemoglobin | Due to the too active production of indirect bilirubin, the liver simply cannot cope with its processing and excretion |
| Liver diseases | The amount of bilirubin produced does not exceed the norm, but the affected liver cells are not able to fully function and cope with their work |
| Impaired flow of bile | Instead of entering the intestines, bile accumulates in the liver and provokes its destruction. Bilirubin then enters the blood again. |
Jaundice is an indication for a biochemical blood test to determine the level of bilirubin in the blood. These indications also include liver tumors and cirrhosis, hepatitis, and hemolytic anemia.
Immunological blood test
Few people know what blood tests there are from the point of view of the human immunological system, since these tests are not so common. As a rule, such a blood test provides information about the immunodeficiency virus in the human body and is anonymous, since it is carried out at the request of the patient. For sampling, blood taken from a vein on an empty stomach is used, from which serum is obtained for testing by centrifugation. In addition, the study of blood serum can detect a number of sexually transmitted diseases (syphilis, herpes, chlamydia), as well as all types of hepatitis, measles, rubella, mumps and toxoplasmosis.
Basically, for ELISA analysis, the biological material being studied is blood, however, cerebrospinal fluid, vitreous contents, amniotic fluid, etc. can be examined.
What is immunoglobulin (antibody)?
Immunoglobulins are immune molecules that can bind to and neutralize most infectious pathogens and toxins in the body. In this case, the most important characteristic of immunoglobulins is their specificity, that is, the ability to bind to a specific antigen. It is this property that is used to conduct a blood test for immunoglobulin.
There are five types of immunoglobulins, but the most studied are immunoglobulins A, M, and G. Immunoglobulins M and G show their activity in the blood. Immunoglobulins A are a kind of barrier on the surface of the mucous membranes, as they are present there in large quantities.
An immunological blood test allows you to determine the type of immunoglobulins, thanks to which ELISA allows you not only to diagnose the disease, but also to determine the stage of the disease and monitor the dynamics of the disease:
- In the first 2 weeks of the disease, only immunoglobulins A are detected.
- From the 2nd to the 3rd week of the disease, immunoglobulins A and M are detected in the blood.
- From 3 to 4 weeks, a blood test for immunoglobulin determines all three types.
- During recovery, immunoglobulins M disappear from the blood, and the amount of A and G decreases by 2–4 times.
- In the presence of a chronic process, immunoglobulins G are necessarily present in the blood, immunoglobulins M are absent, immunoglobulins A may or may not be present.
Advantages of enzyme immunoassay (ELISA):
- Relatively high sensitivity (accuracy).
- Reasonable price.
- Allows for early diagnosis (due to the ability to determine immunoglobulin classes during analysis).
- Allows you to monitor the dynamics of the infectious process (thanks to the ability to determine immunoglobulin classes).
- Ease of use.
- An immunological blood test allows you to get a quick answer.
Disadvantages of ELISA blood test:
- Sometimes enzyme immunoassays give false positive or false negative results.
Scope of application of immunological blood test
- Diagnosis of viral diseases: hepatitis, herpes, Epstein-Barr virus, cytomegalovirus, etc.
- Sexually transmitted infections: chlamydia, gonorrhea, trichomonas, mycoplasma, ureaplasma.
- Syphilis.
- Endocrinology (determination of hormone levels).
- Tumor markers (diagnosis of cancer).
- Immunology (diagnosis of immunodeficiency).
- Allergology (diagnosis and treatment of allergies).
Serological blood test is a laboratory method of blood testing that is used to diagnose infectious diseases and determine the stage of the infectious process. The serological reaction is based on the interaction of antibodies and antigens.
Determination of antigens is used to determine the genus and species of microorganisms. This research method is used in urology and venereology. Blood for a serological blood test is taken in the morning on an empty stomach from a vein.
Biochemical analysis and blood enzymes
Enzymes are proteins that help speed up chemical reactions in the body. The main enzymes are: ALP (alkaline phosphatase), ALT (alanine aminotransferase), CK (creatine kinase), GGT (gamma-glutamyltransferase) and AST (aspartate aminotransferase). They are found in large quantities in the pancreas, liver cells, heart, and muscles. There are few enzymes in the blood.
AST and ALT are involved in chemical reactions and are necessary for the transport of alanine and aspartate. These enzymes are found in muscle tissue, heart and liver. Elevated levels of ALT and AST in the blood are a sign of destruction of the cells of those organs in which an excess of the permissible norm was detected.
Reasons for increased AST and ALT:
- Myocardial infarction.
- Liver lesions.
- Hepatitis.
- Liver tumors and metastases.
- Destruction of skeletal muscles.
ALP is needed by the body as a way to deliver phosphorus to cells. Alkaline phosphatase can be bone or liver. The main reasons for increased levels of alkaline phosphatase in the blood:
- Cytomegalovirus;
- Hepatitis;
- Sarcoma;
- Metastases in the bones;
- Multiple myeloma;
- Liver damage from toxins;
- Osteoporosis;
- The healing process of bone fractures.
