Diabetic polyneuropathy: effectiveness of Actovegin
I.A. LINES
1 Doctor of Medical Sciences, Professor,
A.S.
FOKINA 2, O.S.
FEDOROVA
3,
V.A.
GOLOVACHEV 1 1
Department of Nervous Diseases of the First Moscow State Medical University named after.
THEM. Sechenov 2
Department of Endocrinology, First Moscow State Medical University named after.
THEM. Sechenov 3
Federal State Budgetary Institution "Federal Bureau of Medical and Social Expertise", Moscow Diabetes mellitus (DM) is widespread throughout the world, for example, in the USA, DM was detected in 12% of the population aged 60 years and older, and in Europe in this age group - in 8–10%.
The prevalence of diabetes is constantly growing, outstripping the most pessimistic forecasts of the beginning of the century, and there is also a “rejuvenation” of type 2 diabetes. In diabetes, as a result of metabolic disturbances due to hyperglycemia and pathology of blood flow in the vessels of the microcirculatory system, various lesions are formed in most organs and systems of the body. The “classical” complications of diabetes include nephropathy, retinopathy and distal symmetric sensory-motor polyneuropathy (DPN), and DPN is most often detected in patients with diabetes [1]. Lesions of peripheral nerves in patients with diabetes are diverse, which is reflected in the classification of diabetic neuropathies [2]. The most common type of diabetic neuropathy is DPN (30–50% of patients with diabetes), other diabetic neuropathies (diabetic painful fine fiber polyneuropathies, diabetic amyotrophy, diabetic thoracoabdominal neuropathy, diabetic motor neuropathy, diabetic mononeuropathies) are observed much less frequently (1–3% of patients SD). S. Tesfaye et al. proposes the term “typical” diabetic polyneuropathy for DPN, and the term “atypical” for other variants of diabetic polyneuropathy (thin fiber) [3, 4]. This is hardly justified, since the term “typical” implies the most common variant of the disease, and the term “atypical” implies an unusual course, symptoms, and severity of the same disease, i.e., having similar pathophysiological mechanisms of development. At the same time, fine-fiber diabetic polyneuropathies have fundamentally different clinical manifestations, a different onset, different characteristics of objective research methods, the state of peripheral nerve function and, apparently, other mechanisms of formation [2, 5, 6]. Thus, we are talking about forms of diabetic polyneuropathies that are fundamentally different from DPN. Therefore, practitioners should not use thyremin “atypical diabetic polyneuropathy” at this time. It is more appropriate to keep the previous qualifying names: acute painful diabetic polyneuropathy (Ellenberg syndrome) and acute painful diabetic polyneuropathy associated with the normalization of carbohydrate metabolism.
DPN is most often encountered in the clinical practice of neurologists and endocrinologists; it develops slowly, has a subclinical phase, and in type 2 diabetes can be its manifest manifestation. Many patients with even quite severe damage to the peripheral nerves do not complain, and polyneuropathy can only be detected during a neurological examination and electrophysiological examination. DPN refers to the so-called. neuropathies that depend on the length of the nerves, so its phenotype is quite typical: positive and negative neuropathic symptoms always predominate in the legs, in the distal parts (fingers, feet, legs), and due to damage primarily to thin fibers, sensory disorders always dominate over motor ones. In the later stages of DPN, generalized damage to peripheral nerves is manifested by simultaneous damage to somatic (motor and sensory) and autonomic nerve fibers. According to the classification of DPN stages proposed by PJ Dyck [7], states with the absence of neuropathy are distinguished - N0, the subclinical phase of DPN, in which there are no positive and severe negative neuropathic symptoms, however, upon examination (EMG, quantitative sensory and autonomic testing) a dysfunction of somatic or autonomic nerves - N1, and stage N1 is also established in cases where there is any one symptom indicating trouble in the peripheral nerves (only a decrease in Achilles reflexes or only a decrease in one sensory modality). In the presence of typical patient complaints (pain, burning, numbness, paresthesia) and/or severe sensory neurological deficit, the stage of symptomatic DPN is determined - N2a, and if symptoms of involvement of motor fibers are detected in the clinic (the patient cannot stand or walk on his heels) - stage N2b . In the event that damage to the peripheral nerves leads to disruption of the social and work adaptation of patients (severe pain syndrome, diabetic foot, severe orthostatic hypotension), we are talking about stage N3. The diagnosis of DPN can only be made in patients with type 1 or type 2 diabetes established on the basis of international criteria. The average time for the development of DPN is about 9 years, therefore the early development of polyneuropathy should force one to exclude another nature of the formation of peripheral nerve pathology in patients. In approximately 10% of patients with diabetes, polyneuropathies of non-diabetic etiology are detected [8]. Diagnosis of DPN is based on identifying typical positive neuropathic symptoms (pain, burning, numbness, paresthesia), as well as positive neuropathic symptoms (decreased sensitivity of various modalities (primarily pain, temperature and vibration), decreased or absent tendon reflexes in the legs, primarily Achilles turn). Additional symptoms of damage to peripheral sympathetic fibers on the feet may be: dry skin, calluses, changes in temperature (increase) and skin color (redness). To objectively confirm damage to somatic nerve fibers, EMG is used, which reveals a decrease in excitation conduction velocity (ECV) along the motor (peroneal and tibial nerves) and sensory (sural) nerves of the legs, a decrease in the amplitude of motor and sensory responses, and an increase in residual latency. To identify damage to autonomic fibers, the study of heart rate variability using RR intervals at rest, during deep breathing, and during an orthostatic test is used; a study of the power spectrum of high and low frequencies of the ECG is also used during daily monitoring. To identify damage to the autonomic nerves of the extremities, a study of cutaneous evoked sympathetic responses is used. In DPN, there may be no responses or a significant prolongation of latency [6]. The most accurate way to judge the presence of DPN in patients with diabetes is the so-called method developed at the Mayo Clinic. compositional score – NIS LL (Neuropathy Impairment Score Low Limb – score of neuropathic symptoms in the legs) + 7 electrophysiological tests [11]. In recent years, the earliest method for detecting pathology of peripheral nerves in patients with diabetes is considered to be confocal microscopy of thin corneal nerves and biopsy of the skin of the foot with examination of the condition of thin epidermal fibers. Risk factors for the development of DPN include poor glycemic control, type 1 and duration of diabetes, excess weight, and arterial hypertension, age, smoking, dyslipidemia, and low insulin and C-peptide levels may also play a role. Intensive therapy of patients with type 1 diabetes with insulin can reduce the risk of developing vascular disorders and DPN, although it cannot completely eliminate its occurrence or lead to a serious regression of symptoms [14]. A review of prospective studies of the effect of glycemia on DPN emphasizes that long-term maintenance of normoglycemia in patients with type 1 diabetes can improve the function of somatic and autonomic nerves. In type 2 diabetes, no convincing data have been obtained on the possibility of reducing the risk of developing DPN with intensive insulin therapy. At the same time, there is no doubt that good control of diabetes is a priority in preventing the development of DPN and ensuring maximum effectiveness of its pathogenetic therapy.
