Cardiovascular diseases and their treatment in Russia
The Russian Federation, with a population of 146.6 million people, is the largest country in the world. Mortality from cardiovascular diseases (CVD) in the country is extremely high, and this group of pathologies is the main cause of death, accounting for ≈ 1 million (46%) of the total number of deaths per year.
At the end of the 20th century and the beginning of the 2000s, Russia faced a deep socio-economic crisis, accompanied by a sharp increase in mortality from cardiovascular pathology. However, from 2003 to 2021, there was a steady decline in the number of deaths due to CVD (≈ 3% annually), with CVD mortality falling by 51% over this entire period (see figure); in particular, mortality from coronary heart disease decreased by 45.8%, and from cerebrovascular diseases - by 60.1% [1].
Figure 1 | Age-standardized mortality trend, as well as the number of deaths due to cardiovascular pathology in Russia
Top graph: trends in age-standardized cardiovascular mortality rates for men and women in Russia from 1995 to 2021. Bottom graph: absolute number of deaths due to cardiovascular pathology in Russia for the period from 2014 to 2021. According to Rosstat (Federal State Statistics Service).
Russia is characterized by an extremely heterogeneous population in terms of social status, characteristics of the development of pathologies, dietary habits, as well as an uneven distribution of medical institutions in large areas with sparse population. The country's constitution guarantees universal health care. Medical care for cardiovascular pathology is provided at three levels: primary, specialized outpatient and specialized inpatient. The financial model of healthcare is mixed: 60% of costs are covered by state health insurance, and 40% by federal and regional budgets. Patients treated for acute cardiovascular pathologies are entitled to free medications for 12 months.
The main aspects of improving control of risk factors for cardiovascular diseases since 2008 are the promotion of healthy lifestyles and the prevention of non-communicable diseases. Russia has joined the World Health Organization Framework Convention on Tobacco Control. Since then, extensive smoking legislation passed in 2013 has imposed major restrictions, such as a complete ban on cigarette advertising, a 21% increase in tobacco taxes, and a ban on smoking in public places. In April 2021, a minimum price of 108 ₽ (≈ 1.5 US dollars) per pack of cigarettes was introduced, and the average price of a pack is currently 150 ₽ (≈ 2.1 US dollars). This has led to a significant reduction in smoking at the population level. In 2021, this legislation also extended to e-cigarettes. Such restrictions have led to a significant reduction in alcohol consumption and mortality associated with its use in Russia. Between 2003 and 2016, overall alcohol consumption decreased by 43% (from 20.4 to 11.7 liters per capita), in particular, strong alcoholic beverages by 67% (from 14.7 to 4.8 liters per capita population) and unregistered alcohol (i.e., artisanal production) by 48% (from 6.9 to 3.6 liters per capita). In 2021, a restriction was introduced on the content of trans fats < 2% in fat and oil products.
In 2013, nationwide screening for major noncommunicable diseases was launched. This program includes: a questionnaire for the presence of risk factors, measurement of blood pressure and heart rate, determination of total cholesterol and glucose, ECG and an assessment on the SCORE scale (from the English Systematic Coronary Risk Evaluation - to assess the risk of death from cardiovascular diseases in the next 10 years) for all adults. In high-risk groups, at the second stage, diagnostic tests and observation by cardiologists are carried out due to identified CVDs (15,750 certified specialists in Russia or 10.8 per 100,000 population), ≈ 90% of whom are women.
It should be noted that women constitute <15% of all practicing cardiologists in Western countries [2]. Such a significant gender gap with a predominance of women in medical professions is observed in Russia and in many countries of the former USSR, not only in cardiology: > 90% of endocrinologists, > 92% of pediatricians, rheumatologists and gastroenterologists, > 95% of neonatologists and clinical immunologists are women. Until recent changes to the professional standards of the specialty of cardiology, allowing cardiologists to obtain additional training and certification in cardiovascular imaging, vascular (coronary and systemic) interventions, and electrophysiology, cardiology was primarily a noninvasive subspecialty of internal medicine concerned with CVD. This is currently changing as more male graduates choose cardiology as their major; however, it will take time to close the above gap.
Government spending on healthcare accounts for 3.5% of Russia's gross domestic product, of which 5% is in the GCC. Particular attention is paid to emergency cardiac (and cardiac surgical) care, which leads to a marked improvement in the population's access to emergency interventions, pharmacoinvasive treatments and prehospital thrombolysis for acute coronary syndrome and cerebral circulatory emergencies. The rate of primary percutaneous coronary intervention increased from 8.7% (2005) to 71.3% (2013), and the average travel time to the nearest percutaneous coronary intervention center decreased from 73 minutes (2010) to 48 minutes (2015) [3]. In 2021, 161,300 cases of acute myocardial infarction were recorded, and the overall mortality rate for this pathology reached 36.8 per 100,000, the average hospital mortality rate was 11.2% (6.4% in Moscow).