The purpose of GGT is, first of all, to participate in the transfer of cholesterol and fats into the cell. Most of all this enzyme is found in the kidneys, prostate gland, liver, and pancreas. The concentration of gamma-glutamyltransferase in the blood increases when:
- Diabetes mellitus;
- Alcohol poisoning;
- Liver diseases;
- Mononucleosis;
- Heart failure.
CC is aimed at maintaining energy metabolism in the cell at the required level. There are three types of creatine kinase:
- BB (location: brain);
- CF (heart muscle);
- MM (muscle tissue).
The level of CK in the blood increases due to destructive processes in these organs and tissues. This destruction occurs due to the following pathologies:
- Myasthenia;
- Gangrene;
- Encephalitis;
- Myorcarditis;
- Myositis;
- Amyotrophic sclerosis;
- Myocardial infarction;
- Treatment with prednisone;
- Schizophrenia;
- Sclerosis.
Alpha amylase
This enzyme is special. It breaks down complex carbohydrates into simpler compounds. Alpha amylase is concentrated in the salivary glands and pancreas. When examining blood, the doctor will definitely pay attention to the decrease and increase in the level of this enzyme.
Alpha-amylase exceeds the normal level in hepatitis, pancreatic cancer, pancreatitis, mumps, and renal failure.
A decrease in the level of the enzyme is observed with alcoholism, myocardial infarction, toxicosis during pregnancy, thyrotoxicosis, pancreatic necrosis, and taking steroid drugs.
Blood electrolytes
The most important electrolytes are sodium and potassium. Despite their minimal amount in the body, these substances are involved in almost all human processes and organs. Potassium is a kind of conductor of electrical impulses to the heart. Therefore, even minor changes in potassium levels negatively affect myocardial function. Hyperkalemia is an increase in potassium levels, and hypokalemia is a decrease.
- An upward deviation in the amount of potassium is fraught with arrhythmia, clouding of consciousness, slow heartbeat, and decreased blood pressure. This can happen when the indicator increases to 7.15 mmol/l.
- If the potassium level, on the contrary, falls below 3.05 mmol/l, then vomiting and nausea, difficulty breathing, cardiac and muscle weakness are likely to occur.
Sodium does not play any special role in the metabolic process. It is found in large quantities in extracellular fluid. Sodium has the function of controlling pH and osmotic pressure. The process of sodium production itself is controlled by aldosterone, a hormone of the adrenal cortex. Sodium is excreted in the urine.
The state of hyponatremia (low sodium level) leads to apathy, nausea and vomiting, refusal to eat, drowsiness, weakness, convulsions, and coma.
Hypernatremia (high sodium levels) causes seizures, irritability, muscle tremors, and twitching.
To summarize, I would like to note that each laboratory has its own research equipment and a set of reagents. Therefore, indicators may vary between institutions. Be careful when receiving the test result. It is important that the form contains information about the acceptable standards for all parameters of a biochemical blood test. Only in this case is it possible to interpret the data obtained correctly and identify possible deviations from the norm.
Hormonal blood test
This type of study helps determine the general functioning of the organs of the human endocrine system, as well as identify diseases of the pituitary gland, thyroid gland, adrenal glands and other human endocrine organs. Blood is drawn on certain days depending on the production of the hormone that will be tested. This can be an analysis of thyroid hormones (T4, T3), pituitary gland (TSH, LH, FSH), sex glands (testosterone, estriol), adrenal glands (cortisol), as well as pregnancy hormone (hCG). The results will depend entirely on the age and gender of the person, as well as whether there are any diseases in his endocrine system.
Preparing for a hormone test
The amount of hormones in the blood depends on the time of day, since there is a daily rhythm of secretion (release of hormones). Blood for hormonal analysis should be taken in the morning, on an empty stomach.
In women, hormonal levels also depend on the stage of the menstrual cycle. The most favorable days for analysis are days 5-7 of the cycle, starting from the first day of menstruation.
On the eve of the test, you should not drink alcohol, and you should also avoid increased physical activity and stressful situations. It is advisable not to smoke for an hour before the test.
A week before the test, you must stop taking hormonal medications. If you are prescribed medication, discuss this with your doctor; the test may have to be postponed.
How to take a hormone test correctly?
The human hormonal system is connected to all organs and systems of the body. Therefore, the level of hormones in the blood may depend on various external influences and changes in the human body. General recommendations from doctors are as follows: you need to take a blood test for hormones in the morning on an empty stomach. Before donating blood for hormone testing, stop smoking, drinking alcohol and strenuous physical activity. Women need to have many hormones analyzed on certain days of the menstrual cycle. To ensure that the results of your hormone tests are as reliable as possible, consult your doctor and follow his recommendations.
When is a blood test for hormones prescribed?