In 2001, M. Brownlee, in an article published in the journal Nature, summarized experimental and clinical data on the molecular and biochemical basis of the pathogenesis of DPN. In 2005, M. Brownlee summarized the results of experimental and clinical studies of the pathogenesis of late complications of diabetes in the Benting Lecture [9, 10]. According to modern concepts, in the formation of the pathological process in nerve fibers, endothelium and the vascular wall in DPN, the leading role is played by the blockade of the hexoseamine pathway of glucose utilization with the accumulation of intermediate products of glucose metabolism, in particular, glucose-6-phosphate and glyceraldehyde-3-phosphate. An increase in the concentration of metabolic intermediate products triggers the activation of protein kinase C and the formation of a large number of AGEs (Advanced Glycated end products), which leads to disruption of endothelium-dependent reactions and the function of nerve cell structures, for example, axoplasmic flow. The reason for the blockade of glucose metabolism is the activation of special polymerases (PARP), which occurs in response to the destruction of mitochondrial DNA by superoxide. Oxidative stress, the cause of which in diabetes is the formation of a large number of free radicals against the background of the weakness of one’s own antioxidant system (decreased content of antioxidant enzymes), is responsible for impaired glucose metabolism in the cytoplasm of cells. This theory is supported by facts confirming the dependence of the timing of development of DPN in patients with diabetes on the polymorphism of certain genes. An association was found between the timing of development of DPN and the polymorphism of the mitochondrial and endothelial superoxide dismutase genes and the PARP gene, which is in good agreement with the idea of the leading role of mitochondrial superoxide in the formation of late complications of diabetes [12].
Damage to endoneurial vessels in diabetes occurs as a result of metabolic disorders, but later begins to play an independent role in the formation of pathology of peripheral nerves. It has been shown that there is a correlation between the number of nerve fibers in the peripheral nerve and the wall thickness of the endoneurial vessels in diabetes and, thus, the vascular component is fundamental for the development of DPN [13]. In the apt expression of A.S. Efimova, “diabetes begins as a metabolic disease and ends as a vascular pathology” [27], which must be taken into account when prescribing pathogenetic therapy to patients with DPN.
Treatment of DPN is based on the use of drugs that act on the pathogenetic mechanisms of its formation, symptomatic treatment, for example, the use of pain medications (anticonvulsants, antidepressants, local anesthetics, opioids), prevention of late complications and, if possible, exclusion of risk factors for their development. Pathogenetic therapy of DPN is determined by modern ideas about the mechanisms of formation of late complications of diabetes, emphasizing the relationship of metabolic and vascular factors, which has been repeatedly considered in the literature. In this regard, the possibilities of using: 1) aldose reductase blockers to reduce the utilization of glucose through the polyol pathway are discussed; 2) γ-linolenic acid preparations to normalize the metabolism of essential fatty acids and the synthesis of prostaglandins; 3) vasodilators and prostaglandin analogues, which help reduce hypoxia and increase endoneurial blood flow; 4) protein kinase C inhibitors to improve endothelium-dependent reactions of the vascular wall; 5) nerve growth factors; 6) inhibitors of the formation and accumulation of advanced glycation end products AGEs, 7) antioxidants, thiamine. Currently, the main drugs that have proven their effectiveness in DPN are antioxidants, Actovegin and thiamine.
Pathogenetic therapy of DPN is determined by modern ideas about the mechanisms of formation of late complications of diabetes, emphasizing the relationship of metabolic and vascular factors, which has been repeatedly considered in the literature. In this regard, the possibilities of using: 1) aldose reductase blockers to reduce the utilization of glucose through the polyol pathway are discussed; 2) γ-linolenic acid preparations to normalize the metabolism of essential fatty acids and the synthesis of prostaglandins; 3) vasodilators and prostaglandin analogues, which help reduce hypoxia and increase endoneurial blood flow; 4) protein kinase C inhibitors to improve endothelium-dependent reactions of the vascular wall; 5) nerve growth factors; 6) inhibitors of the formation and accumulation of advanced glycation end products AGEs, 7) antioxidants, thiamine. Currently, the main drugs that have proven their effectiveness in DPN are antioxidants, Actovegin and thiamine.
The main antioxidant drug used to treat DPN is α-lipoic (thioctic) acid (ALA), which is a powerful natural fat-soluble antioxidant. The effectiveness of ALC in DPN has been shown in a number of clinical studies conducted within the framework of evidence-based medicine, and confirmed by a meta-analysis of four studies on the effectiveness of ALC in DPN [15].
