Heart Attack Symptoms
Because cardiogenic shock typically occurs in people who have had a severe heart attack, it is important to know the signs and symptoms of a heart attack. These include:
- Pressing, bursting or squeezing pain in the chest lasting more than 15 minutes;
- Pain radiating to the shoulder, arm, back or teeth and lower jaw;
- Increased frequency of attacks of chest pain;
- Prolonged pain in the upper abdomen;
- Dyspnea;
- Sweating;
- A looming feeling of fear;
- Fainting;
- Nausea and vomiting.
If you see your doctor right away when these signs or symptoms appear, you can prevent the possibility of developing cardiogenic shock. Prompt treatment of a heart attack increases the chances of survival and reduces damage to the heart. Don't ignore these symptoms if they last more than five minutes. Call an ambulance immediately. If you cannot call an ambulance, ask someone to take you to the nearest hospital.
Causes
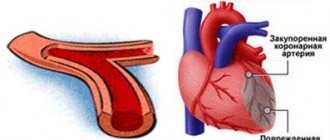
Cardiogenic shock occurs when the heart loses its ability to pump enough blood to the rest of your body. The most common cause of cardiogenic shock is damage to the left ventricle, the main pumping chamber of the heart, due to lack of oxygen due to a heart attack.
A heart attack occurs when one or more of the arteries that carry oxygenated blood to your heart (coronary arteries) becomes blocked. Sometimes, over time, a narrowing of the coronary arteries occurs due to the deposition of cholesterol on their walls. The formation of these deposits, called plaques, in the arteries throughout the body is called atherosclerosis.
During a heart attack, one of these plaques may rupture, forming a blood clot at the site of the rupture, blocking blood flow through the arteries. Without oxygenated blood entering the heart, the heart muscle weakens and cardiogenic shock develops.
In rare cases, cardiogenic shock develops when the right ventricle of the heart is damaged. From the right ventricle of the heart, blood travels to the lungs, where it is enriched with oxygen before being sent to the rest of your body. Damage to the right ventricle causes the heart to lose its ability to pump blood effectively to the lungs, causing the body to not receive enough oxygen.
Although a heart attack is the most common cause, other conditions that cause cardiogenic shock include inflammation of the heart muscle (myocarditis) or infection of the heart valves (endocarditis). Causes include drug overdose or poisoning from substances that affect the pumping function of your heart.
| Intensive therapy | Site's home page | ||
Amniotic embolism
Amniotic embolism is an obstetric disaster that, fortunately, is quite rare. The frequency of this complication, according to various authors, ranges from 1 case in 8000 to 1 in 80,000 births. Amniotic embolism is the most unpredictable and, in many cases, almost unpreventable cause of maternal mortality, with rates reaching 86%. In the structure of maternal mortality, this pathology occupies from 1.2 to 16.5%. Such a wide range of data on incidence and mortality is due to the fact that, unfortunately (or rather, fortunately), not a single doctor can “boast” of extensive personal experience in managing patients with amniotic embolism. Despite the fact that interest in this complication of childbirth has been growing in recent years, doctors’ ideas about the clinical physiology of amniotic embolism and the intensive care of this complication are still very far from the desired perfection. Even though amniotic embolism is rare, it does not matter for the woman in labor and her doctors who are faced with this formidable complication that among other complications of childbirth, the percentage of amniotic embolism is small: the patient who died is 100% for herself and her family. Therefore, it seems to us very important that obstetricians and anesthesiologists are well aware of the current state of the problem of amniotic embolism.