Despite unprecedented advances in the prevention and treatment of CVD, Russia still faces serious challenges. The increase in life expectancy from 64.8 years (2002) to 73.4 years (2019), accompanied by a decrease in the birth rate (10.1 per 1000 in 2021), has led to an aging population with a consequent increase in the burden of disease and health care costs. Unaddressed problems include widespread poor lifestyle choices, poor control of risk factors and lack of primary prevention. The high prevalence of obesity and hypertension, as well as the increasing incidence of diabetes mellitus, are accompanied by relatively poor self-control of blood pressure (only 49.7% of patients receiving treatment achieve target values) and a high proportion of uncontrolled arterial hypertension and hyperglycemia (the prevalence of diabetes mellitus is 5. 4%, not diagnosed in 54%, treatment not received in at least 2.9%) [4].
Russia is a member of the World Health Organization and other international structures and actively cooperates with them in order to reduce the risk of CVDs and the burden of diseases. The Russian Society of Cardiology is an active member of the European Society of Cardiology and the World Cardiology Federation. The recommendations of the European Society of Cardiology are approved by the Russian Society of Cardiology and published in the leading Russian cardiology journal. The Russian Society of Cardiology works closely with the Ministry of Health on national recommendations.
The medical education system in Russia is regulated by the Ministry of Health and the Ministry of Education and Science. Graduates of medical universities can enroll in two-year fellowship programs (residency programs) in cardiology (100 government positions in 2021) and pediatric cardiology (65 government positions in 2021) at accredited hospitals. Contract training programs are also available on a paid basis. A comprehensive accreditation exam for the specialty is conducted by the Ministry of Health. Although a large number of cardiologists join the medical community every year, there remains a high demand for cardiologists, especially in primary care settings and remote areas of the country.
The new professional standard for the cardiology specialty, developed in 2021, introduces best training and education methods, and also provides a new curriculum for young doctors and researchers entering the arena of the fight against CVD. National and international periodicals remain the most important source of information; they are steadily being replaced by electronic sources of information such as PubMed, podcasts and interactive publications on social networks. Close integration of large universities and the Russian Academy of Sciences allows for breakthrough biomedical research and facilitates the translation of their results into clinical settings [5].
In conclusion, despite significant improvements in cardiac care in Russia in recent years, achieving sustainable reductions in CVD mortality and improving cardiovascular health in all people requires revolutionary innovation rather than incremental evolution. Large, sparsely populated areas create difficulties in providing adequate access to specialized cardiac care, especially for acute CVD. This is partly solved with the help of telemedicine and remote patient supervision, and in 2018, Russia adopted a federal law regulating the use of these technologies in healthcare. The global transformation of cardiac care must be driven by the introduction of information technology, mobile devices and applications into the healthcare system, as well as big data analytics.
Good news
In Kuban, mortality from diseases of the circulatory system is decreasing. According to statistics available to Scientific Research Institute-KKB No. 1, the coordinator of the implementation of the federal project “Combating Cardiovascular Diseases” throughout the region, 492 out of one hundred thousand people die in the region per year, which is 3% below the target set by the national project. Hospital mortality from myocardial infarction has decreased, and good results have been achieved in terms of reducing deaths from acute cerebrovascular accidents.
Who needs diagnostics
Everyone and always - that is, regularly.
Today, cardiologists have at their disposal effective methods of clinical, instrumental and laboratory diagnostics that allow them to identify risk factors and act on them in a timely manner. “It is imperative to examine glucose, creatinine, lipid spectrum, transaminases, uric acid in the blood once a year, perform an ECG (and for those involved in fitness and cardio training - an ECG with stress, 24-hour heart rate monitoring), and occasionally measure blood pressure in the morning after waking up , advises City Clinic specialist, cardiologist of the highest category, candidate of medical sciences Elena Leonidovna Shukhardina.
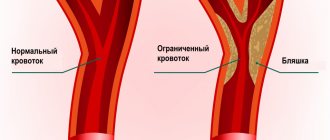
“The mandatory minimum is annual blood tests, including cholesterol and glucose levels, blood pressure monitoring, as well as an ECG,” says cardiologist at the WMT High Technology Clinic Elizaveta Andreevna Nemtsova. “Based on the results, doctors can prescribe more extensive examinations: ECG with physical activity, 24-hour ECG and/or blood pressure monitoring, transesophageal cardiac stimulation, ultrasound examinations of the vessels of the neck or extremities (to look for atherosclerotic plaques), heart (to assess valve function and heart function) or referral to a cardiovascular center for such diagnostics , such as computed tomography of the coronary (heart) vessels or coronary angiography.”
What depends on us
Risk factors for the development of CVD are divided into three groups: fatal, avoidable and social. We cannot influence the first ones: gender (men are more susceptible to cardiovascular diseases than women), age (over 55 years for men, over 65 years for women), early menopause in women (up to 40-45 years), family history predisposition. As for the second ones, they can be eliminated. “Increased levels of blood pressure, cholesterol, homocysteine, impaired carbohydrate metabolism, excess weight, sedentary lifestyle, stress, smoking and alcohol consumption contribute to the development of atherosclerosis, endothelial dysfunction and, as a consequence, myocardial ischemia - these factors are among those that we we can successfully influence,” explains cardiologist at the “Be Healthy” clinic, candidate of medical sciences Maria Valeryevna Aristova. As for social risk factors, they are theoretically conquerable, but only through collective efforts: these are urbanization, industrialization and economic backwardness of the population.