Another opportunity to influence the pathogenetic mechanisms of DPN formation is to influence the activity of the transketolase enzyme. This enzyme is able to reduce the pathological accumulation of intermediate products of glucose metabolism. Enzyme activity directly depends on the concentration of thiamine. In 2003, the hypothesis about the ability of thiamine to reduce the severity of metabolic disorders caused by hyperglycemia was confirmed in an experimental study that showed the ability of thiamine to activate transketolase and prevent vascular damage to the retina in diabetes [16, 17].
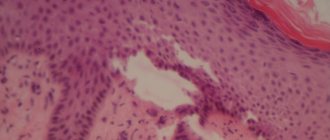
In recent years, data have been obtained on the effectiveness of treatment of DPN with Actovegin. The drug Actovegin from Takeda (Japan) contains highly purified hemodialysate obtained by ultrafiltration from the blood of calves. The drug contains organic low-molecular compounds, which eliminates the development of prion diseases, such as Creutzfeldt-Jakob disease, when Actovegin is administered into a human vein. The technology for producing Actovegin excludes the presence of protein components that have antigenic and pyrogenic properties. Actovegin is a mixture of natural substances of inorganic (electrolytes - sodium, potassium, calcium, magnesium, chlorides, nitrogen compounds) and organic (acetate, lactate, amino acids, nucleosides, glycosphingolipids, intermediate products of carbohydrate and fat metabolism, antioxidant enzymes). There is no exact data on the pharmacokinetics of Actovegin, since it is a multicomponent drug, and its composition includes substances originally contained in the human body. The production method of Actovegin and the discussion of studies on the mechanisms of its action are discussed in detail in reviews devoted to the almost half-century history of this drug [18, 23]. It is known from experimental work that Actovegin’s activation of glucose uptake into cells begins 5 minutes after intravenous administration of the drug and the peak of its action is detected after 120 minutes. It is currently believed that the insulin-like effect of Actovegin and stimulation of glucose metabolism are associated with inositol phosphooligosaccharides contained in the drug. Due to the fact that Actovegin modulates the activity of intracellular glucose transport, lipolysis is activated [19]. The antihypoxic effect of Actovegin is associated with its ability to increase the absorption of oxygen by tissues, which increases the resistance of cells to hypoxemia [20, 21]. As a result of the supply of oxygen to tissues, the formation of macroergic phosphates (ATP, ADP) increases, oxidative phosphorylation enzymes are activated, the synthesis of carbohydrates and proteins and the breakdown of anaerobic glycolysis products (lactate) are accelerated, and cellular energy imbalance is reduced. An increase in oxygen absorption by the vascular wall with the administration of Actovegin leads to normalization of endothelium-dependent reactions and a decrease in peripheral vascular resistance. As a result, the formation of high-energy phosphates in cellular structures increases. The improvement in blood flow in the microcirculation system under the influence of Actovegin, associated with the normalization of endothelium-dependent reactions (vasodilation) and a decrease in peripheral vascular resistance, reflects an increase in oxygen metabolism of the vascular wall. The antioxidant effect of Actovegin is ensured by the presence of superoxide dismutase in the drug, which is confirmed by atomic emission spectrometry, as well as magnesium ions, which increase the activity of glutathione synthetase, which converts glutathione into glutamine [22] (Fig. 1).
A recent study by MW Elminger revealed that Actovegin reduces apoptosis (based on caspase-3 activity), increases the number of synaptic connections and dose-dependently reduces oxidative stress in neurons [24]. In a study by A. Dieckmann et al. It was found that Actovegin improves the conduction of excitation along sensory fibers and reduced apoptosis in sciatic nerve fibers by reducing PARP activity, which emphasizes the influence of Actovegin on the pathogenetic mechanisms of the formation of cellular damage in diabetes [25]. Actovegin is used in the form of a 10 or 20% solution for intravenous (in 250 ml of saline) or intramuscular administration or 200 mg tablets for oral administration.
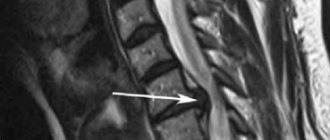
Side effects of the drug mainly include rare allergic reactions. In the literature there is a description of only one case of anaphylactic shock after intravenous administration of the drug with the development of liver and kidney damage, but not in a patient treated by a doctor, but in an athlete [26]. In this regard, one can think that medical standards were violated when administering the drug. Interest in the use of Actovegin in DPN is due to the fact that the drug has antioxidant properties and the ability to improve the utilization of oxygen and glucose into cells, which is extremely important in diabetes, when energy deficiency forms in the tissues, associated with both the phenomenon of pseudohypoxia and true hypoxia ( Fig. 2).
In the work of V.A. Yavorskoy et al. in an open study, Actovegin was used for the treatment of DPN in 24 patients with type 1 and type 2 diabetes in the form of daily infusions for 20 days. An improvement in the clinical condition of patients was noted in the form of a decrease in pain, improved sensitivity and tendon reflexes, and an increase in muscle strength. Rheovasography showed an improvement in blood flow in the legs, and an EMG examination showed an increase in the amplitude of the M-response and SRV when stimulating the nerves of the legs [28]. The use of Actovegin in the complex treatment of 33 patients with diabetic foot syndrome of varying severity according to the Wagner classification showed in an open study that the connection of the drug to traditional treatment contributed to the rapid relief of pain and the acceleration of the processes of granulation and epithelization of ulcerative defects with their healing [29].
