According to epidemiological studies, a connection has been established between cholesterol levels and the risk of cardiovascular diseases. Lipid metabolism disorders by themselves, as well as in combination with other risk factors for the development of cardiovascular diseases, can lead to the development of atherosclerosis and increase the risk of cardiovascular and cerebrovascular diseases.
Dyslipidemias include a wide range of disorders, some of which play an important role in the development of cardiovascular diseases.
Assessment of lipid metabolism after reaching the age of 40 years is indicated for men, and at the age of 50 years - regardless of gender; patients with identified cardiovascular diseases, as well as conditions that are combined with an increased risk of their development:
- chronic autoimmune diseases: rheumatoid arthritis, systemic lupus erythematosus and psoriasis;
- hypertension during pregnancy in women;
- erectile dysfunction in men;
- chronic kidney disease;
- diabetes mellitus type 1 and 2;
- family history of early development of coronary artery disease;
- HIV treatment;
The development of dyslipidemias may be caused by other diseases (secondary dyslipidemias) or a combination of hereditary predisposition and unfavorable environmental factors (diet errors and sedentary lifestyle). The greatest attention is paid to increasing the level of total cholesterol (TC) and low-density lipoprotein cholesterol-LDL cholesterol.
Lipostatic (aimed at reducing the level of cholesterol and its derivatives) therapy is considered as a long-term strategy for primary and secondary prevention of cardiovascular diseases and their complications (death, stroke, heart attack). Drug therapy and lifestyle changes can affect lipid levels. At the same time, the effect of non-drug preventive measures is considered insufficient [].
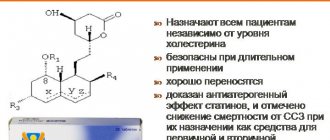
Statins have the most pronounced effect on the lipid spectrum. Other strategies for correcting dyslipidemia (taking fibrates, bile acid sequestrants, diet) do not reduce cardiovascular risk. Their use is indicated only for statin intolerance [,].
The use of statins significantly reduces mortality from cardiovascular diseases. Long-term experience with use confirms the good tolerability and high safety of this class of drugs.
Table 1 Effects of various lipostatic drugs on cholesterol metabolism parameters
| Drug class | LDL-C | HDL-C | Triglycerides |
| Bile acid sequestrants | ↓ 15 — 30 % | 0 - slight increase | No changes1 |
| A nicotinic acid | ↓ 10 — 25 % | ↑ 15 — 35 % | ↓ 25 — 30 % |
| HMG CoA reductase inhibitors | ↓ 20 — 60 % | ↑ 5 — 10 % | ↓ 10 — 33 % |
| Gemfibrozil | ↓ 10 — 15 % | ↑ 5 — 20 %2 | ↓ 35 — 50 % |
| Fenofibrate (microionized form) | ↓ 6 — 20 % | ↑ 5 — 20 % | ↓ 41 — 53 % |
| Cholesterol absorption inhibitors | ↓ 17 % | ↑ 1 % | ↓ 7 — 8 % |
| Neomycin | ↓ 20 — 25 % | Without changes | Without changes |
| Omega-3 unsaturated fatty acids | ↑ 4 — 49 % | ↑ 5 — 9 % | ↓ 23 — 45 % |
The widespread use of drugs in this group for primary and secondary prevention is reflected in the recommendations of modern guidelines. Statins are among the best-selling drugs in both the US and Europe.
Correction of dyslipidemia with statins is aimed at reducing the overall cardiovascular risk of a particular patient. In this regard, both the American and European guidelines indicate a differentiated approach to determining the dose of drugs and target values of lipid spectrum indicators.
Scheme 1 Determination of the dose of statins depending on a set of risk factors for cardiovascular complications (ACC/AAC, 2013).
