Authors:
Currie KD, Floras JS, La Gerche A, Goodman JM.
Translation
- Sergei Strukov.
Current guidelines defining indicators for exercise testing and the prognostic importance of excessive blood pressure response to exercise lack contextual references and require updating.
- The magnitude and rate of change in blood pressure varies depending on age, gender, baseline values, training level, heart rate, comorbidities, and exercise protocol.
- The clinical utility of blood pressure measurement during exercise may increase with the establishment of normative ranges that integrate similar variables and defining models with better prediction of cardiovascular events.
How does increased blood pressure (BP) occur?
Many people are not even aware that they have high blood pressure, even if it is sometimes measured. That's why doctors call hypertension the silent killer. The pathology is insidious: 70% of people suffering from the disease die in the first 5 years after the official diagnosis. 89% die in their sleep. High blood pressure is a direct path to heart attacks and strokes.
Static loads. Advantages and disadvantages
Training exercises can be divided into static and dynamic. Dynamic work involves the impact of load in combination with muscle movements: working muscle groups can either relax or tense. Static work, on the contrary, involves performing the exercise motionlessly without muscle relaxation. At the moment, experts in the field of physiology talk about the negative impact of static exercises on the health of the circulatory system. And this point of view is completely justified. Prolonged tension created in a muscle without relaxation impairs blood flow. Obstructed blood flow increases the oxygen demand of muscle fibers. At the same time, the heart begins to work harder, which, as a rule, contributes to an increase in blood pressure and increases the load on the entire cardiovascular system. The fact that constant static loads increase blood pressure is noticed by athletes involved in martial arts, especially with the frequent practice of breaking hard objects with bare hands, and this, in turn, involves the impact of static loads on the body, since they make the athlete’s body more stable to the blows.
According to Dr. Gavronina, to improve the musculoskeletal system, a person should exercise exclusively with a moderate degree of intensity. However, moderate or low-intensity exercise is suitable for people suffering from hypertension. In case of vegetative-vascular dystonia with high blood pressure, static training must be used in order to have a hypotensive effect on the walls of blood vessels. The intensity should be low or moderate, and the duration of classes should be medium. Strength exercises should be combined with breathing techniques. Low intensity, according to the doctor, is 25-30% of 1RM (one-repetition maximum), however, it is necessary to determine 1RM in patients with hypertension empirically, using weights equal to 25-30%. The duration of such exercises is from 2 to 30 seconds. A combination of static and dynamic loads, the so-called static dynamics, has a beneficial effect on the circulatory system. The time spent on static work coincides with the time spent on dynamic exercises; therefore, the time the muscle is under load in static work is sufficient to work out the muscle group being loaded. With all this, people, regardless of whether they have signs of hypertension, need to exercise static loads with caution. In this case, especially for hypertensive patients, there is a need to create an individual training program, since a general training plan for people with hypertension is contraindicated.
Slope test
From the point of view of pressure, body movement during gymnastics has a beneficial effect on gymnast athletes, since this improves the functioning of blood vessels and normalizes the orthostatic parameters of the vascular system. The tilt test or orthostatic test, which determines pulse and blood pressure while moving the body from a lying position to a standing position, is an extremely important diagnostic procedure. In this case, static-dynamic training has a number of advantages in contrast to classical aerobic exercise. There are a number of studies showing that the statodynamic type of load has a beneficial effect on the results of the orthostatic test. The final information proving this assumption was described in the works of Mazenkov. The subjects were divided into 2 groups. The 1st group performed exercises in a static-dynamic manner for several series in a row at a slow pace. The principles of physical exercise were as follows:
- Dynamic strength training with an intensity level of 70-80% of 1 RM;
- Isometric exercises last 3-5 seconds;
- Dynamic training at a fast pace.
Initially, all exercises were done in the classical (dynamic) style.