In a study by F.E. Morgoeva et al. The effectiveness of intravenous monotherapy with Actovegin in patients with type 2 diabetes was studied in an open study [30]. The group of 30 patients who received Actovegin once a day intravenously at a dose of 400 mg diluted in 200.0 ml of physiological solution for 3 weeks (15 infusions) included patients with a duration of diabetes of at least 10 years at the age of 58.94 ± 1.29 years (9 men and 21 women). Before treatment, in the group of patients with diabetes with DPN, a significant increase in the level of lipid peroxidation in plasma and erythrocyte membranes was observed compared with a group of 15 healthy volunteers of the same age, which indicated the severity of oxidative stress. Treatment with Actovegin led to a decrease in the level of malondialdehyde (MDA) in plasma and erythrocyte membranes with its normalization. Thus, Actovegin had an undoubted antioxidant effect, acting on the pathogenetic mechanisms of the development of DPN. The state of the rheological properties of blood was assessed by computer capillaroscopy before and after treatment with Actovegin. After treatment with Actovegin, a significant improvement in the main characteristics of capillary blood flow was noted, not only reflecting the rheological properties of the blood, but also the state of permeability of the capillary wall. A clinical study showed a significant decrease in positive and negative neuropathic symptoms (p < 0.05) after treatment with Actovegin. When studying the functional state of the sensory nerve, a significant increase in the amplitude of the sensory response was revealed (3.87 ± 2.43 μV before treatment and 6.19 ± 3.16 μV after treatment, p < 0.05) with the SRT unchanged.
A study of temperature and pain sensitivity thresholds using quantitative sensory testing showed that after treatment with Actovegin, there is a decrease in sensitivity thresholds associated with the state of thin nerve fibers (p < 0.05). Thus, the study showed that treatment with Actovegin, reducing the severity of oxidative stress and improving the state of the microcirculation system, leads to a regression of the clinical manifestations of DPN in patients with type 2 diabetes, which is confirmed by an improvement in objective indicators of the functional state of peripheral nerves.
W. Jansen and E. Beck studied the effect of oral administration of Actovegin on patients with DPN in a controlled study: one group of 35 patients received placebo, another group of 35 patients received Actovegin tablets (600 mg 3 times a day) for 24 weeks [31]. The criteria for assessing the effectiveness of the drug were clinical characteristics of polyneuropathy (tendon reflexes, superficial and deep sensitivity, intensity of pain) and EMG indicators of peripheral nerve function (velocity of propagation of excitation (RPV), as well as the distance that patients could walk without pain. Improvement in the condition of patients in Actovegin treatment group was observed in the majority of patients 8 weeks after the start of treatment, and the optimal effect was achieved after 16 weeks of treatment (Fig. 3).A significant improvement during treatment with Actovegin compared to the placebo group was shown in almost all clinical indicators: pain-free walking distance, tendon reflexes, superficial and deep sensitivity (p < 0.01). SRV significantly (p < 0.001) increased in the treatment group compared to the placebo group. Patients in the treatment group felt better and had fewer complaints about a violation of the psycho-emotional state, which correlated with improving their physical condition.
In 2009, the results of a multicenter, randomized, double-blind, placebo-controlled study of the treatment of patients with type 2 diabetes with DPN with Actovegin were published [32]. A multicenter, double-blind, placebo-controlled, randomized, parallel-group clinical trial was conducted at 26 clinical sites in Russia, Ukraine, and Kazakhstan. The purpose of the study was to evaluate the clinical efficacy and safety of Actovegin compared to placebo in patients with type 2 diabetes and clinical manifestations of peripheral diabetic polyneuropathy after intravenous infusions of Actovegin or placebo followed by switching to Actovegin tablets. A total of 567 patients were included in the study. 281 patients first received 20 intravenous infusions of Actovegin (250 ml of a 20% solution - 2.0 g), and then for 140 days the patients received Actovegin tablets 600 mg 3 times a day (1,800 mg/day). 286 diabetic patients with DPN received intravenous placebo therapy followed by placebo tablets. Inclusion criteria were: diagnosis of type 2 diabetes, age 18–65 years, glycated hemoglobin level below 10%, presence of clinical manifestations of DPN, that is, TSS score ≥ 6 points and NIS-LL ≥ 2 points, vibration sensitivity threshold ≤ 30V, adequate blood supply to the foot, proven by the presence of pulses in the posterior tibial artery and dorsalis pedis artery. The main criteria for the effectiveness of the drug in this study were positive neuropathic symptoms, which were assessed on the TSS scale, and the vibration sensitivity threshold, which was tested at several points on the legs (ankle, toes) using a biotensiometer. Secondary efficacy criteria included individual TSS scores, NIS LL scores, and quality of life scores (short scale - SF 36).
The best results were noted in relation to positive neuropathic symptoms, and improvement was noted both in the total assessment of all symptoms and in relation to each specific symptom. A significant decrease in sensory neurological deficit was revealed; in relation to changes in reflexes and muscle strength, a positive trend towards improvement was noted, which did not reach the degree of reliability. This may be due to the fact that reflexes and especially muscle strength were altered in a relatively small number of patients. Objective indicators of the state of proprioceptive nerve fibers were assessed by assessing vibration sensitivity thresholds. The decrease in the vibration sensitivity threshold was highly significant when using Actovegin compared to placebo (Fig. 4). Throughout the study, fasting glucose levels and 2-month diabetes compensation (HbA1c) were measured. The results obtained indicate that the effectiveness of Actovegin is associated with the effect of the drug, and not with changes in diabetes control.
There were no significant side effects noted in the study. A total of 386 reports of adverse events were received from 192 patients (Actovegin - 186, placebo - 198). The most common adverse events were headache (Actovegin - 22, placebo - 19), hypoglycemia (21/19), hypertension (10/13), hyperglycemia (6/16), increased blood pressure (7/11) and respiratory infections paths (8/5). There were 21 serious adverse events reported, of which 10 occurred in 7 patients receiving Actovegin and 11 in 10 patients receiving placebo. Causality was considered possible for 1 serious adverse event (Actovegin: heart failure) and probable for 1 (placebo: hypersensitivity). No patients died during the study.