Hormonal analysis is usually carried out if there is a suspicion of dysfunction of the endocrine glands or if an increase in the size of the glands is detected.
Indications for testing for female sex hormones (estrogens) are:
- menstrual irregularities;
- infertility;
- miscarriage;
- acne;
- overweight;
- fibrocystic mastopathy (breast disease).
Indications for testing for male sex hormones (androgens) are:
- suspicion of the development of tumor processes;
- ovarian dysfunction;
- kidney dysfunction;
- overweight (obesity);
- infertility;
- acne;
- in women – excessive growth of body hair.
Hormonal analysis is prescribed during pregnancy if pathological development of the fetus is suspected. An analysis for the hormone hCG (human chorionic gonadotropin), produced by the cells of the membrane of the embryo, can detect pregnancy already on the 6-10th day after fertilization.
Interpretation of blood test results for hormones
Blood from a vein is used to test hormones.
Depending on the clinical signs indicating a specific pathology, an analysis with tests for specific hormones is usually prescribed.
The most complete picture of your health can be obtained by taking a test for the following hormones.
Thyroid hormones:
- T3 (triiodothyronine) free – stimulates oxygen metabolism in tissues. Normal values: 2.6 - 5.7 pmol/l.
- T4 (thyroxine) – stimulates protein synthesis. Normal values: 0.7-1.48 ng/dl.
- Antibodies to thyroglobulin (AT-TG) are an important parameter for identifying a number of autoimmune diseases. Normal values: 0-4.11 U/ml.
- Some others.
Pituitary hormones:
- TSH (thyroid-stimulating hormone) – stimulates the production of thyroid hormones (T3 and T4). Normal values: 0.4-4.0 mU/l. An elevated TSH value usually indicates decreased thyroid function.
- FSH (follicle stimulating hormone) . Normal values: in women - depends on the phase of the menstrual cycle. Phase I – 3.35-21.63 mU/ml; Phase II – 1.11-13.99 mU/ml; postmenopause – 2.58-150.53 mU/ml; girls under 9 years old 0.2-4.2 mU/ml. In men – 1.37-13.58 mU/ml.
- LH (luteinizing hormone) . Normal values: in women - depends on the phase of the menstrual cycle. Phase I – 2.57-26.53 mU/ml; Phase II – 0.67-23.57 mU/ml; postmenopause - 11.3-40 mU/ml; girls under 9 years old - 0.03-3.9 mU/ml. In men – 1.26-10.05 mU/ml.
- Prolactin . The main function is to stimulate the development of mammary glands and lactation. Normal values: in women (from the first menstruation to menopause) - 1.2-29.93 ng/ml; in men - 2.58-18.12 ng/ml. Increased concentrations of prolactin are called hyperprolactinemia . There are physiological and pathological hyperprolactinemia. Physiological hyperprolactinemia can be caused by breastfeeding, pregnancy, severe physical activity, and stress. An increased concentration of prolactin in women leads to menstrual irregularities and may cause infertility. In men, hyperprolactinemia leads to decreased libido and impotence.
- ACTH (adrenocorticotropic hormone) – stimulates the synthesis and secretion of hormones from the adrenal cortex. Normal values: 9-52 pg/ml.
- Some others.
Sex hormones:
- Testosterone (male sex hormone) is produced by the adrenal glands and in the gonads (in men - in the testicles, in women - in the ovaries). Affects the development of the genital organs, the formation of secondary sexual characteristics, the growth of bones and muscles. Normal values: for men - 4.94-32.01 nmol/l, for women - 0.38-1.97 nmol/l.
- Estrogens (female sex hormones). The main estrogens - progesterone and estradiol - are produced by the adrenal glands and ovaries. Normal values of progesterone in women depend on the phase of the menstrual cycle: Phase I - 1.0-2.2 nM/l; Phase II - 23.0-30.0 nM/l; for postmenopause - 1.0-1.8 nM/l. Similarly for estradiol: phase I - 198-284 pM/l: phase II - 439-570 pM/l; for postmenopause - 51-133 pM/l. Elevated estrogen levels may indicate tumors of the ovaries and adrenal cortex, as well as cirrhosis of the liver. Reduced - for insufficient development and sclerosis of the ovaries.
Adrenal hormones:
- DEA-s (dehydroepiandrosterone sulfate) is necessary for the synthesis of testosterone and estrogens. The range of normal values for the concentration of this hormone: 3591 – 11907 nmol/l; in women - 810 - 8991 nmol/l. However, this is the general picture; when processing analysis data, the patient’s age must also be taken into account.
- Cortisol is involved in many metabolic processes and is actively produced as a result of the body’s response to hunger or stress. Normal values: for children under 16 years of age - 3-21 mcg/dl, for an adult - 3.7-19.4 mcg/dl.
- Aldosterone is responsible for regulating water-salt balance in the body. Normal values: 35 - 350 pg/ml.