What kind of care is provided to a patient in intensive care?
A patient diagnosed by an ambulance with acute coronary syndrome is immediately taken to the intensive care unit.
Often, large cardiology clinics have separate specialized infarction intensive care units. Resuscitation during a heart attack primarily consists of providing the damaged heart muscle with oxygen, stopping the developed life-threatening arrhythmias, and correcting hemodynamic disorders and thrombus formation.
To do this, the following procedures are used:
- oxygen therapy - the patient is connected to a ventilator to combat hypoxia;
- infusion therapy - indicated to restore normal blood supply to tissues, water and electrolyte balance, and is used to provide parenteral (intravenous) nutrition;
- sedation – during a heart attack it is very important to calm the patient’s nervous system, for which appropriate medications are used;
- pain relief – ischemia of the heart muscle is accompanied by intense pain, which can lead to the development of shock, so it is relieved with the help of narcotic analgesics;
- prevention of thrombus formation or dissolution of a formed thrombus - it is very important to prevent a recurrent attack or to ensure access of oxygen to the ischemic area, for which anticoagulants such as heparin or warfarin are prescribed;
- strict bed rest is necessary to minimize physical activity and restore the body.
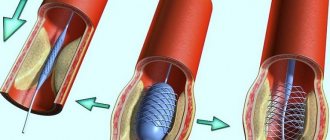
While in intensive care, the patient can be treated surgically:
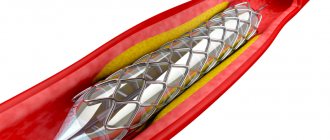
stenting of coronary arteries;- coronary artery bypass grafting;
- laser angioplasty;
- balloon dilatation of coronary vessels.
Patients are in intensive care after a heart attack under constant supervision of medical personnel. They are connected to equipment around the clock, which automatically takes an ECG, monitors blood pressure, respiration, heartbeat and other indicators. If the patient develops clinical death, he is urgently given cardiopulmonary resuscitation, which consists of the following actions:
- indirect cardiac massage;
- artificial ventilation;
- defibrillation;
- drug support for the patient.
How is a ureteral stent removed?
Removal of a ureteral stent occurs on an outpatient basis and takes much less time than the procedure for its installation. Currently, there are several ways to remove a stent. The first traditional one is cystoscopic. The second is using threads that are tied to a stent and exit through the external opening of the urethra. The third method is applicable only to women and involves using a special sterile loop under X-ray or ultrasound control. The fourth method is less common due to the high cost of the special stent with a magnet used.
In cases of stent encrustation, entanglement, or migration, surgical treatment may be required.
Length of patient's stay in intensive care after a heart attack
In modern medicine, they try to reduce the time a patient spends in a hospital in order to optimize costs and reduce prices for treatment. If previously a patient with a heart attack could stay in the hospital for almost a whole month, now this period has been significantly reduced.
With an uncomplicated course of the disease, the patient remains in intensive care for an average of three days. During this time, a full standard examination is carried out, vital signs are stabilized and appropriate treatment is prescribed. In most cases, surgical intervention becomes necessary. In such a situation, the duration of the patient's stay in the intensive care unit is supplemented by the pre- and postoperative period. But the total period usually does not exceed 7-10 days.
After this, the patient is transferred to a cardiology hospital or discharged home.
What determines the length of a person's stay in the intensive care unit?
The length of time a patient is kept in intensive care after a heart attack is determined by the following factors:
- localization and size of ischemic necrosis;
- the presence of complications (shock, reperfusion syndrome, coma);
- the presence of concomitant diseases (hypertension, diabetes mellitus);
- the age of the patient and his general condition;
- volume of surgical intervention.
The combination of these circumstances creates a wide time frame: some are discharged within a week, others are kept for a month or more. It is necessary to understand that patients with coronary artery disease are always at high risk of recurrent heart attacks, therefore you should strictly follow the doctor’s instructions and not stop the treatment process ahead of time.
A person is discharged if the following criteria are met:
- restoration of normal heart rhythm;
- absence of life-threatening complications;
- absence of disturbances of consciousness.
As well as the length of hospital stay, the time spent in bed rest after discharge was significantly reduced. It was found that a long stay in a supine position increases the risk of complications such as thrombosis, embolism, and bedsores. In most cases, patients can begin to walk fully within 3-4 weeks of the acute episode.
