Hypotonia in newborns
Hypotonia, or decreased muscle tone, is usually found at birth or in infancy. If your baby has hypotension, he may be born lethargic, have difficulty sucking at the breast, and get tired quickly when feeding. When examined, such a child’s arms and legs easily extend at the joints; he can spread his hips almost without resistance to an angle of more than 90 degrees. A child with hypotonicity of the muscles of the cervical and shoulder girdle has difficulty controlling the head and has delays in the development of grasping skills and fine motor skills.
As a child with reduced muscle tone gets older, he or she will experience difficulty speaking, have incorrect posture, hypermobility in the joints, and decreased physical endurance.
What is muscle tone
Content:
- What is muscle tone
- How to recognize decreased muscle tone
- What Causes Muscle Hypotonia
- How is muscle hypotonicity diagnosed?
- Treatment of decreased muscle tone
- Reduced muscle tone in sedentary people
- Why you should monitor your muscle tone
Most people have a good understanding of what muscle strength is, but the term “muscle tone” can be difficult to explain. Strength is the ability of a muscle (or group of muscles) to work under load. This criterion can be objectively measured. But tone is a very subjective characteristic that determines the functionality of muscles at rest. But even when our body is at rest (that is, we do not move, and no individual muscle or group of muscles tenses), our muscles still do not go into absolute calm. There is such a thing as a baseline level of activity, which can be felt, but is difficult to measure. This condition is called muscle tone. It is muscle tone that allows a person to maintain one or another static posture, and is also responsible for supporting the bones of the skeleton (roughly speaking, without muscle support, the skeleton would simply crumble).
That is, healthy muscles never relax completely. They constantly maintain a certain tension and rigidity, which can be felt as resistance to movement. For example, the tone of the back and neck muscles allows a person to maintain his position when standing or sitting. In a healthy body, muscle tone decreases slightly when a person sleeps. Therefore, when someone falls asleep while sitting, their head usually falls to one side.
Muscle tone may be normal, low or high. Reduced tone is also called muscle hypotonia or muscle hypotonia. People with this disorder have difficulty holding their head up, standing and moving independently, and with any movement they can easily damage the skeleton. Increased tone in medicine is usually called muscle hypertonicity or spasticity. In this condition, the muscles constantly remain compressed, and the person constantly experiences spasms. People with this disorder find it difficult to assume a natural body position. Many of them cannot walk on the entire foot, but only on the toes, and they may also have impaired flexibility of the knee or hip joints.
Causes of hypotension in young children
Hypotension can be caused by congenital diseases of the nervous or muscular system. Sometimes hypotension is the result of birth or neonatal trauma, hypoxia during childbirth, an acquired disease, or an inherited disorder. Also, a decrease in muscle tone may be associated with physiological immaturity of the nervous system. There are situations when the cause of hypotension cannot be determined. Some babies are born with hypotension that is not associated with other diseases or conditions. This is called benign congenital hypotension. These children have minor developmental delays or learning difficulties. Physical and speech therapy can help a child regain tone and develop normally or reduce developmental delays.
It is important to know that hypotension can be caused by dangerous diseases that affect the brain, central nervous system or muscles:
Cerebral palsy
In many cases, these chronic diseases require lifelong care and treatment.
Hypotension can also be caused by genetic diseases:
- Down syndrome
- Prader-Willi syndrome
- Tay-Sachs disease
- Trisomy 13
- Hartnup's disease.
How to recognize decreased muscle tone
Decreased muscle tone is more common in infants and young children, although it sometimes occurs in adults.
If a baby suffers from muscle hypotonia, this will become noticeable by the 6th month of his life. Young children with decreased muscle tone are often characterized as being very flexible. But there are more clear signs of muscle hypotension in children. This:
- practically uncontrollable neck muscles, so these babies cannot hold their head up;
- when you hold such a child in your arms, you get the impression that he is about to slip out;
- the baby cannot hold anything in his hands;
- when the baby is picked up, his limbs simply hang to the sides, and do not bend at the elbows, hips or knees;
- the child has no sucking reflex and has difficulty swallowing;
- The voice and crying of such babies is very weak and quiet.
A child with muscle hypotonia, compared to healthy peers, needs much more time to learn to sit, crawl, walk, talk and eat.
The following symptoms may indicate hypotension in an adult:
- he looks clumsy and falls often;
- it is difficult for him to rise from a sitting or lying position;
- abnormally high degree of flexibility of the hip, elbow and knee joints;
- it is difficult for him to lift and carry heavy objects (manifests itself if decreased tone is accompanied by muscle weakness).
Muscle hypertonicity in a child
If your newborn baby constantly looks away, clenches his fists, has difficulty moving, and has obvious emotional signs of general discomfort, he may be suffering from hypertension.
Muscular hypertonicity is a condition in which a child's muscles are constantly tense, causing you to be unable to easily bend or straighten your child's legs and arms. If you touch the baby’s muscles, they will be dense to the touch, like those of a well-pumped bodybuilder. It is important to know that hypertonicity is a pathological condition.
In a newborn with hypertonicity, muscle tension can noticeably weaken only during sleep. As your baby grows, you may notice that he or she feels “stiff” and has trouble rotating his or her body or bending his or her limbs. In infants prone to hypertonicity, this condition may be caused by a startle reaction to an unexpected sound, movement or touch. Hypertonicity in fear is characterized by excessive arching of the head and jerky movements of the arms and legs. Sometimes severe fright can lead to a permanent state of hypertonicity.