As it turned out, the final results in group 2, which did not use static training, were significantly worse. The results of the orthostatic test were better in group 1. The heart rates between the groups differed by 11 beats when comparing people from the two groups in good health. Participants with a satisfactory state of health differed by 18 beats, and with poor functioning of the cardiovascular system - by 20 beats or more. At the same time, in group 1 the vital capacity of the lungs was higher. This factor may indicate good adaptation of the cardiovascular and respiratory systems to physical activity.
General idea of pressure
The human heart is a pump for pumping blood in the body and providing it to all organs and systems. When it contracts, the chambers contract and blood is released into the vascular bed. This contraction is systole. Then the heart muscle relaxes (diastole) and blood enters the chambers of the heart again for subsequent release. From here, 2 pressure indicators are obtained: systolic and diastolic - upper and lower, respectively.
The normal blood pressure of an adult should not exceed 120/80 mmHg. Art., values below these numbers (for example, 110/70) are also normal. But a fall below 110 or a rise above 130 mmHg. Art. is no longer considered the norm.
130/80 is still the norm, but already borderline. Excess values of more than 130/90 indicate hypertension.
Blood pressure 140/95 is definitely grade 1-2 hypertension, which requires treatment. A person’s blood pressure may rise at times, for example, when they are nervous, scared, or even cleaning the room. During exercise, pressure in athletes increases not only in terms of indicators, but also in frequency, i.e. it increases many times during training. In sports, the heart experiences similar stress constantly, working in extreme mode. Hypertension develops if the norm of pressure in athletes is exceeded more than 2 times in a row during training.
Strength training and atherosclerosis
Atherosclerosis is directly related to an increase in blood pressure, since this disease is characterized by the deposition of cholesterol plaques that narrow the vascular lumen. To maintain normal blood pressure in all tissues and organs, the heart pushes large volumes of blood through narrowed vessels, thereby increasing the pressure. Thus, it can be argued that an increase in blood pressure is only a small part of the consequences that can be a consequence of atherosclerosis. Strength dynamic training with a high degree of intensity (70-80% of 1RM), as well as static training, can become a factor in the development of atherosclerosis. Although today this conclusion is often refuted by new research data. There is an assumption that static training helps to increase levels of “bad” cholesterol (LDL - low-density lipoprotein). This type of cholesterol is called “bad” because it is deposited on the inside of blood vessels and forms plaques. Strength training with a moderate degree of intensity (50-60% of 1RM), on the contrary, reduces the level of “bad” cholesterol. In this case, incorporating pumping into your workouts to lower cholesterol levels may come to mind. Pumping just means working at 50-60% of 1RM. In addition, pumping with alternating antagonist muscles (biceps-triceps, chest-back) has a beneficial effect on blood pressure, normalizing it to normal values. In addition to “bad” cholesterol, the body also contains “good” cholesterol or HDL (high-density lipoprotein). The main difference between “good” cholesterol and “bad” is that “good” cannot be deposited on the walls of blood vessels, but it takes part in most physiological processes, plus it is involved in the production of sex hormones - testosterone and estrogen. Cholesterol is a transport agent for many biological substances. However, a large amount of HDL (“good” cholesterol) is more harmful to the body than beneficial. The HDL level increases due to aerobic and static-dynamic loads and, as a rule, rarely goes beyond the reference values.
Clinical trials conducted under the leadership of Dr. Nekorkina, during which participants performed static exercises, fully confirm the direct dependence of HDL and LDL levels on the effects of physical activity. Participants from group 1 did both static and dynamic exercises. For one static exercise there were 2-3 dynamic ones followed by a long rest. The duration of static work in each exercise was 5-8 seconds. The 2nd group performed only dynamic work. The test results demonstrate that aerobic and static-dynamic work lead to an increase in HDL. However, in group 1, which performed only statodynamic exercises, the HDL/LDL ratio was better.
Etiology of the phenomenon
The reasons are determined by the intensity of the load, nutrition and lifestyle of the athlete. Active sports are automatically a risk group for hypertension. Strength and extreme sports contribute to the development of the disease.