Brief history of the problem
Apparently, the first purposeful description of amniotic fluid embolism was the dissertation of our compatriot N.E. Kasyanov “On the issue of pulmonary embolism by placental giants,” defended in St. Petersburg in 1896. True, in 1893. Ch. G. Schmorl discovered trophoblast cells in the lungs of a woman who died in childbirth and suggested that these cells enter the uterine bloodstream into the heart, and then into the lungs, where they are deposited, creating an obstacle to blood flow in the pulmonary circulation. However, this fairly well-reasoned hypothesis remained unnoticed. The next case of amniotic embolism was reported only 33 years later by the Brazilian doctor LRMeyer. Another year later, experimental work by RMWarden showed significant changes in the cardiovascular system in animals that occur after intravenous administration of amniotic fluid. These perfectly executed experiments had no clinical significance: they were obtained as a “by-product” in the study of the pathogenesis of eclampsia, and not amniotic embolism. This was followed by another break of a decade and a half, until in 1941 two researchers from the University Hospital of Chicago, PESteiner and CCLushbaugh, began a systematic study of amniotic embolism. The authors described this syndrome in 8 women who died suddenly in childbirth, and only after this amniotic embolism was recognized by medicine as a nosological form of the disease. It may seem that in their subsequent works these authors are guilty of overdiagnosis of amniotic embolism, citing a very high incidence of embolism - 1 in 3000 births. However, if we recall the cases of unexpected coagulopathic bleeding and pulmonary edema during childbirth, some of which, as we now know, are caused by undiagnosed amniotic embolism, then the statistics given by the authors will not seem so implausible. However, the “discovery” of amniotic embolism in 1941 flooded the medical literature with this diagnosis, since it was attributed to most cases in which a pregnant or postpartum woman died suddenly. In 1958, fetal epithelial cells were found in the uterine veins without clinical symptoms of amniotic embolism. Therefore, the detection of desquamated epithelial cells in blood samples obtained from the central vein or pulmonary artery, in the absence of clinical manifestations, should not be considered a pathognomonic sign of amniotic embolism, because a small number of them can be detected in the absence of this complication. According to modern ideas about the clinical physiology of amniotic embolism, the cause of the disaster does not lie in fetal scales, which means their detection in the bloodstream cannot always confirm or reject this diagnosis. For a very long time, published materials about amniotic embolism resembled extremely pessimistic scientific, and sometimes unscientific, fiction. And only in the last two decades, experimental and clinical work on amniotic embolism began to be devoted to the mechanisms of development of this formidable complication and its intensive therapy and prevention. One thing is indisputable - with amniotic embolism, amniotic fluid enters the maternal bloodstream. When and how does this happen, that is, what are the physiological mechanisms of amniotic embolism?
Clinical physiology
Conditions for embolism
Using radioisotope methods, it has been shown that during contractions during normal childbirth, amniotic fluid does not enter the maternal bloodstream. For this to happen, two conditions are necessary:
1) a significant excess of amniotic pressure over venous pressure;
2) gaping of the venous vessels of the uterus.
As for the first condition - the excess of amniotic pressure over venous
, - then in the absence of labor, amniotic pressure is about 8
mm water column
, and venous pressure is about 10
mm water column
.
At the height of contractions, these indicators are equal to 20 and 40 mm of water column, respectively,
that is, the first condition for the occurrence of amniotic embolism is not present either at rest or at the height of contractions. However, there are a number of situations that cause an imbalance of these parameters, which makes it possible to identify a group at risk of amniotic embolism. A decrease in venous pressure can sometimes be a consequence of hypovolemia associated with obstetricians' enthusiasm for diuretics in the treatment of edema in pregnant women without proper clinical and physiological understanding of the causes of their occurrence. Hypovolemia with low venous pressure can often accompany pregnancy in patients with diabetes mellitus, heart defects and severe forms of preeclampsia. Amniotic embolism occurs more often in multiparous women. Previously, it was believed that changes in the cardiovascular system that occur during pregnancy undergo complete reversal after childbirth. However, in 1991, ELCapeless and IFClapp showed that the decrease in peripheral vascular resistance that occurs after pregnancy is quite persistent. Therefore, during subsequent pregnancies and childbirths, multiparous women may experience a growing discrepancy between the increasing capacity of the peripheral vascular bed and the volume of circulating blood. As a result, relative hypovolemia and a decrease in venous pressure may sometimes occur, and then the likelihood of amniotic embolism increases. The unreasonable prescription of vasodilators and antihypertensive drugs to pregnant women without appropriate timely correction of volemic disorders leads to a similar result. Amniotic pressure can exceed venous pressure during rapid labor, breech presentation, large fetus or multiple pregnancy, with a rigid cervix and untimely opening of the amniotic sac. Among the factors predisposing to amniotic ambolism are stimulation of labor with oxytocin. It should be borne in mind that during a cesarean section, an infusion of oxytocin at a rate of 10 drops/min can itself lead to the development of arterial hypotension. There was even a report linking castor oil, used to stimulate labor, with the occurrence of amniotic embolism. Ingestion of castor oil increases the concentration of prostaglandin E and thus can induce contractions and potentiate the action of various contractile agents. Therefore, both castor oil and other factors that cause excessively strong contractions and increased intrauterine pressure can contribute to the occurrence of amniotic embolism.