This study, conducted within the framework of (GCP - Good Clinical Practice), answered positively the question of the effectiveness and safety of the use of Actovegin for the treatment of DPN. It was concluded that sequential intravenous and then oral therapy with Actovegin for 160 days improved symptoms of neuropathy, reduced the threshold of vibration sensitivity and improved sensory function in patients with type 2 diabetes and diabetic polyneuropathy. A significant improvement in the quality of life (on a mental health scale) was shown in the Actovegin group compared to placebo. It was noted that the groups of patients receiving Actovegin and placebo had a comparable safety profile.
Thus, from a pathophysiological point of view, there is no doubt that Actovegin, which has antihypoxic and antioxidant effects, can be used for DPN, as well as a wide range of diseases of the central and peripheral nervous system, in the pathogenesis of which hypoxia, ischemia and oxidative stress play a role.
Literature
1. Strokov I.A., Melnichenko G.A., Albekova Zh.S. and others. Prevalence and risk factors for the development of diabetic polyneuropathy in inpatients with type 1 diabetes mellitus // Neuromuscular diseases. – 2012. – No. 1. – pp. 25–31. 2. Boulton AJM, Vinic AI, Arezzo JC et al. Diabetic neuropathies: a statement by the American Diabetes Association // Diabetes Care 2005; 28:956–962. 3. Tesfaye S, Boulton AJM, Dyck PJ et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments // Diabetes Care 2010; 33(10): 2285–2293. 4. Khramilin V.N. Diabetic polyneuropathy. Review of modern recommendations // RMD. Endocrinology 2012; 32:1580–1582. 5. Archer AG, Watkins PJ, Thomas PK et al. The natural history of acute painful neuropathy in diabetes mellitus // J Neurol Neurosurg Psychiatry 1983; 46:491–499. 6. Strokov I.A. Diabetic neuropathy // Diabetes mellitus type 2. Problems and solutions. GEOTAR-Media 2011. – pp. 506–529. 7. Dyck PJ Detection, characterization and staging of polyneuropathy: appreciated in diabetic. Muscle Nerve. 1998; 11(1): 21–32. 8. Dyck PJ, Davies JL, Wilson DM et al. Risk factors for severity of diabetic polyneuropathy: intensive longitudinal assessment of the Rochester Diabetic Neuropathy Study cohort // Diabetes Care 1999; 22: 1479–1486. 9. Brownly M. Biochemistry and molecular cell biology of diabetic complications // Nature. – 2001. – Vol. 414 – P. 813–820. 10. Brownlee M. The pathobiology of diabetic complications. A unifying mechanism. Diabetes 2005; 54:1615–1625. 11. Dyck PJ, Davis JL, Litchy WJ et al. Longitudinal assessment of diabetic polyneuropathy using a composite score in the Rochester Diabetic Neuropathy Study cohort. Neurology 1997; 49: 229–239. 12. Nikitin AG, Chudakova DA, Strokov IA et al. Leu54Phe and Val762Ala polymorphisms in the poly(ADP-ribose)polymerase-1 gene are associated with diabetic polyneuropathy in Russian type 1 diabetic patients.Diabetes Res Clin Pract 2008; 79(3):446–452. 13. Dyck PJB, Dyck PJ Diabetic polyneuropathy. In Dyck PJ, Thomas PK ed. “Diabetic polyneuropathy”, 2nd ed, Philadelphia, Pa: WB Saunders 1999: 255–278. 14. DCCT Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329:977–986. 15. Ziegler D., H.-J. Tritschler, Strokov I.A., Ametov A.S. Treatment of diabetic polyneuropathy with thioctic acid (literature review) // Farmateka. – 2008. – No. 17. – pp. 28–35. 16. Strokov I.A., Akhmedzhanova L.T., Solokha O.A. The use of high doses of B vitamins in neurology // Difficult patient. – 2009. – No. 10. – pp. 17–22. 17. Strokov I.A., Strokov K.I., Albekova Zh.S. Thiamine and benfotiamine in the treatment of late complications of diabetes mellitus // Doctor.Ru. – 2009. – No. 6 (2). – pp. 14–18. 18. Buchmayer F., Pleiner J., Elminger MW et al. Actovegin®: a biological drug for more than 5 decades // Wien Med Wochenschr – 2011 – Vol. 161 (3–4) – P. 80–88. 19. Jacob S., Dietze GJ, Machicao F. et al. Improvement of glucose metabolism in patients with type II diabetes after treatment with hemodialysate // Arzneimittelforschung. – 1996. – No. 3. – P. 269–272. 20. Kuninaka T, Senga Y, Senga H, Weiner M. Nature of enhanced mitochondrial oxidative metabolism by a calf blood extract. J Cell Physiol. 1991; 146(1): 148–155. 21. Reichel H., Weiss C., Leichweiss HP The effects of a blood extract on the oxygen uptake of isolated artificially perfused kidney and skeletal muscles in rats //Arzneimitte-Forschung / Drug Research 1968; 18: 1019–1021. 22. Nordvik B. Mechanism of action and clinical use of the drug Actovegin // In collection. “Actovegin. New aspects of clinical application". M., 2002 – pp. 18–24. 23. Machicao F., Mureanu DF, Hundsberger Y. et al. Pleiotropic neuroprotective and metabolic effect of Actovegin // Neuromuscular diseases. – 2012. – No. 4. – P. 3–10. 24. Elminger MW, Kriebel M., Ziegler D. Neuroprotective and anti-oxidative effects of the hemodialysate actovegin on primary rat neurons in vitro // Neuromolecular Med 2011; 13(4): 266–274. 25. Dieckmann A., Kriebel M., Andriambeloson E. et al. Treatment with Actovegin® improves sensory nerve function and pathology in streptozotocin-diabetic rats via mechanisms involving inhibition of PARP activation // Exp Clin Endocrinol Diabetes 2011; 120(3): 132–138. 26. Mailo L. Anaphylactic shock with multiorgan failure in a cyclist after inravenous administration of Activegin // Ann Intern Med 2008; 148–407. 27. Efimov A.S. Diabetic angiopathy. M.: Medicine, 1989. 28. Yavorskaya V.A., Egorkina O.V., Mashkin O.N. and others. Clinical experience with the use of Actovegin in diabetic polyneuropathy // In the collection. “Experience in the clinical use of Actovegin in endocrinology” M. 2005: 27–30. 29. Obolensky V.N. Complex treatment of patients with diabetic foot syndrome // In collection. “Experience in the clinical use of Actovegin in endocrinology” M., 2005: 39–46. 30. Morgoeva F.E., Ametov A., Strokov I.A. Diabetic encephalopathy and polyneuropathy: therapeutic possibilities of Actovegin // Russ. honey. magazine – 2005. No. 6. – pp. 302–304. 31. Jansen W., Beck E. Treatment of diabetic polyneuropathy. Controlled double-blind study // In collection. "Experience in the clinical use of Actovegin in endocrinology." – M., 2005. pp. 11–20. 32. Ziegler D., Movsesyan L., Mankovsky B. et al. Treatment of symptomatic polyneuropathy with actovegin in type 2 diabetic patients // Diabetes Care 2009; 32(8): 1479–1484.