- Bodybuilding and arm wrestling are direct provocateurs of hypertension. How this happens: a huge weight is lifted with a jerk, holding your breath and strong muscle tension. After the jerk, an equally sharp throw with lowering the weight and relaxing the heart muscle. This gives a sharp jump in pressure and can end in disaster. If you have hypertension, intense and long-term fitness and lifting weights are prohibited.
- Diving. The pattern of blood pressure rise here is similar to that described. The only difference is that the body is under water with the additional action of external pressure.
- Parachuting. At altitude there is always not enough oxygen, and parachutists combine this with a surge of adrenaline. All internal organs are working to the limit.
Working hard - that's what competitions and demonstrations are all about. This has the most negative effect on the heart and vascular system, because in order to pump blood in large volumes, the heart must increase its output and contraction frequency. And this is nothing more than tachycardia and hypertension.
Athletes’ blood pressure also increases due to additional negative factors:
- nervous tension from fear of losing;
- fluctuations in body weight;
- lack of sleep;
- salty food.
For example, a strict diet allows the body to be at the desired size and weight. This means a lack of nutrients in the diet, which means increased blood pressure.
Disruption of sleep patterns also leads to pressure surges. Stress is present in all competitions, so it is correct to measure blood pressure at rest.
Taking anabolic steroids definitely increases blood pressure; a jump can be provoked by prolonged sleep or constipation.
Taking a bath or shower is also a reason; after water procedures, recovery time is required. New technologies increase blood pressure - gadgets with electromagnetic fields. The cold in the sleeping area causes vasospasm and also increases blood pressure. The optimal temperature in the room should be about 20 degrees.
Smoking, strong tea and coffee, especially on an empty stomach, are obligatory provocateurs of hypertension.
Blood pressure is not measured while lying down or crossing your legs - this will always increase the readings. Ideally, you should sit upright.
Jacobson's muscle relaxation
As noted earlier, blood pressure is directly dependent on the tone of the vascular walls. In order to lower blood pressure, you need to be able to properly relax your muscles. In 1929, Dr. Jacobson considered the option of non-passively relaxing all human muscles, but on the contrary, he recommended relaxing the muscles after first tiring them. This technique is often used in modern medical practice to treat neurotic diseases. It was later discovered that using this relaxation technique, it is possible to achieve a decrease in blood pressure in hypertensive patients.
Jacobson's muscle relaxation involves short-term muscle tension using willpower. This alternating tension and relaxation of muscles is often found in the techniques of other specialists. The Russian scientist Anokhin at the beginning of the 20th century developed a special system aimed at getting rid of muscle and mental stress. Chinese Wushu gymnastics also uses this method. Short-term blocking of vascular blood flow stimulates baroreceptors that respond to changes in pressure. They transmit signals to the central nervous system that suppress vascular tone and activate the parasympathetic department of the autonomic (vegetative) system, which helps lower blood pressure. Apparently, stimulation of baroreceptors and static work compensate for the contractility of antagonist muscles. If this did not happen, a person would not be able to perform a static load or be stationary. Mental contractions also compress large arteries. It turns out that baroreceptors localized in large vessels have a more powerful effect in terms of muscle relaxation than during isolated work of one muscle group. With all the described advantages of this technique, it can both lower blood pressure and reduce it. In this case, the fluctuations depend on the duration and intensity of the applied loads.
Strength sports
Strength sports are a great and constant stress for the body, after which time is required for long-term recovery of the heart and blood vessels. But the problem is that professional athletes cannot afford long breaks. That is why, before the age of 30, all security officials often develop hypertension - pathologically high blood pressure in athletes. The optimal sport for preventing the disease is aerobic exercise (such as walking, swimming and yoga). At the same time, the vessels dilate, blood pressure normalizes, and the cardiovascular system (CVS) is trained. But security forces do not have such a luxury, because during aerobics they will lose their shape and muscle volume.