High-dose statins provide ≥50% reduction in LDL levels
Scheme 2 SCORE scale
Table 2 Different intervention strategies depending on overall cardiovascular risk and LDL cholesterol*
| LDL cholesterol level (mmol/l) | |||||
| Overall risk of developing CVD (SCORE), % | <1,8 | 1.8 to <2.6 | 2.6 to <4.0 | 1.8 to <4.6 | ≥4,9 |
| <1 | No interference with lipid metabolism is required | No interference with lipid metabolism is required | No interference with lipid metabolism is required | No interference with lipid metabolism is required | Lifestyle changes, drug therapy if necessary |
| Class a/Level b | I/C | I/C | I/C | I/C | IIa/A |
| ≥1 to <5 | No interference with lipid metabolism is required | No interference with lipid metabolism is required | Lifestyle changes, drug therapy if necessary | Lifestyle changes, drug therapy if necessary | Lifestyle changes, drug therapy if necessary |
| Classa/Levelb | I/C | I/C | IIa/A | IIa/A | I/A |
| ≥5 to <10 or high risk | No interference with lipid metabolism is required | Lifestyle changes, drug therapy if necessary | Lifestyle changes and immediate initiation of drug therapy | Lifestyle changes and immediate initiation of drug therapy | Lifestyle changes and immediate initiation of drug therapy |
| Class a/Level b | IIa/A | IIa/A | IIa/A | I/A | I/A |
| ≥10 or very high risk | Lifestyle changes, drug therapy if necessary | Lifestyle changes and immediate initiation of drug therapy | Lifestyle changes and immediate initiation of drug therapy | Lifestyle changes and immediate initiation of drug therapy | Lifestyle changes and immediate initiation of drug therapy |
| Class a/Level b | IIa/A | IIa/A | I/A | I/A | I/A |
* EOK/EOA Guidelines for the Diagnosis and Treatment of Dyslipidaemias (2016)
Table 3 Similarities and differences in drug therapy between the 2011 EOA/ESC recommendations for the treatment of dyslipidemia and the 2013 ACC/AAC recommendations for lowering blood cholesterol levels to reduce the risk of cardiovascular complications of atherosclerosis.
| EOA/EOC, 2011 | ACC/AAS, 2013 | |
| Secondary prevention | Target LDL cholesterol <1.8 mmol/L, or at least a 50% reduction. If the target cannot be achieved with statins, combination therapy should be considered. | High intensity statin therapy. If a 50% reduction is not achieved, combination therapy should be considered. |
| Statin intolerance in secondary prevention | Reduce statin dose, consider combination therapy | Moderate to low dose statin therapy, consider combination therapy |
| Primary prevention, LDL >4.9 mmol/l | Target LDL-C level <2.5 mmol/l. If the target level is not achieved, reduce LDL-C as much as possible using a combination of existing drugs at tolerated doses. | High dose statin therapy aimed at achieving at least a 50% reduction in LDL cholesterol. If a 50% reduction is not achieved, consider additional therapy. |
| Primary prevention for diabetes mellitus | Diabetes mellitus in combination with other risk factors or target organ damage: target LDL cholesterol ≤ 1.8 mmol/L, or at least a 50% reduction. Uncomplicated diabetes mellitus: target LDL level < 2.5 mmol/L | High risk diabetes: High dose statins. Low risk diabetes: moderate dose statins. |
| Primary prevention in patients at high risk of cardiovascular complications | SCORE ≥ 5% risk of fatal cardiovascular disease: target level < 2.5 mmol/L | Cumulative risk of cardiovascular events > 7.5%: moderate-to-high-dose statin therapy. Risk of cardiovascular events 5-7.5%: moderate-dose statin therapy. |
Conditions for which patients receive treatment consistent with secondary prevention
Cardiac ischemia
- Myocardial infarction
- Angina pectoris
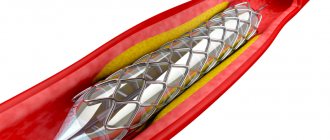
- Revascularization operations on the coronary arteries
Cerebrovascular diseases
- Stroke
- Transient ischemic attack
Peripheral artery diseases
Multiple risk factors with an overall 10-year risk of developing cardiovascular disease >20%
Chronic kidney disease with GFR <45 ml/min per 1.73 m2
©2016 UpToDate®
Mechanism of action
Currently, it is customary to separate lipid and non-lipid (pleiotropic) mechanisms of action of statins (E.A. Koval, 2007).
The main lipid mechanism of action of statins lies in blocking the activity of a key enzyme - 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMG-CoA reductase), which takes part in the synthesis of cholesterol in the liver. Since cholesterol is the main element of intracellular metabolism, in case of its deficiency, receptors for the main transport form of cholesterol - apoB - are actively expressed on the cell surface, as a result of which the main transport form of cholesterol - LDL and VLDL, triglycerides (TG) are captured from the blood. The level of TG in the blood is greatly influenced by lipophilic statins, which block the synthesis of VLDL and the inclusion of the apoB protein in their composition.