Gaping of the vessels of the uterus - the second indispensable condition of amniotic embolism - is observed with premature placental abruption and with its presentation, with any surgical intervention on the uterus - caesarean section, manual examination of the uterus and separation of the placenta, as well as with postpartum atony of the uterus. Some authors associate amniotic embolism with traumatic non-penetrating uterine ruptures, the entry of amniotic fluid into the bloodstream through damaged endocervical veins or decidual sinuses. The conclusion from these clinical and physiological considerations is specific: various pathologies of pregnancy and childbirth, as well as concomitant hypovolemia of any etiology, including iatrogenic ones, are fraught with the danger of amniotic embolism.
We must pay attention to an amazing paradox: amniotic fluid is a clever invention of nature, designed to preserve the life and growth of the fetus, that is, for the normal development of pregnancy. But the imperfection of this important device is striking, fraught with a mortal threat to the mother and fetus if the amniotic fluid enters the maternal bloodstream, which, as we see, may not be so rare.
Patho- and thanatogenesis
Let's consider the composition of amniotic fluid. Amniotic fluid is a colloidal solution containing mucoproteins with a high carbohydrate content, a large amount of lipids and protein in a concentration of 210-390 mg%
.
Various biologically active substances are present in fairly high concentrations - adrenaline (76 µmol/l
), norepinephrine (59
µmol/l
), thyroxine and estradiol [Barnes].
Amniotic fluid is rich in histamine, levels of which increase in preeclampsia. It also contains profibrinolysine and thrombokinase-like substances. Adding one drop of amniotic fluid to a test tube of blood speeds up the clotting time by half. Amniotic fluid contains many products of protein and fat metabolism, biologically active substances, including cytokines and eicosanoids, as well as various mechanical impurities - epidermal scales, lanugo, cheese-like lubricant. With intrauterine infection of the fetus, the amniotic fluid can become infected, and the entry of infected amniotic fluid into the maternal bloodstream causes even more severe coagulopathy. The clinical physiology of amniotic embolism falls into two main forms - cardiopulmonary shock
and
coagulopathy
, but often these forms differ only in the time and degree of their manifestation.
Cardiopulmonary shock
For a long time there was an opinion that pulmonary arterial hypertension is caused by obstruction of the pulmonary capillaries by mechanical impurities (scales, vellus hair, mucin, etc.), but since in 1 ml
amniotic fluid contains on average about 500-600 cells, then in order for it to create a barrier to pulmonary blood flow, it would be necessary for the lungs to filter about seven liters of amniotic fluid, which requires the amniotic fluid of at least six pregnant women. The hypothesis of an increase in pulmonary vascular resistance with the occurrence of cardiopulmonary shock under the influence mainly of prostaglandin F2a seems more plausible. In animal experiments, the development of pulmonary hypertension and cardiopulmonary shock has been repeatedly noted with intravenous administration of amniotic fluid taken during childbirth, but not in mid-pregnancy. The main difference in the composition of amniotic fluid at these moments is the high concentration of prostaglandins at the time of birth. True, amniotic fluid embolism has been described in the early stages of pregnancy with high rupture of the membranes, but in the early stages amniotic embolism is more manifested by coagulopathy and, to a lesser extent, by cardiopulmonary shock. In 1985, special studies of SLClark ea revealed acute left ventricular failure and a sharp decrease in cardiac output with relatively normal pulmonary vascular resistance in amniotic embolism. A hypothesis arose about the direct toxic effect of amniotic fluid on myocardial contractility, and to test it, isolated animal hearts were perfused with filtered amniotic fluid. This caused pronounced spasm of the coronary vessels and a decrease in cardiac output, that is, heart failure due to direct myocardial ischemia. It is appropriate to remember that prostaglandins F2a and E, as well as thromboxane, cause spasm of the coronary vessels, while prostacyclin dilates them and improves the pumping function of the heart. Rare symptoms of amniotic embolism include the appearance of an unpleasant taste in the mother’s mouth immediately after separation of the placenta, short-term chills and hyperthermia, although most likely these “trifles” are simply rarely paid attention to by specialists intoxicated by the power of their science. Anesthesiologists working in maternity wards are familiar with difficult-to-control postpartum tremors, which can hardly be considered only from the standpoint of hypoergosis, especially when it is followed by hypotonic or coagulopathic bleeding. During a caesarean section, these symptoms are masked by anesthesia. The chain of changes described ends with either ventricular fibrillation or cardiopulmonary shock with the development of components of non-cardiogenic pulmonary edema. The gloomy description of thanatogenesis of cardiopulmonary shock during amniotic embolism has one small silver lining: we mentioned that there are no insurmountable mechanical obstacles to pulmonary and coronary blood flow, and death occurs from reactions triggered by biologically active substances. Coping with them is the main task of the anesthesiologist-resuscitator in the early stages of amniotic embolism.