Even during one training session, athletes’ blood pressure changes dozens of times and often increases. The heart gradually wears out.
Causes of hypertension in sports
Professional athletes are at risk for developing arterial hypertension.
This is due to the fact that during or after active training the body works for wear and tear. The cardiovascular system is especially affected, as the heart has to increase its rate of contraction and pump more blood. In addition, symptoms of hypertension are associated with:
- with nervous overstrain;
- with chronic lack of sleep;
- with excessive salt intake;
- taking medications (steroids, stimulants)
- with fear and stress;
- large body weight.
Along with these reasons, excessive physical activity can cause the development of hypertension or other complex diseases.
Alarming symptoms
In order to detect a disturbance in the heart’s function in time and the onset of an increase in blood pressure, in the gym you need to have water, a blood pressure monitor, validol, nitroglycerin or prescribed hypotensive drugs with you. You need to measure the pressure several times. It is very convenient to simply wear a bracelet with a tonometer on your arm. It is lightweight, automated, compact and especially relevant for professional athletes.
It is necessary to stop training, or better yet call a doctor, if:
- behind the sternum, with a return to the shoulder blade, arm, there was an acute pressing pain;
- sudden nausea appeared, sometimes with vomiting;
- it’s dark in the eyes and spots flicker;
- deafness and ringing in the ears;
- cold sweat;
- feeling of lack of air and fear of death.
Try to go out into the fresh air or sit near an open door or window. Try to calm down and relax.
Ask for a glass of cold water to sip and wipe your hands and face. You need to take validol or valocordin drops.
Another option: your health is normal, but your blood pressure is elevated on the tonometer. This does not change the algorithm of actions. Sports training is stopped immediately.
We train the heart muscle
During aerobics, blood vessels become elastic due to the development of vascular endothelium and the appearance of new capillaries. At the same time, the performance of the heart increases. This also improves the blood supply to skeletal muscles.
The most beneficial for the heart and blood vessels are:
- swimming;
- race walking;
- yoga (not all asanas);
- water aerobics;
- calm running;
- qigong gymnastics;
- stretching;
- breathing exercises;
- cycling;
- skiing;
- sports dancing and skating.
The list is quite impressive, but running, walking and yoga are still of particular importance.
Running is the most popular and useful sport for hypertension. A moderate jogging pace strengthens the heart, improves general condition, lowers blood pressure, and increases oxygen supply to the brain. When running, it's not the speed that matters, but the duration. Fresh air also improves your health.
Race walking is also a choice for hypertensive non-athletes. By the way, blood pressure in former athletes often remains significantly elevated and requires not only control, but also treatment. Therefore, these recommendations are useful for them too.
Payloads
Depending on the stage of the disease, after consultation with a doctor, an individual training program can be selected for the athlete.
Typically, sports that involve all muscle groups at the same time are approved:
- race walking;
- water gymnastics;
- stretching;
- yoga;
- skiing;
- dance Sport;
- moderate running;
- swimming;
- breathing exercises;
- cycling;
- skating.
The benefits of sports with high blood pressure are reflected in the functioning of the heart. Exercise helps blood vessels carry oxygen to brain cells. This effect is an excellent therapy for hypertension.
The most common sport chosen by hypertensive patients is moderate running.
It helps improve heart function, corrects vascular tone and provides the brain with oxygen. Perfectly improves overall health and reduces blood pressure.
The effect of anabolic steroids on blood pressure
Anabolic steroids are popular not only among bodybuilders. The results with their use, of course, improve, but at a high cost.
A clear increase in achievements produces the opposite effect in that anabolic steroids increase blood pressure in 50% of cases of use and the risk of heart and vascular pathologies.
It is strictly not recommended to combine anabolic steroids and sports for the following categories of people:
- Over 35 years old.
- With poor heredity, a predisposition to hypertension in the family. If the parents were hypertensive, the offspring have a 75% chance of hypertension.
- Who already have at least 2 risk factors for developing hypertension.
