Valz
Hyperkalemia
When used simultaneously with dietary supplements containing potassium, potassium-sparing diuretics, potassium-containing salt substitutes, or with other drugs that may cause an increase in potassium levels in the blood (for example, heparin), caution should be exercised and regular monitoring of potassium levels in the blood should be carried out.
Renal dysfunction
There is no experience of safe use in patients with creatinine clearance less than 10 ml/min and in patients on hemodialysis, so valsartan should be used with caution in such patients. In patients with CC more than 10 ml/min, no dose adjustment is required.
Liver dysfunction
In patients with mild or moderate hepatic impairment without cholestasis, valsartan should be used with caution.
Sodium deficiency in the body and/or decreased blood volume
In patients with severe sodium deficiency in the body and/or reduced blood volume, for example, those receiving high doses of diuretics, in rare cases, after starting therapy with valsartan, arterial hypotension may develop, accompanied by clinical manifestations.
Before starting treatment with Valz, it is necessary to adjust the sodium content in the body and/or replenish the blood volume, including by reducing the dose of the diuretic.
Renal artery stenosis
The use of the drug in a short course in patients with renovascular hypertension, which developed secondary to unilateral stenosis of the artery of a single kidney, does not lead to any significant change in renal hemodynamics, serum creatinine concentration or blood urea nitrogen.
However, given that other drugs that affect the RAAS may cause an increase in serum urea and creatinine concentrations in patients with bilateral renal artery stenosis or stenosis of the artery of a solitary kidney, monitoring these indicators is recommended as a precautionary measure.
Kidney transplant
There are no data on the safety of using Valz in patients who have undergone kidney transplantation.
Primary hyperaldosteronism
The drug is not effective for the treatment of arterial hypertension in patients with primary hyperaldosteronism, since activation of the RAAS is not observed in this category of patients.
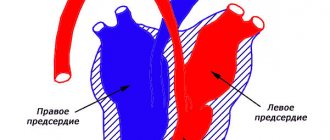
Aortic and mitral stenosis, obstructive hypertrophic cardiomyopathy
As with other vasodilating agents, caution should be exercised when taking Valz in patients with aortic or mitral stenosis and obstructive hypertrophic cardiomyopathy.
Pregnancy
Taking angiotensin II receptor antagonists is contraindicated during pregnancy. Patients planning a pregnancy should choose treatment with alternative medications that have a proven safety profile when used during pregnancy.
If pregnancy is diagnosed during treatment with Valz, it should be discontinued as soon as possible and alternative treatment prescribed (see sections “Contraindications” and “Use during pregnancy and breastfeeding”).
CHF/period after myocardial infarction
In patients with CHF or after myocardial infarction who begin treatment with valsartan, a slight decrease in blood pressure is often observed, and therefore it is recommended to monitor blood pressure at the beginning of therapy. If you follow the recommendations for changing the dosage regimen, there is usually no need to discontinue the drug due to arterial hypotension. Evaluation of patients with CHF should include assessment of renal function.
Due to inhibition of the RAAS, renal dysfunction may occur in some patients. In patients with CHF functional class II-IV according to the NYHA classification, treatment with ACE inhibitors and angiotensin II receptor antagonists may be accompanied by oliguria and/or an increase in azotemia and, in rare cases, the development of acute renal failure and/or death. Therefore, in these categories of patients, before using the drug Valz, as well as periodically during treatment, it is necessary to assess renal function.
Combination therapy for arterial hypertension
For arterial hypertension, the drug Valz can be used in monotherapy, as well as in combination with other antihypertensive drugs, in particular with diuretics.
Combination therapy in the period after myocardial infarction
It is possible to use the drug Valz in combination with other drugs used after myocardial infarction, namely: thrombolytics, acetylsalicylic acid as an antiplatelet agent, beta-blockers, HMG-CoA reductase inhibitors and diuretics. In this category of patients, it is not recommended to use Valz simultaneously with ACE inhibitors, since this combination therapy does not have advantages over valsartan or ACE inhibitor monotherapy in terms of overall mortality from any cause.
Combination therapy for CHF
For CHF, the drug Valz can be used both in monotherapy and simultaneously with other drugs - diuretics, cardiac glycosides, as well as ACE inhibitors or beta-blockers.
In this category of patients, the use of triple combination therapy with an ACE inhibitor, a beta-blocker and the drug Valz is not recommended.
Angioedema (Quincke's edema)
During treatment with valsartan, there have been reports of the development of angioedema, accompanied by swelling of the larynx and vocal cords, leading to airway obstruction, and/or swelling of the face, lips, pharynx and/or tongue. Some patients in this group had previously experienced angioedema while taking other medications, including ACE inhibitors.
If angioedema develops, Valz should be discontinued immediately, after which drugs containing valsartan should not be taken in the future.
Double blockade of the RAAS
When treated with drugs that affect the RAAS, especially when they were combined, a marked decrease in blood pressure, syncope, stroke, hyperkalemia and changes in renal function (including acute renal failure) have been reported in sensitive patients.