Statins can increase the level of HDL cholesterol, regardless of the degree of decrease in the concentration of LDL cholesterol in the blood. Thus, statins have a positive effect on all parts of lipid metabolism in atherosclerosis.
Moreover, numerous clinical studies have found that, at least in high-risk patients, lower TC and LDL-C levels are associated with a statistically and clinically significant reduction in the risk of death from cardiovascular disease. This is why TC and LDL-C levels remain the main recommended therapeutic targets in these guidelines
A meta-analysis of 9 large studies showed a strong correlation between the reduction of LDL cholesterol with statins and a decrease in intima-media thickness (IMT) in the carotid arteries (every 10% decrease in LDL cholesterol is associated with a 0.73% decrease in IMT thickness in year).
The mechanism for the beneficial effects of lowering lipid levels is not fully understood. A decrease in the severity of atherosclerotic lesions is observed only in a small proportion of patients; in addition, at least six (6-12) months are required for the development of the clinical effect of the lipostatic action of the drugs. The action of statins may be based on factors such as plaque stabilization, a decrease in the severity of endothelial dysfunction with a decrease in epithelial thrombogenicity.
The neuroprotective potential of HMG-CoA reductase inhibitors is discussed. In a pilot study, a lower degree of severity of neurological symptoms was revealed if IS occurred during treatment with statins.
How to take statins: before or after meals?
- Food does not have any significant effect on the absorption of satins. Diet plays a big role. The effectiveness of statins can be easily negated by food. To do this, it is enough to add foods high in cholesterol, trans fats, saturated fats, and sugar to the menu.
- The products do not affect the absorption of dietary sterol. A large amount of cholesterol in the body compensates for the lack of synthesis through food. And as a result, the sterol level does not decrease.
- A prerequisite is the exclusion from the diet of alcoholic beverages , which cause a strong blow to the liver. Added to this is the medication burden. Smoking also has a negative effect on lowering cholesterol because nicotine damages the vascular system.
- While taking statins of the 1st-3rd generation, drinking grapefruit juice . It contains substances that block the transport enzyme needed to remove the drug from the body. The amount of medication in the blood increases, which causes side effects.
- An exception is the drug lovastatin. It is taken during dinner.
Effects of statins not related to the main mechanism of action [9].
In a meta-analysis of 19 studies performed from 1998 to January 2012, 48 effects of statins were identified that were not related to their main action.
Neurological and mental diseases:
A meta-analysis of statin studies found that taking drugs in this group reduces the risk of developing dementia, mild (non-dementia) cognitive impairment and Alzheimer's disease by approximately 30%. Notably, in better-designed studies with larger sample sizes and follow-up durations, the effect of statins on the risk of these conditions was less pronounced. There is less convincing evidence that statin treatment is associated with a reduced risk of developing Parkinson's disease.
Despite data from individual studies, an increase in the risk of developing peripheral polyneuropathy, depression and suicidal behavior was not identified in the meta-analysis.
Visual disorders
There was no increase in the incidence of cataracts, glaucoma and age-related macular degeneration in patients taking statins.
Thromboembolic complications (deep vein thrombosis (DVT), thromboembolism of the pulmonary artery and its branches (PE))
Taking statins is associated with a reduced risk of thromboembolic complications, and data from higher-quality studies indicate a less pronounced effect of statins on the incidence of these conditions.
Myopathy
An increase in the incidence of myopathy when taking statins was shown to be 2.5-3 times; according to various studies, the incidence of complications was 2.3-9.6 per 10,000. It was shown that the presence of diabetes mellitus in patients does not affect the risk of developing myopathies.
Liver damage and increased activity of liver enzymes
A 1.5-fold increase in the incidence of liver disease was shown during the first year of statin use, with little or no difference thereafter.
In two large prospective studies, the incidence of liver injury was 44 and 120 per 10,000 participants, corresponding to an increased risk of 16 and 50 per 10,000 participants, respectively.
Kidney damage
A meta-analysis did not show an increased risk of kidney damage when taking statins. Data from individual studies are contradictory: there are studies indicating both a higher and lower frequency of this type of pathology in patients taking statins.