Coagulopathy
If the phase of cardiopulmonary shock can be successfully overcome, then most patients develop one or another degree of coagulopathy caused by the thromboplastic properties of the amniotic fluid. Disseminated intravascular coagulation syndrome may be the only clinical manifestation of amniotic fluid embolism, and may also precede or complete cardiopulmonary shock. You just need to remember that amniotic embolism is the clinical and physiological basis of many “unexplained” coagulopathic bleeding in obstetric practice. Bleeding can begin without RVS syndrome, due to the fact that amniotic fluid also causes uterine atony. Clinical manifestations and functional diagnosis of the coagulopathic form of amniotic embolism are not specific.
Intensive therapy
Unfortunately, intensive care for cardiopulmonary shock during amniotic embolism most often turns into intensive care. That is why it is necessary that near a woman in labor who is suspicious of the possibility of this complication, there is always a person who knows resuscitation techniques. And it doesn’t matter what he is called in the hospital’s staff list - obstetrician, anesthesiologist, resuscitator or therapist: we will be considered glory after the patient’s safe discharge. But only one person must command, because, as H.V. Hufeland rightly noted, “... one doctor is better than two, two are better than three, etc., with an increase in the number of doctors, the probability of recovery always decreases.”
. When the heart stops due to compression syndrome of the inferior vena cava, venous return practically stops, no matter how hard the heart massage is performed. Therefore, performing pulmonary-cardiac resuscitation in the supine position of a pregnant woman reduces its effectiveness due to a sharp decrease in blood supply to the myocardium due to a decrease in venous return. During resuscitation in late pregnancy, the table should be tilted slightly to the left to reduce aortocaval compression. We believe that amniotic embolism is too formidable a complication of the daily practice of obstetricians and anesthesiologists working next to them to remember about it only when it occurs. Based on knowledge of clinical physiology, identification of risk factors for amniotic embolism, timely elimination of physiological mechanisms contributing to the development of this complication, readiness and equipment for resuscitation and intensive care for both cardiopulmonary shock and coagulopathy - this is the simple basis for success in preserving the lives of patients with amniotic embolism. After successful resuscitation or in cases of amniotic embolism that did not require it, intensive care can be roughly divided into three groups of actions:
I. Suppression of reactions that caused cardiopulmonary shock.
II. Treatment of coagulopathy.
III. Prevention and treatment of multiple organ failure.
We adhere to the following procedure for intensive care of amniotic embolism. Catheterization of the subclavian vein with mandatory monitoring of central venous pressure after eliminating aortocaval compression by tilting the operating table to the left;
Following actions:
* at CVP < 8 cm water column.
correction of hypovolemia is carried out by infusion of colloids and crystalloids in a 2:1 ratio at a rate of 5 to 20
ml/min
, depending on changes in central venous pressure; in case of bleeding, the infusion therapy includes transfusion of fresh frozen plasma or fresh blood;
* at central venous pressure > 8 cm water column
. use drugs with a positive inotropic effect (Dobutrex, etc.), starting with minimal doses; At the same time, glucocorticoids can be administered, which stabilize adrenergic receptors;
* with increasing signs of respiratory failure and PaO2 < 70 mm Hg
. perform tracheal intubation and transfer the patient to mechanical ventilation;
* as early as possible, after monitoring the blood clotting properties, administer heparin at the rate of 50-100 units/kg
simultaneously intravenously in combination with large doses of proteolytic enzyme inhibitors: this can significantly reduce the likelihood of coagulopathy.