New aspects of the use of Actovegin: from mechanisms of action to clinical effects
The results of studies evaluating the effect of the drug Actovegin on the functional activity of the microvascular endothelium, in particular the functional state of the microvascular smooth muscle apparatus, are presented. Due to its endothelial protective properties, Actovegin can be used to correct endothelial dysfunction in neurological, therapeutic, endocrinological and surgical patients.
Currently, the universality of the mechanisms of cell damage under various types of pathological influences has been proven. The final link in inflammation, ischemia, and stress is a violation of redox reactions, metabolism and energy supply to cells [1]. Today, neuroprotection, neuroplasticity and neurogenesis are considered fundamental neurobiological processes that participate in the implementation of endogenous protective activity, resist pathophysiological damaging mechanisms and stimulate endogenous recovery [2].
The classical concept of neuroprotection involves suppression of individual pathophysiological mechanisms of damage when using an appropriate drug [3]. Impaired transport and utilization of glucose is one of the leading pathogenetic mechanisms of cell apoptosis. The action of various drugs is aimed at enhancing the delivery of glucose into cells, inhibiting the oxidation of long-chain fatty acids in mitochondria and indirectly enhancing the oxidation of glucose. This leads to an increase in the synthesis of adenosine triphosphate and the neutralization of oxygen radicals, the production of which increases under ischemic conditions [4].
Today, one of the best approaches to neuroprotection is the use of pleiotropic drugs. Pleiotropic action involves a simultaneous modulating effect on various damaging pathological mechanisms (hypoxia, oxidative stress, excitotoxicity, inflammation, apoptosis and many others) [3]. The drug of biological origin Actovegin has these properties.
Actovegin is a highly purified, protein-free derivative of calf blood, obtained by ultrafiltration and consisting of more than 200 biological substances. The molecular weight of the organic compounds that make up the drug does not exceed 5000 daltons [5]. The main components of Actovegin are amino acids, biogenic amines and polyamines, sphingolipids, hexoses, eicosanoids, succinate, choline, vitamins, adenosine monophosphate, inositol phosphooligosaccharides, as well as macroelements (magnesium, sodium, calcium, phosphorus) and neuroactive microelements (silicon, copper). The macro- and microelements that make up Actovegin are part of neuropeptides, enzymes and amino acids, and therefore are recognized and absorbed by neurons much better than macro- and microelements that enter the body in the form of salts.
The metabolic effect of Acto-vegin consists primarily of enhancing the utilization of oxygen and the transfer of glucose into cell mitochondria. Various experimental models have shown that Actovegin, by influencing oxidative phosphorylation in mitochondria, increases oxygen production by cells by almost 40% [6, 7]. In addition, Actovegin is able to enhance the transport of glucose into the cell. It was found that the active fraction of the drug, including inositol phosphooligosaccharides, activates the transport of glucose into the cell through the activation of transport proteins (GLUT1, GLUT4), without involving insulin receptors. This is of great clinical importance, for example, in type 2 diabetes mellitus against the background of insulin resistance [8].
Actovegin has a neuroprotective effect and, in particular, has a pronounced antioxidant effect. According to in vitro data, Actovegin improves metabolism in cells, increases the number of neuronal synapses, reduces the level of markers of apoptosis induction (caspase 3) and the formation of reactive oxygen species in cells. These effects are dose-dependent [9, 10]. Similar results were obtained in recent experimental work.
MM. Yurinskaya et al. (2014) found that the use of Actovegin leads to a decrease in apoptosis of human neuroblastoma cells induced by hydrogen peroxide and suppression of intracellular signaling pathways involved in the mechanism of cell death [11].
L.G. Khaspekov et al. (2014) [12], studying the protective effect of Actovegin in a model of glutamate toxicity, found that the drug at a dose of 1 mg/ml has a neuroprotective effect, expressed in a decrease in cell death and most likely associated with the action of glutamate in rat cerebellar neurons.
Actovegin also demonstrated a neuroprotective effect in severe neuropathy in a model of streptozotocin-induced diabetes in rats. According to A. Dieckmann et al. (2011), Actovegin significantly improved conductivity in sensory nerve fibers and reduced the activity of poly-ADP-ribose polymerase, a nuclear enzyme whose excessive activation can trigger cell death processes in conditions such as cerebrovascular diseases and diabetic polyneuropathy [13].
In a study by S. Mielin et al. (2014) on a model of total cerebral ischemia in rats with occlusion of four main arteries of the brain, Actovegin contributed to better survival of neurons in the CA1 zone of the hippocampus compared to placebo [14]. This observation was accompanied by a large number of surviving individuals in the Actovegin group and significantly better results in the Morris water maze test.
In addition to Actovegin’s ability to improve cellular metabolism and have a neuroprotective effect, a number of studies have noted the drug’s effect on the microvascular endothelium.