The same applies to sports nutrition: if the jar contains instructions for containing caffeine and ephedrine, put it back on the shelf. Even with hypertension (hypertension) of the 1st degree, this cannot be taken. But glutamine, phosphates and creatine are not dangerous.
Generalization and directions for further research
Many clinicians express concern when the SBP response exceeds the “normal” range, but in such cases there is insufficient empirical evidence to make clinical recommendations. Moreover, arbitrarily set upper blood pressure values for stopping CST have the same drawback. We argue that the clinical utility of BP measurements can be improved under the following conditions:
In addition to the maximum/peak values obtained with CST, consider the rate of change of BP (slope of the curve), and establish the level of agreement between these two measurements.
Possibility of influence of age, gender, health status, medications and CST protocol on blood pressure values obtained in the test.
Standardize BP measurements as recommended by Sharman and LaGerche (1):
- Measure at the end of each CST step.
- Measure before ending the test, and if not possible, immediately after stopping the test.
- Use an automated device that can measure on the move (65). This limits interobserver variability. Prefer DBP data from auscultatory devices over oscillometric devices. However, caution is needed as there is little reliable data on these devices, mostly from small studies of healthy people.
- Manual measurements are suitable for experienced assessors. There are no empirical data to inform the threshold effects of training, but regular BP measurement during exercise is likely to be more beneficial than sporadic BP measurement.
Future studies should record and report BP values at which acute cardiovascular events occur during CST to properly assess risk and establish evidence-based upper limits.
Pressure after load: norm and permissibility
An athlete's normal blood pressure should be 120-130/80-90 mmHg. Art. After physical activity, the acceptable change is 140-150/90-100 mmHg. Art. It is important not only to monitor and control the tonometer readings, but also the time during which the numbers return to normal, that is, the period during which the pressure is restored. Normally, it should be no more than an hour. The indicators after and before the load are unequal. Blood pressure tends to rise.
In general, athletes have lower blood pressure than ordinary people due to constant vascular training. After active physical activity, blood pressure increases - this is natural and normal if over a certain period of time everything returns to normal. It is the sharp jumps that are dangerous for athletes, which can provoke a stroke even with a small load.
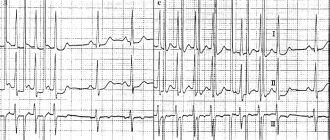
Introduction
Blood pressure (BP) measurement during clinical exercise testing (CST) is a necessary adjunct to electrocardiography (ECG) and heart rate (HR) assessment, as abnormal responses may reveal underlying pathology. Given the difficulty of measuring BP during exercise, accurate measurement techniques are required to ensure optimal clinical interpretation (1). Widely accepted contraindications to continued CST for safety include upper blood pressure limits (2,3). However, definitions of “normal” BP during exercise and a safe “upper limit” are based on a limited number of studies dating back to the early 1970s (4, 5). Since then, our knowledge of phenotypic variations and possible links to pathology of abnormal BP responses has evolved significantly. Despite this, BP responses in CST that exceed the recommended norms often pose a dilemma due to unclear clinical consequences, especially when other tests are normal. There is compelling evidence that excessive increases in systolic blood pressure (SBP) or diastolic blood pressure (DBP) during CST, called the hypertensive response (2, 3), are associated with a 36% increased risk of cardiovascular events and mortality (6), masked hypertension, despite clinically normal blood pressure (7), and an increased risk of latent hypertension in normotensive people (8 – 18). These observations highlight the potential clinical diagnostic and prognostic utility of exercise BP measurements, but they are not yet widely used in clinical practice due to limitations of previous studies (19), lack of standardized methodology, and limited empirical data in the general population.
The purpose of this review is to critically analyze the evidence contained in current guidelines for CST AD. We will show that the criteria used to define “normal” and “abnormal” responses are largely arbitrary and based on insufficient empirical data. We will also identify key factors influencing BP responses during exercise and how to increase their explanatory value in individual responses to CST. Finally, we will provide recommendations for future studies on exercise BP measurement to expand the evidence base and facilitate its adoption into clinical practice.