Further intensive therapy for the coagulopathic form of amniotic embolism is not specific and requires only a scrupulous clinical and physiological approach. What in critical care medicine does not require this? It is necessary to take blood from the central vein, sputum or tracheal washings, and then examine them for the presence of elements of amniotic fluid, although, as already noted, their presence is not an absolute argument for confirming the diagnosis. An amniotic embolism can masquerade as another extremely serious pathology, and no matter how our intensive care ends, who knows how much effort will still have to be made at the morning conference, proving that it was an amniotic embolism and not something completely different.
| Intensive therapy | Site's home page | ||
Complications
If not treated promptly, cardiogenic shock becomes a fatal condition. Another serious complication of cardiogenic shock is organ damage.
If the heart cannot pump enough oxygenated blood to the rest of your body, damage to the liver, kidneys and other organs develops. When the liver and kidneys are damaged, cardiogenic shock is worsened because the kidneys release chemicals into the blood that support muscle function and the liver produces proteins that help blood clot. With long duration of cardiogenic shock, permanent organ damage can develop.
Cardiogenic shock pathogenesis
The tone of peripheral vessels increases, acute circulatory failure develops with a clear decrease in blood pressure. Some of the blood goes beyond the vascular bed into dilated vessels and blood sequestration develops with hypovolemia and a decrease in central venous pressure. Decreased blood volume and hypotension lead to decreased blood flow to the kidneys, brain, liver, and heart. The result is tissue hypoxia and increased vascular permeability. You can read more about the pathogenesis of cardiogenic shock on our website https://www.dobrobut.com/. Fill out a special form and make an appointment for a personal appointment with the desired specialist.
Diagnostic methods
Diagnosis of cardiogenic shock requires immediate action. Doctors will check for signs and symptoms of shock and then order additional tests to determine the cause of your condition. Methods for diagnosing cardiogenic shock include:
- Blood pressure measurement. People with shock often have low blood pressure. If a person in shock is taken to hospital by ambulance, blood pressure is measured before admission to hospital.
- Electrocardiogram (ECG). This is the first test to diagnose a heart attack. It is often done at the same time as a survey about symptoms. The test involves recording the electrical activity of the heart using electrodes attached to the skin. The pulses appear as "waves" displayed on a monitor or printed on paper. Because the heart muscle cannot conduct electrical impulses normally when damaged, an ECG can help determine whether you are having a heart attack or are in the process of having one.
- X-ray of the chest organs. A chest x-ray will help your doctor evaluate the size and shape of your heart and its blood vessels.
- Blood tests. Blood tests can determine if you have kidney or liver damage, detect signs of heart infection, and also determine if you are having a heart attack. Another type of blood test (arterial blood gas test) is also ordered to determine the amount of oxygen in the blood.
- Echocardiogram. This test uses sound waves to produce images of the heart. During echocardiography, sound waves are sent to the heart from a wand-shaped device (transducer) placed on the chest. Sound waves bounce off the heart and back through the chest and are processed electronically to produce a video image of the heart. An echocardiogram can help identify areas of damage to your heart and problems with the heart's pumping function.
- Catheterization of coronary arteries (angiography, coronary angiography). This test will look for narrowing and blockage of the coronary arteries. Liquid contrast dye is injected into the arteries of the heart through a long, thin tube (catheter) that is passed through an artery in the leg or arm to the arteries of the heart. As the contrast agent fills the arteries, they become visible on X-rays, revealing areas of blockage.
Additionally, during catheterization, your doctor may remove the blockage in the artery through coronary angioplasty and stenting. Angioplasty uses tiny balloons that are inserted through a blood vessel into the coronary artery to widen the blocked area. After angioplasty, a mesh tube (stent) is placed inside the artery to maintain sufficient lumen and prevent re-narrowing in the future.