In a pilot study by A.A. Fedorovich on 28 healthy volunteers, it was revealed that Actovegin has a direct endothelial protective effect at the level of the microvascular bed [15]. The obtained results were subsequently confirmed in a population of patients with obliterating diseases of the arteries of the lower extremities, as well as with arterial hypertension.
According to the results of another study, intravenous infusions of Actovegin improved microcirculation parameters due to the endothelial protective effect and had a positive effect on the course of the disease. Patients receiving the drug were able to walk longer distances without pain [16].
The effectiveness of the drug was assessed in patients with arterial hypertension and moderate vascular cognitive impairment. Despite adequate lipid-lowering and antihypertensive therapy with the achievement of target blood pressure levels, cognitive disorders persisted in the comparison group (decrease in voluntary attention indicators), while in the Actovegin group it was possible to level out the cognitive deficit. In addition, during Actovegin therapy, a significant increase in the number of functioning capillaries at rest was noted, that is, a decrease in the elements of functional rarefaction of the microvasculature observed in patients with arterial hypertension [17].
V.V. Zakharov and V.B. Sosnin assessed the therapeutic effect of Actovegin on cognitive functions in patients with type 2 diabetes mellitus [18]. The patients were divided into two subgroups: the first - with the presence of concomitant arterial hypertension, signs of coronary heart disease and hemodynamically significant stenosis of the carotid arteries, the second - with the absence of the above pathology. After a three-month course of therapy, the greatest dynamics in indicators of concentration, short-term memory, visual-motor coordination and regulation of mental activity were observed in the group of patients in whom diabetes was combined with other clinically significant cardiovascular risk factors. Cognitive impairment in this category of patients, along with other factors, is based on tissue hypoxia caused by micro- and macrovascular damage. It is likely that Actovegin may have an additional positive effect in vascular cognitive disorders associated with damage to small vessels by improving microcirculatory parameters.
Thus, based on a number of experimental and clinical data, we can conclude that Actovegin, having many positive effects (antihypoxic, metabolic, neuroprotective and endothelial protective), is one of the promising drugs for the correction of hypoxic-ischemic damage, endothelial dysfunction, and microcirculatory disorders. Actovegin can be recommended as the drug of first choice for neurological and therapeutic patients: with acute or chronic cerebral ischemia and concomitant cardiovascular diseases, diabetes mellitus complicated by diabetic polyneuropathy, moderate and severe cognitive impairment in persons who have suffered a stroke. Therapeutic regimens used for the use of Actovegin in chronic ischemic conditions: 10–20 ml (400–800 mg) per 200 ml of saline intravenously in a course of seven to ten days, then one or two tablets (200–400 mg) three times a day within one to two months. In the presence of mnestic-intellectual disorders in elderly people - up to 12 weeks, two to three tablets three times a day. Repeat courses after six to eight months.
Neuroprotection is defined as creating conditions for the neuron to adapt to new functional conditions and reduce damage to brain tissue. Currently, the universality of the mechanisms of cell damage in various pathological processes has been proven. The final link in these cases is a violation of redox processes, a violation of metabolism and energy supply to cells [16]. The use of pleiotropic drugs is considered a promising direction in neuroprotection. The pleiotropic neuroprotective effect involves a simultaneous modulating effect on various damaging pathological mechanisms - excitotoxicity, inflammation, apoptosis, oxidative stress, etc. [20].
Today, there are several pharmacological groups of drugs with neurometabolic action [15]. These include Actovegin; the features of clinical action and the mechanisms of its implementation have not yet received enough attention, which served as the basis for writing the proposed review.
Actovegin belongs to the group of drugs that activate metabolism without direct vasodilating effects [17]. It is a highly purified deproteinized hemodialysate obtained by ultrafiltration from the blood of young calves, which includes more than 200 biological substances [1]. Actovegin mainly consists of substances with low molecular weight, including amino acids, biogenic amines and polyamines, sphingolipids, hexoses, lactate, succinate, choline, vitamins, adenosine monophosphate and inositol phosphooligosaccharides [20]. The drug also contains macroelements - magnesium, sodium, calcium, phosphorus and neuroactive microelements - silicon and copper. One of the most important macronutrients is magnesium, which is part of many proteins and enzymes. In addition, magnesium is part of glutathione peroxidase, which takes part in the metabolism of H2O2, leading to the formation of glutathione [6, 8, 9].
Preclinical trials have shown that at the molecular level, Actovegin improves the uptake and utilization of oxygen and glucose [2, 10, 18]. Glucose transporters play an important role in neuronal homeostasis and glucose utilization, and changes in glucose homeostasis in the CNS lead to disruption of neuronal activity and cognitive functions, which is especially dangerous for the hippocampus, an area of the brain associated with learning and memory processes [20]. In an in vitro
P. Buchmayer et al. [18] it was shown that actovegin has a neuroprotective effect: when it is added to a neuron culture, the number of “living” neurons and synaptic contacts on their processes increases. Under ischemic conditions, actovegin improves metabolic balance by increasing glucose uptake and oxygen consumption by tissues [17, 18]. We are talking about the antioxidant and antiapoptotic mechanisms of action of actovegin, which underlie their neuroprotective properties, as well as its ability to influence neuroplasticity, neurogenesis, and the trophic function of the nervous system. It is the multicomponent nature of Actovegin that determines its pleiotropic neuroprotective mechanism of action and clinical effectiveness [20].
Before moving on to the presentation of clinical studies related to cerebrovascular diseases (CVD), we recall that one of the most common manifestations is impaired cognitive function. They include deficits in attention, concentration, decreased ability to quickly navigate in a changing environment; memory impairment, especially for current events; slowness of thinking processes, rapid exhaustion during intense mental work; narrowing the range of interests [15].