Pulse
The pulse and blood pressure of an athlete professionally involved in strength sports are always elevated. The system begins to work hard, so beginners may be afraid of their off-scale heart rate.
A person's heart rate decreases slightly with age. In old age it increases slightly again. Women in menopause have an increased heart rate. At the same time, endurance also decreases.
If at the beginning of a sports journey, at 15-25 years old, the pulse can be 75-80 beats per minute, then at 30 years old - 45-50 beats. This is considered normal blood pressure in athletes; in an ordinary person it is bradycardia. In women in the same age group as men, the pulse is always 7-10 beats less.
A weak pulse is the result of insufficient heart function. Blood pressure and pulse are not directly related - you cannot think that lowering your heart rate will also lower your blood pressure.
With significant physical activity, the pulse of professional athletes can reach 200 beats; in weightlifters, when lifting loads, it can reach 120-135 beats per minute. At these moments, it is important to control your breathing.
Prevention
The best prevention of hypertension is dietary adjustments. It is best to exclude foods high in animal fats and sugar from your daily menu, and also avoid caffeine.
It is worth dedicating about 30 minutes of time daily for running and morning exercises.
High blood pressure in athletes requires hospitalization and treatment under the supervision of a cardiologist.
Professional athletes are required to see a personal physician to monitor their workload and prevent the development of dangerous diseases. This is especially true for the work of the cardiovascular system, which during training begins to work in an enhanced mode. Author of the article Svetlana Anatolyevna Ivanova, general practitioner
Is it possible to exercise with low blood pressure?
Not all sports are beneficial for hypotension. By the way, hypotensive people live longer.
If with hypertension the vessels experience stress on the walls and can rupture, then with hypotension the blood, on the contrary, flows poorly into the brain, which provokes hypoxia with subsequent fainting and dizziness.
Low blood pressure in an athlete will lead to a drop during training, so if you have hypotension, exercises with bending, lowering your head, somersaults, hanging your body on a horizontal bar, squats - anything related to balance are excluded. Fatigue and lack of sleep, dieting and fasting for various purposes aggravate the condition.
Sports under control
Any physical activity can be divided into two types:
- Static exercises. This is a set of exercises for increasing physical mass. These include weightlifting, kettlebell lifting, and powerlifting. In people who choose this sport, blood pressure is always higher than normal, so if persistent hypertension occurs, you should stop exercising.
- Dynamic exercises. They use all the muscles of the arms and legs. For example, running, swimming and walking. These types of physical activity improve blood circulation and lower blood pressure.
Even with the correct calculation of your own strength and caution, some exercises should be excluded from daily training.
You should refuse:
- jerks and sudden loads;
- strong tension when exercising on exercise machines;
- loads under which the muscles contract and the limbs are not involved in any way.
Ignoring these recommendations, a person will not be able to avoid sudden jumps in blood pressure. There is a risk of hypertensive crisis, persistent hypertension and headaches. And that's not the worst thing!
High blood pressure in athletes is a common sign of sudden stroke and death.
How to recognize hypertension
High blood pressure in athletes manifests itself as characteristic headaches in the back of the head and temples, and dizziness. Manifestations intensify during training; they may be absent at rest. Other signs of high blood pressure:
- nosebleeds;
- noise in ears;
- deterioration of vision and hearing;
- nausea or vomiting;
- sleep disorders;
- swelling of the limbs;
- hyperemic face during exercise;
- pain in the heart area and increased heart rate even at rest.
Treatment of hypertension
Therapy is carried out comprehensively, but antihypertensive drugs prevail. They are selected only by a doctor, individually, taking into account the stage of hypertension, age and concomitant diseases.
Sartans, ACE inhibitors, adrenergic blockers (alpha and beta), calcium antagonists, diuretics, and combination drugs may be prescribed.