After discharge, the rehabilitation stage begins, which lasts several months (up to a year) and plays a very important role in the further prognosis for the patient.
Duration of sick leave for myocardial infarction
After discharge, the patient is given a sick leave, which is drawn up by the attending physician. If it is necessary to extend its validity, a special medical commission is appointed. The specific duration of sick leave for incapacity for work after a heart attack depends on the severity of the pathology:
- small focal infarction without complications – 60 days;
- extensive large-focal and transmural – 60-90 days;
- complicated heart attack – 3-4 months.
If the following conditions are present, the patient is referred to a medical and rehabilitation expert commission to determine the fact of permanent disability:
- repeated (recurrent) heart attack;
- the presence of severe heart rhythm disturbances;
- chronic heart failure.
The commission determines the severity of the patient's condition and assigns him to one of the functional classes. Depending on the class, doctors decide the future fate of the patient - extend his sick leave, or give him a disability group.
There are four functional classes:
- I – ability to work is preserved, but patients are removed from night shifts, additional workloads, and business trips. In this case, it is recommended to change heavy physical work to lighter work;
- II – only light work is allowed, without significant physical exertion;
- III – patients are recognized as disabled if their activities are associated with physical work or psycho-emotional stress;
- IV – patients are considered absolutely unable to work, they are given a disability group.
Further rehabilitation
A heart attack is not a diagnosis, but a way of life. After the patient leaves the hospital bed, he will have a long period of rehabilitation, during which he will restore his health and performance.
A specific program is prescribed by a cardiologist and physiotherapist. In addition to drug therapy, it includes:
- Spa treatment;
- physical therapy – in accordance with the functional class of the disease;
- dieting and weight control - avoidance of flour and fatty foods, split meals;
- quitting smoking and alcohol, which can significantly reduce the risk of relapse;
- avoiding stress, including psychological training or meditation;
- constant independent monitoring of blood pressure and pulse.
It is also necessary to periodically undergo preventive examinations according to the following scheme:
- first month - every week;
- the first six months - once every two weeks;
- the next six months - once a month;
- in the future – once a quarter.
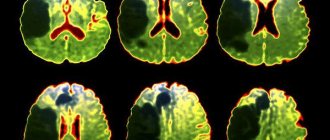
The problem of lung damage during a viral infection caused by COVID-19 is a challenge for the entire medical community, and especially for anesthesiologists and resuscitators. This is due to the fact that patients in need of resuscitation due to developing respiratory failure have a number of specific characteristics. Patients admitted to the ICU with severe respiratory failure, usually over 65 years of age, suffer from concomitant somatic pathology (diabetes, coronary heart disease, cerebrovascular disease, neurological pathology, hypertension, oncological diseases, hematological diseases, chronic viral diseases, disorders in the blood clotting). All these factors indicate that patients admitted to the intensive care unit according to indications belong to the category of severe or extremely severe patients. In fact, such patients have mild to severe ARDS.
In patients with respiratory failure, it is customary to use respiratory therapy. Currently, there are many options for respiratory therapy: oxygen inhalation (low flow - up to 15 l/min, high flow - up to 60 l/min), artificial ventilation (non-invasive - NIMVL or invasive mechanical ventilation, high-frequency ventilation).
In the treatment of classic ARDS, it is customary to use a stepwise approach to the choice of respiratory therapy. A simple scheme is as follows: low-flow oxygen therapy - high-flow oxygen therapy or NIMVL - invasive mechanical ventilation. The choice of a particular respiratory therapy method is based on the severity of ARDS. There are many validated scales for assessing the severity of ARDS. In our opinion, the “Berlin definition of ARDS” can be considered convenient and applicable in clinical practice.
Global practice indicates an extremely high percentage of deaths associated with a viral infection caused by COVID-19 when using invasive mechanical ventilation (up to 85-90%). In our opinion, this fact is associated not with the method of artificial ventilation itself, but with the extremely serious condition of the patients and the characteristics of the course of the COVID-19 disease.
The severity of patients undergoing invasive mechanical ventilation is due to the large volume of damage to the lung tissue (usually more than 75%), as well as the resulting superinfection during prolonged artificial ventilation.