Resuscitation measures
In case of loss of consciousness and respiratory arrest, urgent resuscitation measures must be performed. Artificial respiration is performed mouth to mouth. To do this, the person’s head needs to be tilted back, placing a cushion made of a towel or any other fabric under the neck. The person performing resuscitation must inhale air, cover the victim's nose with his fingers, and exhale air through the victim's mouth. You need to take up to 12 breaths in one minute.
During the provision of first aid, it is necessary to monitor the patient’s pulse. If a person loses consciousness and heartbeats cannot be heard, chest compressions must be performed. To perform it, the patient is placed on his back, the surface must be hard. The person performing the massage should position himself to the side of the patient. The heels of your palms should press down on the chest area in the middle. Pushes are performed with straight arms; there is no need to bend them. The frequency of pressing is at least 60 shocks per minute. If an elderly person is being resuscitated, the number of pushes per minute is up to 50, for children - 120 pushes. Important! When performing artificial respiration and chest compressions simultaneously, you should alternate 2 breaths with 30 shocks.
Medications
Medicines to treat cardiogenic shock are prescribed to improve blood flow through the heart and improve the pumping function of your heart.
- Aspirin. Aspirin reduces blood clotting and maintains blood flow through the narrowed artery. Take aspirin on your own while waiting for emergency services to arrive, only if your doctor tells you to do so if you are experiencing symptoms of a heart attack.
- Thrombolytics. These drugs help dissolve a blood clot that is blocking blood flow to the heart. The sooner you are given a thrombolytic drug during a heart attack, the better your chance of survival and less damage to your heart. Thrombolytics are prescribed if emergency catheterization of the heart arteries and stenting cannot be performed.
- Antiplatelet agents. Doctors in the emergency room may give you other drugs that are similar to aspirin to prevent new blood clots from forming. These include drugs such as clopidogrel (Plavix) and other platelet glycoprotein IIb/IIIa receptor blockers.
- Other blood thinning drugs. You will likely be prescribed other medications. These include heparin, to reduce the likelihood of dangerous blood clots. Heparin is given intravenously or subcutaneously for the first few days after a heart attack.
- Inotropic drugs. Dopamine or epinephrine is prescribed to improve and maintain heart function.
Risk factors
- Extensive transmural myocardial infarction (according to ECG, infarct changes in 8-9 leads; large zone of akinesia according to EchoCG)
- Repeated myocardial infarctions, especially heart attacks with rhythm and conduction disturbances
- Zone of necrosis equal to or greater than 40% of the mass of the left ventricular myocardium
- Decrease in myocardial contractile function
- Decreased pumping function of the heart as a result of the remodeling process that begins in the first hours and days after the onset of acute coronary occlusion
- Cardiac tamponade
- Elderly age
- Diabetes
Surgical interventions
Surgery to treat cardiogenic shock aims to restore blood flow through the heart. They are performed in specialized cardiac centers. Such interventions include:
- Angioplasty and stenting. Typically, when blood flow through the blocked artery is restored, the signs and symptoms of cardiogenic shock improve. Emergency angioplasty works to clear blocked arteries, allowing blood to flow freely to your heart. Doctors insert a long, thin tube (catheter) that is threaded through an artery in your leg or arm to the blocked artery in your heart. This catheter is equipped with a special balloon. When installing a stent in the area of narrowing, the balloon is inflated to restore the lumen of the artery. In addition, a metal mesh stent may be inserted into the artery to keep it open for a long time and restore blood flow to the heart. Doctors install stents that slowly release drugs into the blood to keep the artery wide enough.
- Balloon pump. Depending on your condition, doctors may place a balloon pump in your heart's main artery (aorta). The balloon pump inflates and deflates to mimic your heart and keep your blood flowing.
Helping a patient in a hospital setting
The algorithm of actions of doctors depends on the characteristics of the patient’s condition. The first medical measures are carried out in the ambulance. The following methods are used here:
- the use of oxygen therapy - the procedure helps to support the patient’s breathing and maintain vital functions until arriving at the hospital;
- use of narcotic analgesics. This event helps reduce severe pain. Medicines such as Droperidol, Promedol, Fentanyl and others are used here;
- to eliminate the risk of blood clots in the arteries, a person is given heparin;
- solutions of Dobutamine, Dopamine, Norepinephrine help normalize the heart rate;
- Injecting insulin with glucose helps improve the nutrition of the heart muscle;
- Panangin, Gilurythmal, Lidocaine help eliminate tachyarrhythmia;
- sodium bicarbonate solution is administered to improve the body's metabolic processes.