The list is huge, and they all have certain indications and contraindications. Self-medication is excluded.
It is also recommended to regularly measure blood pressure - 3 times a day: immediately after waking up, during the day and before bed.
Therapy is successful if blood pressure does not rise above 120-130/80-90 mmHg. Art. Unstable blood pressure may indicate the possibility of complications or improper treatment.
Recommendations for monitoring blood pressure during training
During training, you should adhere to the following rules:
- Maintaining proper water regime - 2.5 liters of clean water per day.
- The permissible heart rate value is no more than 76 beats/min 2 hours after physical activity.
- To reduce blood pressure, breathing exercises can be used: slow deep breathing with hands on knees. This way you can reduce blood pressure by 20 mm. There is another option - put your hands behind your head and, straightening up, breathe deeply.
So, what blood pressure should athletes have? The characteristic norm after exercise is 131/84 mm Hg. Art.
“Normal” blood pressure reactions to CST
With increasing physical activity, SBP increases linearly, mainly due to an increase in cardiac output to satisfy the demand from working muscles. Sympathetically mediated vasoconstriction reduces splanchnic, hepatic and renal blood flow (this increases vascular resistance), the local vasodilatory effect suppresses vasoconstriction (“functional sympatholysis”), allows the redistribution of cardiac output to working skeletal muscles and reduces overall peripheral vascular resistance. These opposite reactions contribute to the maintenance or slight decrease in DBP during CST. A detailed discussion of the regulatory mechanisms of these reactions is beyond the scope of our review; they are widely discussed elsewhere (20). The American College of Sports Medicine (ACSM) and the American Heart Association (AHA) define a “normal” response as an increase in SBP of approximately 8 to 12 mmHg. Art. (2) or 10 mm Hg. Art. (3) per metabolic equivalent (MET – 3.5 ml/kg/min). The source of these values is a 1973 textbook study where healthy men (with unknown sample size and age) showed mean and peak SBP increases of 7.5 and 12 mmHg. st./MET, respectively. An abnormally elevated (“hypertensive”) response to exercise was defined as exceeding these values (12 mmHg/MET) (5). Thus, widespread and long-standing recommendations defining a “normal” response to CST are limited by data from a single study of men with a poorly characterized phenotype. Below we will present information about the significant impact of the blood pressure response to CST depending on gender, level of training, concomitant diseases and associated medications.
Influence of age and gender
In a study of 213 healthy men (4), changes in SBP in response to increasing exercise intensity increased with each decade of life. The largest increase in SBP per MET was observed in the oldest group (50–59 years; 8.3 ± 2.3 mmHg/MET), compared with an average increase of 5.7 ± 2.3 mmHg. Art./MET in the youngest group (20 – 29 years old). With age, the slope of the response graph increased (p <0.001) (Fig. 1a).
Data on the effect of gender on BP response during CST are limited. A group of healthy women aged 20–42 years responded with an average increase in SBP of 5.0±1.1 mmHg. st./MET (21). The slope of the graph should be less than that of men of the same age (Fig. 1b, p <0.001). It is noteworthy that the average increase in the groups of men and women was much lower than the “normal” response range of 8 – 12 mm Hg. st./MET. In contrast, current studies of the effects of age and sex suggest that in older women, the hypertensive response to exercise occurs due to a limited ability to reduce systemic vascular resistance (22). Unfortunately, there are no data on the BP response to exercise in older adults (>65 years), which limits our clinical interpretation of the BP response to CST.
Impact of health status and medications
The level of training during CST behaves as an independent factor influencing blood pressure. According to Fick's rule, maximum oxygen consumption (VO2max) depends on cardiac output and the arteriovenous oxygen difference. A higher VO2max value corresponds to a higher cardiac output, which means a greater increase in SBP. Therefore, when interpreting the maximum SBP obtained during CST, it is necessary to take into account the level of training (VO2max). The rate of change in SBP can also change with the level of training. In a study of young men, 16 weeks of endurance training increased VO2max and peak SBP (Fig. 2a) during CST (23). When we plotted the increase in SBP during CST versus VO2max, the slope of the curve after training was steeper (Fig. 2b; p=0.019). In women, differences in SBP during CST are also observed depending on training. With increasing training, SBP with CST is lower than that of sedentary peers. Young, exercised women achieve higher SBP at the end of the test compared to their sedentary counterparts (24).