When is it time to go to the doctor?
There are signs that require immediate consultation with a cardiologist. These are compressive pain in the chest, a long recovery period after habitual exercises, arrhythmia, high blood pressure, shortness of breath, and attacks of severe weakness.
“In addition, it is worth discussing with a cardiologist the range of individual modifiable factors,” says City Clinic cardiologist Elena Leonidovna Shukhardina. “For example, do you need to constantly take pills if you have high blood pressure? Is it possible to change physical activity and lose weight? Do you really need to drink a lot of water or aspirin? Is it worth following the example of friends who are taking a cholesterol drug brought from a trip abroad, or can you do without pills altogether? All such questions can be answered by being examined by a cardiologist.”
The advisability of early contact with a doctor speaks for itself: with primary prevention, the risk of fatal complications is reduced by 75-85%.
What to do
Prevention of CVD can be primary or secondary. Secondary, called medicinal, is carried out differentially with groups of patients with confirmed cardiovascular diseases. Its main goal is to prevent relapses of diseases and the development of complications in people with existing risk factors, reduce morbidity and mortality from these diseases, and improve the quality of life of patients.
Primary prevention is exactly what those who are still healthy need. It is aimed at people at risk in whom clinical manifestations of the disease have not yet been observed, and consists of observing a work and rest schedule, increasing physical activity, giving up alcohol and smoking, and a balanced diet.
Harmonious work
The success of cardiologists in the Krasnodar region is facilitated by well-coordinated interaction with ambulance: if a patient with a heart attack is in a remote area, he is given thrombolysis at the stage of delivery to the cardiovascular center, so that upon arrival at the center he can immediately undergo angiography.
“The second part of the vascular program is medical examination and identification of patients at an early stage, when they have not yet reached a heart attack,” continues the chief cardiologist of the regional clinical hospital named after Ochapovsky. “This is also a huge job: the creation of offices and primary prevention departments in clinics of municipalities of the region . The medical prevention center with its network created in the districts is very helpful here.”
What and how to treat
In the Krasnodar region today, almost all advanced programs and procedures are used, including surgical treatment, up to heart transplantation.
“The region performs surgical correction of most congenital and acquired heart defects in adults and children, heart valve replacement, including minimally invasive, gentle procedures, while in children defects are detected at the stage of intrauterine screening,” says Elena Demyanovna, a cardiologist at the Zdrava clinic. Alexandrova.— In the region, surgical interventions on the vessels of the heart are performed through open (coronary artery bypass grafting) and intravascular (coronary angioplasty) approaches, including combined interventions. Operations are being carried out to radically treat cardiac arrhythmias.”
Detrimental
One of the most common triggers for heart attacks is stress. To overcome a stressful situation, the body strains all systems, especially the cardiovascular system. “Any stressful situations that lead to a rise in blood pressure, an increase in heart rate, or vascular spasm can provoke a heart attack if a person has coronary heart disease,” notes the head of the cardiology department of the emergency hospital in Krasnodar, the chief freelance cardiologist of the Krasnodar Ministry of Health edge Natalia Spyropoulos.— How to live with this and how to overcome the harmful effects of stress? We learn to alternate between relaxation and tension. We sleep enough time - for an adult this is from seven to nine hours every day. We load our body and brain. We try to think positively and see more good in any situation.”
People with a sedentary lifestyle and exercise less than 150 minutes per week have an increased risk of death from CVD. For those who achieve the recommended high range of physical activity of at least 300 minutes per week, this risk is virtually eliminated
Specialists at the KBL Health Recovery Center recommend using balneotherapy to reduce the negative impact of negative emotions on the body. “They do not cause side effects and not only calm the nervous system, but also trigger natural self-healing mechanisms,” says Svetlana Nikolaevna Anisimova, head physician of the KBL Health Restoration Center. “For example, our unique iodine-bromine baths have pronounced calming properties, since they inhibit the processes of excitation and have a sedative effect."
Dangerous
A risk factor for the development of CVD may be a breathing disorder such as OSA - obstructive sleep apnea syndrome. The first sign of this condition is snoring. OSA can become one of the main causes of heart attack, stroke, and arterial hypertension. “To identify this condition, a number of diagnostic procedures are used,” explains Vasily Evgenievich Myazin, a somnologist at the TS Clinic, a functional diagnostician of the highest category. “These are questionnaires, respiratory monitoring, and sleep endoscopy. The examination allows you to determine the cause of snoring and the severity of the collapse of the upper respiratory tract during medicated sleep. After the examination, I explain to the patient all the nuances of his condition and determine further tactics for his treatment. If the condition is uncomplicated, or if there is a slight deterioration in night breathing, a few simple measures are usually sufficient.”
There is only one center for the diagnosis and treatment of sleep disorders in Krasnodar; it operates on the basis of the TS Clinic.
Men need to monitor the state of their cardiovascular system from the age of 30
Photo: Alexander Chizhenok, Kommersant
Men need to monitor the state of their cardiovascular system from the age of 30
Photo: Alexander Chizhenok, Kommersant