Diabetes mellitus type 2
A slight increase in the risk of developing type 2 diabetes mellitus (1.3 times) was shown. Individual studies included in the meta-analysis did not show a negative effect of statins.
Rheumatoid arthritis and osteoarthritis
There has been no increase in the risk of developing rheumatoid arthritis and osteoarthritis in patients taking statins.
Pneumonia
Statins have not been shown to influence the risk of developing upper respiratory tract infections.
Statins for cardiovascular diseases
WOSCOP (West of Scotland Coronary Prevention Study). The West of Scotland study was the first randomized placebo-controlled trial of primary prevention of coronary artery disease in middle-aged men at high risk of coronary atherosclerosis and with hypercholesterolemia (LDL cholesterol ≥5 mmol/l). Pravastatin 40 mg/day was compared with placebo. The study lasted 5 years and included 6595 people. During the study, in the group taking pravastatin, LDL cholesterol levels were reduced by 26%, the incidence of deaths and non-fatal MI decreased by 31%, the need for coronary artery bypass grafting decreased by 37%, and mortality from all causes decreased by 22%. Long-term follow-up of study participants showed that the effect of treatment persisted after 5 and 10 years, despite the fact that after the end of the study, the treatment of participants in the main and control groups did not differ [].
According to the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS), lovastatin was shown to reduce the likelihood of a first coronary attack (unstable angina, fatal and non-fatal myocardial infarction, sudden cardiac death) in patients of both sexes with low risk, without clinical signs of cardiovascular disease and close to average LDL levels of 3.9 (3.4 - 4.9) mmol/l. For every 1000 patients treated with lovastatin for 5 years, 12 myocardial infarctions and 17 coronary revascularization procedures were prevented. The drug had no effect on overall mortality.
Similar results were obtained in the ASCOT-LLA study, which examined the effects of simvastatin (10 mg) in a group of men and women with relatively normal serum cholesterol levels who had hypertension and at least three additional CVD risk factors.
The JUPITER study examined the use of rosuvastatin at a dose of 20 mg per day in healthy young patients of both sexes with elevated C-reactive protein levels and LDL levels below 3.4 mmol/l and showed a significant reduction in the primary endpoints: cardiovascular complications (acute myocardial infarction, unstable angina , sudden cardiac death) and death from all causes (hazard ratios 0.56 and 0.80, respectively).
Use of atorvastatin in patients with coronary heart disease and acute coronary syndrome
The randomized GREACE trial in patients with documented coronary artery disease demonstrated the ability of escalating doses of atorvastatin (from 10 to 80 mg, mean dose 24 mg) to reduce overall and cardiovascular mortality by 43% (p = 0.002) and 47% (p = 0.00). 0017) respectively. Taking atorvastatin was accompanied by a reduction in the incidence of cardiovascular events (MI, unstable angina, repeated myocardial revascularization) by 54% (p<0.0001) and cerebral strokes by 47% (p=0.034) [5].
The double-blind, randomized TNT (Treating to New Target) study in patients with documented coronary artery disease (n=10,001) assessed the effectiveness of different doses of atorvastatin (10 and 80 mg). Thus, on therapy with atorvastatin 80 mg, the primary endpoint (cardiovascular death, non-fatal MI, cardiac arrest with resuscitation, stroke) was identified in 8.7% of patients, and on therapy with atorvastatin 10 mg - in 10.9%. In summary, patients receiving atorvastatin 80 mg had a 22% lower risk of major events than patients receiving atorvastatin 10 mg (odds ratio (OR) 0.78, 95% confidence interval (CI) 0.69–0 .89, p<0.001) [6, 13].
The ability of high doses of atorvastatin 80 mg to reduce the incidence of ischemic events compared with endovascular treatment was demonstrated in the AVERT (Atorvastatin Versus Revasculatization Treatment) study in 341 patients with stable CAD. Patients treated with atorvastatin 80 mg for 18 months had a 36% lower incidence of ischemic events than patients on standard therapy who underwent percutaneous coronary intervention (PCI) (p=0.048). Thus, aggressive statin therapy may be as effective as endovascular treatment in reducing the incidence of ischemic events in patients with CAD [8].