Caution is required when combining angiotensin II receptor antagonists, including valsartan, with other drugs that block the RAAS, such as ACE inhibitors or aliskiren.
Concomitant use of angiotensin II receptor antagonists, including valsartan, with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m body surface area) and is not recommended in other patients. Concomitant use of angiotensin II receptor antagonists with ACE inhibitors is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Other RAAS stimulation conditions (320 mg dose only)
In patients in whom renal function may be dependent on the activity of the RAAS (for example, patients with severe congenital heart failure), treatment with ACE inhibitors is associated with the occurrence of oliguria and/or progressive azotemia and, in rare cases, acute renal failure and/or death. Since valsartan is an angiotensin II receptor antagonist, it cannot be excluded that its use may be associated with impaired renal function.
Children and teenagers under 18 years of age
Renal dysfunction
The use of the drug has not been studied in patients aged 6 to 18 years with impaired renal function with creatinine clearance <30 ml/min, as well as in patients on hemodialysis, so its use in this group of patients is not recommended.
In patients from 6 to 18 years old with CC more than 30 ml/min, no dose adjustment is required. While taking Valz, renal function and serum potassium levels should be carefully monitored. In particular, these precautions must be observed when taking the drug Valz against a background of elevated temperature or decreased blood volume, since in this case the development of renal dysfunction is possible.
Liver dysfunction
As for adult patients, the use of Valz is contraindicated for patients from 6 to 18 years of age with severe liver dysfunction, biliary cirrhosis and cholestasis. Experience with the use of valsartan in patients with mild to moderate liver dysfunction is limited. The dose should not exceed 80 mg in this group of patients.
Valz tab 160mg N98 (Actavis)
In patients with severe sodium deficiency in the body and/or reduced blood volume, for example, due to taking diuretics in high doses, in rare cases, severe arterial hypotension may develop at the beginning of valsartan therapy. Before starting therapy with Valz, it is recommended to restore the electrolyte and fluid levels in the body, in particular by reducing the doses of diuretics. The drug Valz can be used in conjunction with other drugs intended for the treatment of myocardial infarction, such as thrombolytics, acetylsalicylic acid, beta-blockers, statins and diuretics. Concomitant use of ACE inhibitors is not recommended. In case of renovascular hypertension, regular monitoring of urea and creatinine levels in the blood is necessary. When used together with drugs containing potassium, its salts and drugs belonging to the group of potassium-sparing diuretics, regularly monitor the level of potassium in the blood plasma. In chronic heart failure, at the beginning of treatment with Valz, a slight decrease in blood pressure may be observed, so it is recommended to monitor blood pressure at the beginning of therapy. Due to inhibition of the renin-angiotensin-aldosterone system, changes in renal function may occur in some patients. In patients with severe chronic heart failure, in whom renal function depends on the activity of the renin-angiotensin-aldosterone system, treatment with ACE inhibitors and angiotensin receptor antagonists may be accompanied by oliguria and/or increased azotemia and (rarely) acute renal failure and/or death. The combined use of Valz in patients suffering from chronic heart failure with ACE inhibitors and beta-blockers is not recommended due to a possible increased risk of side effects. In patients with bilateral or unilateral renal artery stenosis, regular monitoring of serum creatinine and urea nitrogen levels is necessary. Effect on the ability to drive vehicles and operate machinery During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Description of the drug VALSARTAN PLUS
Lithium preparations -
with simultaneous use of lithium preparations with ACE inhibitors and angiotensin II receptor blockers or thiazide diuretics, a reversible increase in the concentration of lithium in the blood plasma and an associated increase in toxic manifestations were noted. The risk of toxicities associated with the use of lithium may be further increased during concomitant use of this combination since the renal clearance of lithium is reduced by thiazide diuretics. Concomitant use of the combination of valsartan + hydrochlorothiazide is contraindicated.
Antihypertensive drugs -
it is possible to enhance the antihypertensive effect when used together with other drugs that lower blood pressure (ACE inhibitors, beta-blockers, slow calcium channel blockers, guanethidine, methyldopa, vasodilators, direct renin inhibitors, angiotensin II receptor blockers).
Pressor amines -
the effect of pressor amines (norepinephrine, epinephrine) may be weakened, without requiring cessation of joint use.
NSAIDs, including selective COX-2 inhibitors -
may weaken the antihypertensive effect of both angiotensin II receptor antagonists and hydrochlorothiazide when taken simultaneously. The simultaneous use of a combination of valsartan + hydrochlorothiazide and NSAIDs can lead to impaired renal function and an increase in potassium levels in the blood serum. If it is necessary to use this combination and NSAIDs together, renal function should be assessed and fluid and electrolyte disturbances corrected before starting treatment.
Potassium-containing substitutes for table salt; other medicines that increase serum potassium levels (for example, heparin)
requires compliance with precautions (including frequent determination of potassium levels in the blood).
Medicines that can cause hypokalemia -
The risk of hypokalemia caused by diuretics may be increased with simultaneous use of corticosteroids, laxatives, ACTH, amphotericin B, carbenoxolone, penicillin, acetylsalicylic acid or its derivatives and antiarrhythmic drugs.