Further treatment of cardiogenic shock in a clinical setting involves continuation of therapy started at home and in the ambulance. Upon admission of the patient to the hospital, an immediate comprehensive examination of the body is carried out. This helps to identify contraindications and the risk of side effects that may complicate the situation.
In a hospital setting, resuscitation measures are carried out aimed at restoring the patient’s vital functions
The further standard of care depends on the disease that caused the development of shock:
- a condition in which pulmonary edema occurs requires the prescription of Nitroglycerin, the use of alcohol solutions, and diuretics;
- severe pain is relieved with the help of strong narcotic analgesics, which include Morphine, Promedol, Fentanyl;
- Treatment of severely low blood pressure is carried out using Dopamine solution;
- to preserve breathing in an unconscious patient, tracheal intubation is performed;
- Oxygen therapy helps prevent oxygen starvation of the brain and other organs.
If a person’s condition is serious, it is necessary to use a heart-lung machine and artificial ventilation. During this period, the patient should be provided with the necessary nursing care. It consists of performing hygiene procedures, regularly measuring blood pressure, body temperature and feeding the patient.
Operations
If drug treatment and the listed surgical interventions are ineffective, the doctor will recommend surgery:
- Coronary artery bypass grafting. Bypass surgery involves sewing veins or arteries to bypass the area of blockage or narrowing of the coronary artery. This restores blood flow to the heart. The doctor will suggest this surgery after the heart has recovered from a heart attack.
- Surgeries to repair heart damage. Sometimes the cause of cardiogenic shock is a rupture of one of the chambers of the heart or damage to the heart valve. To correct these problems, the doctor will suggest surgical treatment.
Pre-hospital emergency care
If signs of cardiogenic shock are detected, it is necessary to call an ambulance as soon as possible and provide emergency assistance to the person. To do this, follow these steps:
- Place the patient on any surface, the body should be in a horizontal position, legs slightly elevated. This position ensures better blood flow to the brain.
- During emergency care, it is important to provide fresh air into the room. To do this, you need to open the window or front door. Crowds should not be allowed near the victim.
- The person's neck and chest must be freed from clothing. If there is a tight collar, tie, scarf or other items, they should be removed.
- At the initial stage, you need to measure the patient's blood pressure. In cardiogenic shock it is always reduced. To normalize the indicators, you need to give the patient a drug that contains dopamine, metazone or hydrocartisone.
- If the person is conscious, taking analgesic medications is allowed.
After this, you should wait for the ambulance, and after the doctors arrive, tell them under what circumstances the shock developed.
First aid for the development of shock should be immediate.
Prevention
The best way to prevent cardiogenic shock is to prevent heart attacks. Lifestyle changes used to treat heart disease can help prevent a heart attack. These lifestyle changes include:
- Control of high blood pressure (treatment of hypertension). One of the most important steps to reduce your risk of heart attack and cardiogenic shock is to control your blood pressure. Regular exercise, managing stress, maintaining a healthy body weight, and limiting salt and alcohol intake will help control high blood pressure. In addition to recommendations for lifestyle changes, your doctor may prescribe medications to treat hypertension, such as diuretics, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin receptor blockers.
- To give up smoking. Quitting smoking reduces the risk of having a heart attack. Several years after quitting smoking, a smoker's risk of developing a stroke is the same as a non-smoker's.
- Maintaining normal body weight. Excess weight contributes to the risk factors for heart attack and cardiogenic shock: high blood pressure, cardiovascular disease and diabetes. Losing just 10 pounds of weight will lower your blood pressure and cholesterol levels.
- Reduce cholesterol and saturated fat in your diet. Eating less cholesterol and fat, especially saturated fat, will reduce your risk of heart disease.
- Regular exercise. Exercise reduces your risk of having a heart attack. Exercise lowers blood pressure, increases high-density lipoprotein (HDL) levels, and improves the overall health of your blood vessels and heart. They will help you lose weight, control diabetes and reduce stress. Get regular exercise such as walking, jogging, swimming or cycling for 30 minutes every day.