Our own experience shows that the process of repair of lung tissue during COVID occurs by the 10-14th day of the disease. This is associated with the need for long-term artificial ventilation. In anesthesiology and resuscitation, one of the criteria for transferring to spontaneous breathing and extubation is the persistent maintenance of an oxygenation index of more than 200 mm Hg. Art. provided that low values of PEEP are used (no more than 5-6 cm water column), low values of maintenance inspiratory pressure (no more than 15 cm water column), stable indicators of lung tissue compliance are maintained (static compliance more than 50 ml/mbar), there is sufficient inspiratory effort of the patient ( p 0.1 more than 2.)
Achieving adequate parameters of gas exchange, pulmonary mechanics and adequate spontaneous breathing is a difficult task, given the limited respiratory surface of the lungs.
At the same time, the task of maintaining adequate ventilation parameters is aggravated by the addition of a secondary bacterial infection of the lungs, which increases the extent of damage to the lung tissue. It is known that when performing invasive mechanical ventilation for more than 2 days, there is an extremely high risk of nosocomial pneumonia. In addition, in patients with COVID and “cytokine storm”, interleukin inhibitors are used, which are pronounced immunosuppressants, which increases the risk of secondary bacterial pneumonia several times.
In conditions of subtotal or total damage to the respiratory surface of the lungs, the success rate of treatment for respiratory failure is extremely low.
Our own experience shows that the survival rate of patients on invasive mechanical ventilation is 15.3% at the current time.
The algorithm for the safety and success of mechanical ventilation includes:
- Consistent use of respiratory therapy techniques.
- Hand treatment of staff before and after patient manipulation.
- Change bacterial filters every 12 hours.
- The use of closed systems for sanitation of the tracheobronchial tree and adequate regular sanitation of the tracheobronchial tree.
- Prevention of leaks in the breathing circuit.
- Using systems for warming and humidifying the respiratory mixture.
- Use of protective parameters of artificial lung ventilation.
- Regular use of prone positions and changes in body position.
- Adequate oral care and regular measurement of endotracheal or tracheostomy tube cuff pressure.
- Adequate selection of antibacterial therapy regimens taking into account the sensitivity of the pathogen.
- Restrictive infusion therapy strategy (CVP no more than 9 mm Hg)
- Timely use of extracorporeal blood purification methods.
- Regular laboratory monitoring of gas exchange parameters (arterial blood acid base level) - at least 4 times a day.
- Regular monitoring of mechanical ventilation parameters and regular assessment of pulmonary mechanics parameters.
- Good patient tolerance of mechanical ventilation (sedation, muscle relaxation, selection of parameters and trigger sensitivity, provided that the patient is conscious and has his own breathing attempts)
Due to the fact that the survival rate of patients using invasive mechanical ventilation remains extremely low, interest in the use of non-invasive artificial ventilation is increasing. According to modern concepts, it is advisable to use non-invasive mechanical ventilation for mild ARDS. In a pandemic and a shortage of intensive care beds, the percentage of patients with severe ARDS prevails over the mild form.
However, in our clinical practice, in 23% of ICU patients, non-invasive mask ventilation (NIMV) was used as initial therapy for DN and ARDS. There are a number of restrictions on the use of NIMVL: the patient must be in clear consciousness and must cooperate with the staff. It is acceptable to use light sedation to ensure maximum patient comfort.
Criteria for the ineffectiveness of NIMVL are maintaining the oxygenation index below 100 mmHg, lack of tightness of the respiratory circuit, agitation and disorientation of the patient, inability to synchronize the patient with the respirator, head and neck injuries, lack of consciousness, lack of own breathing. Respiratory rate more than 35/min.
In our practice, the success rate of NIMVL was 11.1%. Head OAIR: Ph.D. Gruzdev K.A.
conclusions
Myocardial infarction is a dangerous emergency condition that requires emergency measures to save life. The earlier resuscitation measures are started, the greater the chances of a successful recovery.
During the first three to seven days, the patient is placed in the anesthesiology and intensive care unit, where there are all the necessary conditions for maintaining life and treating the early stages of a heart attack. Subsequently, the patient is transferred to a cardiology hospital. The timing of discharge from the intensive care unit depends on the specific situation. The duration of sick leave also varies according to the severity of each individual patient.