Double blockade of the RAAS -
When treated with drugs that affect the RAAS, especially when they are combined, a marked decrease in blood pressure, syncope, stroke, hyperkalemia and impaired renal function (including acute renal failure) have been reported in sensitive patients. Concomitant use of the combination of valsartan + hydrochlorothiazide is contraindicated.
Caution is required when combining angiotensin II receptor blockers, including valsartan, with other drugs that block the RAAS, such as ACE inhibitors or aliskiren. Concomitant use of angiotensin II receptor blockers, including valsartan, or ACE inhibitors with aliskiren in patients with type 2 diabetes mellitus or impaired renal function (GFR < 60 ml/min/1.73 m2) is contraindicated.
Transport proteins -
According to the results of an in vitro study on hepatocyte cultures, valsartan is a substrate for the transporter proteins OATP1B1 and MRP2. Co-administration of valsartan with inhibitors of the OATP1B1 transport protein (rifampicin, cyclosporine) and with an inhibitor of the MRP2 transport protein (ritonavir) may increase the systemic exposure of valsartan (Cmax and AUC). Simultaneous use is contraindicated.
Curare-like muscle relaxants -
thiazide diuretics, including hydrochlorothiazide, potentiate the effect of non-depolarizing muscle relaxants. Simultaneous use is contraindicated.
Medicines that affect sodium levels in the blood -
The hyponatremic effect caused by diuretics may be enhanced when used simultaneously with antidepressants, antipsychotic anticonvulsants (carbamazepine). Caution should be exercised during long-term co-administration of hydrochlorothiazide with the above drugs.
Medicines that can provoke polymorphic ventricular
tachycardia of the "pirouette" type -
class IA antiarrhythmic drugs (quinidine, hydroquinidine, disopyramide); class III antiarrhythmic drugs (amiodarone, dofetilide, ibutilide), sotalol; some antipsychotics (thioridazine, chlorpromazine, levomepromazine, trifluoperazine, cyamemazine, sulpiride, sultopride, amisulpride, tiapride, pioside, haloperidol, droperidol); other drugs (bepridil, cisapride, difemanil, erythromycin IV, halofantrine, ketanserin, mizolastine, pentamidine, sparfloxacin, terfenadine, vincamine IV). Due to the risk of hypokalemia, hydrochlorothiazide should be used with caution concomitantly with drugs that can cause torsade de pointes (TdP).
Hypoglycemic agents -
Thiazide diuretics may alter glucose tolerance, which may require dose adjustments of insulin and oral hypoglycemic agents. Metformin should be used with caution due to the risk of developing lactic acidosis caused by possible renal impairment associated with hydrochlorothiazide.
Beta blockers and diazoxide -
simultaneous use of thiazide diuretics, incl. hydrochlorothiazide, with beta-blockers may increase the risk of developing hyperglycemia. Thiazide diuretics, incl. hydrochlorothiazide may enhance the hyperglycemic effect of diazoxide.
Anti-gout drugs (probenecid, sulfinpyrazone and allopurinol) -
Dosage adjustment of uricosuric agents (probenecid or sulfinpyrazone) may be required as hydrochlorothiazide may increase serum uric acid concentrations. Concomitant use of thiazide diuretics, including hydrochlorothiazide, may increase the incidence of hypersensitivity reactions to allopurinol.
Cardiac glycosides -
Hypokalemia and hypomagnesemia (undesirable effects of thiazide diuretics) may contribute to the development of cardiac arrhythmias in patients receiving cardiac glycosides.
N- and m-anticholinergics
(including atropine, biperiden) can increase the bioavailability of hydrochlorothiazide, which is associated with a decrease in gastrointestinal motility and the rate of gastric emptying. Accordingly, gastrointestinal motility stimulants (cisapride) may reduce the bioavailability of hydrochlorothiazide.
Cholestyramine and colestipol
may interfere with the absorption of concomitantly used drugs. The interval between doses should be 4-6 hours.
Vitamin D and calcium salts -
simultaneous use of hydrochlorothiazide with vitamin D or calcium supplements can lead to hypercalcemia due to increased calcium reabsorption.
Cyclosporine -
with simultaneous use of hydrochlorothiazide and cyclosporine, the risk of developing hyperuricemia and exacerbation of gout increases.
Methyldopa -
Cases of hemolytic anemia have been reported with the simultaneous administration of hydrochlorothiazide and methyldopa.
Co-administration of thiazide diuretics, including hydrochlorothiazide, may lead to an increased risk of side effects from amantadine
;
reducing the excretion by the kidneys of drugs that have a cytotoxic effect (for example, cyclophosphamide, methotrexate
), to potentiate their myelosuppressive effect.
Ethanol, barbiturates and narcotic drugs -
combined use with hydrochlorothiazide may potentiate the development of orthostatic hypotension.
When taking iodine contrast agents
in high doses against the background of a reduced volume of blood volume due to the use of diuretics, there is an increased risk of developing acute renal failure.