The effectiveness of the original atorvastatin at a dose of 80 mg as secondary prevention of CVD was also assessed in patients with acute coronary syndrome (ACS). Thus, in the randomized, double-blind MIRACL (Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering) study of 3086 patients with ACS (unstable angina or acute non-ST segment elevation MI), the primary endpoint (death, non-fatal MI, cardiac arrest with resuscitation, or resumption of episodes of myocardial ischemia requiring readmission) was achieved in 228 patients (14.8%) in the atorvastatin group and 269 patients (17.4%) in the placebo group (RR 0.84, 95% CI 0.70–1.00 , p=0.048). There was also a lower incidence of symptomatic myocardial ischemia requiring emergency readmission in the atorvastatin group compared with placebo (6.2% vs. 8.4%, p=0.02) [7]. In 171 patients with ACS in the ARMYDA-ACS (Atorvastatin Pretreatment Improves Outcomes in Patients With Acute Coronary Syndromes Undergoing Early Percutaneous Coronary Intervention) study, atorvastatin reduced the risk of 30-day cardiovascular events after endovascular treatment by 88% compared with the group placebo (in the case of atorvastatin therapy 12 hours before endovascular intervention with 40 mg perioperatively) (OR 0.12, 95% CI 0.05–0.50, p = 0.004) [14].
Another study, PROVE IT-TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy Thrombolysis in Myocardial Infarction 22 Investigators), assessed the effectiveness of atorvastatin 80 mg and pravastatin 40 mg in 4162 patients undergoing PCI due to the development of ACS. Compared with pravastatin 40 mg, atorvastatin 80 mg was associated with a reduction in the composite endpoint of death, MI, stroke, unstable angina leading to hospitalization, and revascularization within 30 days of endovascular treatment (21.5% vs. 26.5%, OR 0.78, 95% CI 0.67–0.91, p=0.002), as well as rates of infarction-related revascularization (11.4% vs. 15.4%, p=0.001) and non-infarction -connected arteries (8.0% vs. 10.5%, p=0.017) [15]. Based on this study, it was concluded that atorvastatin therapy reduces the incidence of major adverse cardiovascular events in patients with ACS undergoing PCI.
Statins for cerebrovascular diseases
The prescription of statins is indicated for both acute and chronic cerebrovascular diseases. In the latter case, in the absence of convincing data on the possibility of drug correction of the main symptoms: cognitive impairment, walking disorders, urination disorders, aggressive correction of risk factors for cardiovascular complications becomes of primary importance. These measures are necessary, but not sufficient to slow the progression of microangiopathy. In some cases, chronic vascular lesions of the brain develop in elderly patients with a low overall risk, indicating a complex pathogenesis of the condition.
Key data on the role of statins in secondary stroke prevention came from the SPARCL trial.
Most, but not all, epidemiological studies have shown a combination of high cholesterol levels and a high risk of stroke. An association has also been shown between high cholesterol concentrations and carotid atherosclerosis [].
Data on the effect of cholesterol levels on the risk of hemorrhagic stroke are conflicting. In the MRFIT study, the risk of death from intracranial hemorrhage in individuals with total cholesterol concentrations <4.14 mmol/L was 3 times higher than in individuals with high total cholesterol levels.
The APCSC study showed a 20% (95% CI, 8% to 30%) reduction in the risk of hemorrhagic stroke for every 1 mmol/L increase in total cholesterol. [].
Thus, the level of total cholesterol has a multidirectional effect on the risk of stroke: high cholesterol levels can be combined with a greater risk of ischemic stroke, while low cholesterol levels can be associated with an increased risk of hemorrhagic stroke .
Most studies show an inverse relationship between low-density lipoprotein (LDL) levels and the risk of ischemic stroke [].
Triglyceride concentrations do not influence the risk of stroke [].
Lipostatic therapy is indicated for both primary and secondary prevention of stroke.
A meta-analysis of randomized trials showed that there is no threshold low-density lipoprotein (LDL) concentration at which the risks of statin use outweigh the benefits [].