V. Jansen et al. [17] conducted a double-blind, placebo-controlled study of the therapeutic effect of Actovegin-Forte in the form of tablets (containing 200 mg of the active substance) on mnestic-intellectual abilities in patients with CVD. The study included 120 patients whose age was 60-72 years (average - 67 years); the average duration of the disease was 2.5 years. All patients were randomized into 3 groups: group 1 included 40 patients treated with Actovegin-Forte, 3 tablets 3 times a day; patients of the 2nd group (also 40 people) received placebo in the form of pills (2 pills 3 times a day or 3 pills 3 times a day); Group 3 (40 patients) took Actovegin-Forte 2 tablets 3 times a day. The duration of therapy was 12 weeks. The patients' condition was assessed before the start of therapy and then after 4, 8 and 12 weeks of treatment. When examining patients, a number of neuropsychological tests were used to assess mnestic-intellectual functions: a test to assess vocabulary; short syndromic test; Pauli test; Benton test; mosaic test; light flicker frequency analysis test. It was found that in the groups of patients treated with Actovegin, success in completing the task in the jigsaw test increased compared to placebo. By the end of the 12-week course of therapy with Actovegin, in comparison with placebo, the patients’ lack of concentration of thinking, attention and volitional disorders disappeared; mnestic-intellectual abilities in general have increased. The authors assessed the effectiveness of 12-week therapy with Actovegin-Forte at 92%, which served as a basis for recommending this drug for long-term outpatient treatment of elderly patients with CVD.
H. Letzel et al. [5] conducted a multicenter study of the effectiveness of Actovegin in 1549 elderly patients (average age 74.1 years) with impaired cerebral functions. Patients included in the study were prescribed Actovegin according to the standard regimen: 10 ml of Actovegin solution intravenously for 2 weeks, then 4 weeks of oral administration of Actovegin tablets (2 tablets 3 times a day). Patients were examined before the start of therapy, after 2 and 4 weeks of oral administration of the drug. After 4 weeks from the start of Actovegin therapy, in 80% of cases, an improvement in the general condition was noted: a decrease in the severity (or cessation) of headaches, dizziness, anxiety and fear, improvement in memory and concentration (according to psychological testing). In 10.9%, when using the drug parenterally, undesirable effects were observed (feelings of heat and nausea). Poor tolerability of the drug was noted in a small percentage (0.9%) of cases. The authors emphasize the importance of combination therapy - starting with intravenous Actovegin to achieve a quick and good response and then continuing it with oral pills. This therapy has been recommended for elderly patients with organic syndrome.
A.A. Fedorovich et al. [12, 13, 19] describe a number of studies that confirmed the effect of Actovegin on the vasomotor and metabolic activity of smooth muscle cells of the microvascular bed of the skin in humans. The authors infused 250 ml of Actovegin solution into the cubital vein of the left arm in doses of 1.0 g of dry matter and 2.0 g of dry matter at a rate of 2-2.5 ml/min for 120-130 minutes. On average, the increase in the amplitude of the endothelial (Ae) rhythm under the influence of the first dose of Actovegin was 75%, the contribution of the endothelium to the modulation of microblood flow increased by 30%, and the functional contribution to the overall level of tissue perfusion increased by 65%. When tested with a higher dose of Actovegin, the most pronounced increase in the activity of the microvascular endothelium was shown: the increase in AE in this group averaged 191%, and the contribution of the endothelium to the overall level of tissue perfusion was 163%. The maximum peak of drug activity after intravenous administration was observed in the interval of 2-6 hours. 2 hours after the end of the infusion, a slight but significant decrease in diastolic blood pressure and mean blood pressure was noted. These changes were noted against the background of a significant increase in all tone-forming links of microcirculation modulation (endothelial, neurogenic and myogenic), with the most significant increase observed in endothelial activity. The increase in the functional contribution of the endothelium to total tissue perfusion averaged 79%. The authors concluded that Actovegin not only has a pronounced metabolic effect, increasing the functional activity of the microvascular endothelium, but also affects the vasomotor function of microvessels, resulting in a significant improvement in the functional state of the smooth muscle apparatus of the microvessels.
Taking into account persistent hemodynamic cerebral insufficiency, Actovegin may be the drug of choice for the treatment of chronic CVD in patients with myocardial damage [11, 14]. Neuroendocrine imbalance in the form of activation of local neurohormonal systems and severe endothelial dysfunction initiates vascular remodeling processes: the thickness of the arterial walls increases and the lumen decreases. Changes in the microcirculatory bed in atherosclerosis of the cerebral arteries: reduction of the bed as a consequence of hypoxia and microvascular convolutes compensating for this hypoxia. Low cardiac output, asymptomatic cerebral microembolization, fluctuations in blood pressure with episodes of hypotension, and metabolic changes can cause cerebral disorders. Narrowing of the lumen of intracranial arteries, along with dysfunction of the endothelium and rigidity of the vascular wall, causes a chronic reduction in cerebral blood flow, the appearance of diffuse or focal changes in the brain substance and clinical signs of CVD. All of the above components of chronic cerebrovascular disorders are a direct indication for the prescription of the drug Actovegin. It is also important to emphasize that Actovegin has a satisfactory efficacy-safety ratio.
A number of clinical studies in recent years have confirmed the positive effect of Actovegin on cognitive function. As established by S.G. Bugrova [3], this applies primarily to mild and moderate cognitive impairment in vascular diseases. In the work of E.A. Derevyannykh et al. [4] revealed a broader effect of Actovegin not only on cognitive functions, but also on EEG and indicators of blood supply to the brain, as well as neurological manifestations of chronic cerebrovascular insufficiency. A.A. Skoromets and V.V. Kovalchuk [7], when comparing several drugs (actovegin, instenon, berlition, rheopolyglucin, gliatilin) in the process of rehabilitation of patients with ischemic and hemorrhagic stroke, found that in ischemic stroke all of the listed drugs have a positive effect, while in hemorrhagic stroke - only actovegin .