Rice. 1. Response of systolic blood pressure (SBP) to a progressive exercise test in healthy people.
Values are presented as changes (Δ) in SBP compared to baseline values with increasing exercise intensity, expressed in metabolic equivalents (METs):
- a) data from healthy men, divided by decades of life;
- b) data from healthy men (20 – 39 years old) and women (20 – 42 years old).
The figure is based on previously published values (4, 21). Regression equations are presented for each gender.
* p < 0.001 for between-group differences in the slope of the SBP response curve.
Rice. 2. Systolic blood pressure (SBP) response before and after 16 weeks of endurance training in healthy men:
- a) the maximum SBP was obtained in a test with a gradual increase in load;
- b) the increase in SBP during the test is shown as a percentage of maximum oxygen uptake (VO2max).
The figure is based on previously published values (23). Before/after regression equations are shown.
* p < 0.05 for differences in the slope of the SBP response curve.
Comorbidities, especially those affecting BP and its regulation, or other indicators of cardiovascular disease also influence BP response to exercise. In people with normal and untreated hypertension (without known baroreflex sensitivity impairments), there is a similar increase in SBP and mean BP with increasing exercise intensity, but the higher baseline BP in people with hypertension results in greater values at maximal effort (25, 26). Conversely, people with hypertension and impaired arterial baroreflex sensitivity experience a greater absolute increase in BP during bicycle ergometry (27). Individuals with changes in autonomic nervous system function also differ in their BP response to exercise, as cervical spinal cord injuries (eg, tetraplegia) are typically associated with altered cardiovascular activity due to absent or reduced sympathetic tone below injury levels (28). Some studies have shown a decrease in SBP with exercise in people with tetraplegia, compared with healthy controls and people with paraplegia (partial or complete preserved sympathetic tone below the level of injury) (29, 30). Similarly, people with diabetes and autonomic neuropathy experienced less of a rise in SBP from baseline and reached lower peak values (37 ± 6 mmHg and 158 ± 7 mmHg, respectively) compared with people without autonomic neuropathy ( 55±8 mmHg and 176 mmHg) (31). In addition, in patients with coronary artery disease, dyslipidemia, and diabetes, aerobic exercise may increase DBP (32, 33). All of these responses are distinct from the pathological conditions associated with exercise hypotension (10 mmHg decrease in SBP with increased exercise) (2, 3), including coronary heart disease and left ventricular dysfunction (34 – 36). Medications prescribed in this clinical population also lower exercise BP: nitrates, calcium channel blockers, diuretics, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and β-blockers (37). Regarding β-blockers, by recording SBP directly from the brachial artery during bicycle ergometry, Floras et al (38) showed a significant attenuation of the SBP response by chronic blockade of cardioselective β1-adrenergic receptors; but nonselective blockade of β1 and β2 adrenergic receptors did not alter this BP response.
Impact of the CST protocol
The type of CST also influences the blood pressure response. In healthy men, four progressive treadmill protocols resulted in similar maximum SBP (39), whereas in women the slope of the SBP response curve and maximum SBP observed in the Bruce and Balke treadmill protocols were significantly different (21). Treadmill and cycle ergometer exercises, with stepwise and continuous increases in exercise, produced similar maximum SBP in men (40). However, bicycle ergometry results in greater maximum SBP in the clinic (41) and in trained individuals (42), possibly due to the addition of isometric work (hand grip) or increased quadriceps activation (and thus sympathetic afferent activity). Therefore, when interpreting the BP response to CST, the type of exercise must be taken into account.