Statin therapy reduces the risk of developing vascular complications, including first stroke. A meta-analysis of studies published up to December 2008 (160,000 participants) found that:
- prescribing statins in combination with other approaches to primary and secondary prevention of strokes reduces the risk of developing all types of stroke by 18%;
- in 10 studies involving 83,000 patients, statins did not increase the risk of hemorrhagic stroke (relative risk 1.03, 95% confidence interval 0.75-1.41). However, in the subgroup of patients with clinical cerebrovascular disease, most of whom participated in the SPARCL trial, there was an increased risk of hemorrhagic stroke (relative risk 1.73, 95% confidence interval 1.19-2.5);
- The effectiveness of statins for secondary stroke prevention was assessed only in the SPARCL trial (4731 outpatients who were not diagnosed with cardiovascular disease, without sources of cardiogenic embolism, who had a stroke or transient ischemic attack 1-6 months before treatment with atorvastatin at a dose of 80 mg /day or placebo). Lowering LDL concentrations has been shown to reduce the risk of recurrent noncardioembolic stroke (relative risk 0.84). (Amarenco P, Labreuche J. Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention. Lancet Neurol. 2009;8(5):453.). According to the study results, “aggressive” lipostatic statin therapy is recommended for patients who have suffered a transient ischemic attack or ischemic stroke and have not been diagnosed with coronary heart disease to reduce the risk of stroke or acute cardiovascular disease. It is preferable to use atorvastatin at a dose of 80 mg/day. For maximum treatment effectiveness, it is necessary to achieve a reduction in LDL levels by ≥50% of the initial level or <1.8 mmol/L.
When is the best time to take statins?
There are many opinions on when it is best to take statins. But each medication comes with instructions that tell you how and when to take them.
Cholesterol synthesis occurs in large quantities at night. During this period, the concentration of statin in the blood should be high. The drug blocks the largest number of cholesterol formation reactions and most effectively reduces its concentration.
Each drug has a different half-life:
- Lovastatin - 3 hours;
- Simvastatin - 2 hours;
- Fluvastatin - 7 hours;
- Pitavastatin - 9 hours;
- Atorvastatin - 14 hours;
- Rosuvastatin - 19 hours.
Statins with the shortest elimination period should be taken in the evening, otherwise a small amount of the drug will remain by the time cholesterol is active. Statins with a long elimination period, such as atorvastatin or rosuvastatin, are eliminated from the body slowly, so they can be taken at any time.
Have an effect on cholesterol
- According to studies conducted on the effect of drugs on the level of triglycerides, total cholesterol and HDL, no significant differences were found between morning and evening doses.
- The analysis of statins with the shortest elimination period did not show significant differences between taking the drug in the morning and in the evening. But based on changes in total cholesterol and LDL, it was found that evening dosing was more effective.
- Studies of statins with long-term release of the drug also showed no significant difference in cholesterol and LDL cholesterol readings. But evening doses were more effective in terms of HDL levels.
- There are exceptions, such as pitavastatin. The drug occupies an intermediate position. But the instructions for use indicate that you should take this pill before bed.
SUMMARY
- Statins are a relatively safe group of drugs. The risk of adverse events requiring drug discontinuation is comparable to placebo. The most common pathological increase in liver enzyme activity (0.3-5%, often at the beginning of treatment, is dose-dependent. The incidence of severe liver damage in patients taking statins does not exceed that in the general population (Cohen DE, Anania FA, Chalasani N , An assessment of statin safety by hepatologists. Am J Cardiol. 2006;97(8A):77C.)
- Assessment of liver function is required only before initiating statin therapy, with further follow-up studies only if clinically indicated [].
- The myotoxic effect of statins is rare: the frequency of myalgia is 2-11%, myositis 0.5%, rhabdomyolysis 0.1%. Routine measurement of the activity of the muscle-specific enzyme, creatine kinase, over time is not recommended, however, assessment of its level is advisable at the beginning of statin treatment and when the patient complains of muscle pain and muscle weakness.
- However, these symptoms can also occur in patients without pathologically elevated enzyme activity.
- Statins are more likely to cause muscle tissue damage in patients with chronic renal failure, liver disease with biliary tract obstruction, and in patients with hypothyroidism. In connection with the latter fact, before starting treatment it is also necessary to evaluate the level of thyroid-stimulating hormone (TSH) [].
- Statin use has been poorly studied for several decades. Prescribing statins to patients 20-30 years old requires individual consideration of each case.
- Statin therapy is contraindicated in pregnant women.
- When prescribing statins to elderly patients, it is necessary to take into account life expectancy and the range of chronic somatic diseases. If there is a serious pathology, prescribing drugs from this group is not advisable.