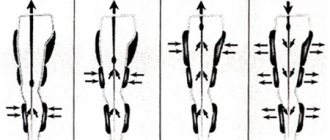
Children suffering from hypertension will have a delay in physical development due to the fact that tense muscles prevent him from moving normally. As a result, a baby with hypertonicity will learn to crawl and walk much later. If the problem of hypertonicity is not eliminated, the child’s gait will be very unstable, he will spread his legs wide when walking. Also, children with hypertonicity may suffer from congenital hip dislocation and sleep apnea due to impaired muscle function.
Treatment of decreased muscle tone
Is it possible to cure muscle hypotension? This is the first question that arises among adult patients, as well as among parents whose children have been diagnosed with “reduced muscle tone.” The answer to the question depends on the reasons that caused hypotension. In different clinical cases, the disease can develop according to different scenarios. Sometimes doctors manage to improve the patient’s condition, in some cases the clinical picture remains unchanged, and in many cases deterioration is possible over time.
The recommended treatment plan for decreased muscle tone is always determined by the doctor individually and depends on the underlying cause of the disease.
Premature babies born with reduced muscle tone, as a rule, become stronger as they grow older and are no different from their peers in adulthood. But at this time, the baby may need specialized care to eliminate other possible problems associated with prematurity.
If reduced muscle tone in a baby appears due to an infection or other illness, then after successful treatment of the underlying disease, muscular hypotension usually also goes away. There is also a chance to improve the child’s condition if his hypotension is a consequence of the presence of myasthenia gravis in the mother. But during the recovery period, again, you cannot do without qualified support from a doctor.
Unfortunately, it is impossible to cure decreased muscle tone if the disease is hereditary and is a congenital defect. In some cases, the patient’s condition can be slightly improved, but the tone cannot be completely returned to normal.
In any case, with reduced muscle tone, it is useful for a child or adult patient to undergo several courses of physical therapy. The physiotherapist will select exercises to improve the patient's posture and coordination (to help offset some of the low muscle tone), as well as a program to strengthen the muscles in the joints of the arms and legs (to provide support and better stability). Physical therapy can be very effective in treating decreased tone in children. But for this you need to do the exercises daily.
In addition to physical therapy, adult patients may also benefit from occupational therapy, during which patients are helped to develop the motor skills needed in everyday life (for example, dressing independently, eating).
If a patient with reduced muscle tone has problems with swallowing and the ability to speak, then he is prescribed language and speech therapy.
Causes of hypertension in children
Hypertonicity can be hereditary in nature and caused by mutations in a specific genetic sequence. Such mutations negatively affect the production of glycine in the child's body, which helps reduce the stimulating effect of neurons on muscle fibers in order to ensure their relaxation after tension. When something interferes with the functioning of glycine, the body's ability to control muscle relaxation is weakened.
To diagnose hypertonicity (for example, in order to distinguish hypertonicity from epilepsy), a neurologist may prescribe to a child:
- Electromyography (EMG), which will examine electrical impulses in the muscles.
- Electroencephalography (EEG) can be used to assess a child's brain activity and its effect on muscle tone.
- Molecular genetic testing can determine the presence of specific mutations in the GLRA1 and SLC6A5 genes.
Reduced muscle tone in sedentary people
Weak muscle tone can occur not only due to a serious disorder in the functioning of the body's systems, but also against the background of a sedentary lifestyle and lack of sufficient muscle training. This is what causes decreased tone in most healthy people. In other words, this condition can be characterized as muscle flabbiness. In this case, improving physical fitness (or better yet, preventing flab) is much easier than treating hypotension caused by neurological or other problems.
Obviously, the most effective way to improve muscle tone is through sports. But some types of training help restore muscles faster than others. In addition, such exercises are especially useful for those who want to increase muscle tone, but not increase their volume. Then it is useful to engage in the following sports:
- strength training using light weights but more repetitions of the exercise;
- exercises using fitness bands;
- yoga;
- Pilates.
However, the list of workouts useful for increasing muscle tone is not limited to those mentioned above. Any physical activity is good for muscles, even a regular walk (but it must be done regularly, at least 2 hours a day).
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Treatment of hypertension in children
To treat hypertension, your doctor may prescribe:
medications, physiotherapy, massage and osteopathy, aquatherapy. Consultation with a family psychologist is also important. Learning how to cope with emotions and disappointments and how to remain calm will be an important factor in creating a positive psychological climate in your child's environment.
- Massage and stretching exercises can significantly relax the muscles and provide relief to the child.
- Aquatherapy in warm water also promotes better muscle relaxation and overall calming of a child with hypertension. Aquatherapy sessions can be performed as early as 3 weeks of age.
- Thanks to the course of treatment, education of the child and parents, the child, as he grows up, will learn to cope with any restrictions and will be able to lead a full life.
Dystonia
Muscular dystonia is a disorder characterized by impaired motor activity of the child and abnormal development of muscle tone. Muscular dystonia can be caused by genetic disorders or birth trauma that leads to hypoxia of the child's brain or cerebral hemorrhage.
Other causes of acquired dystonia in infants may include:
- infections
- side effects of certain medications the mother took during pregnancy
- toxic effects on the fetus
The disorder is caused by impaired or immature connections between the nervous system and muscles. With dystonia against the background of general hypotension, when performing passive movements, individual muscles in the child become spastic (strongly contracted). In a child, this looks like a “combination” of hypertonicity of some muscles with hypotonicity of others, which leads to the appearance of writhing movements. This condition can appear after strong experiences, excitement, feelings of fear, in an unfamiliar environment, with sharp sounds or when touching a child with cold hands.
In addition to uncontrolled muscle movement, other symptoms of dystonia include leg cramps, involuntary neck movements, and uncontrolled blinking. Symptoms usually affect only one side of the body and stabilize within five years. However, accidents and injuries can worsen the disease.
The extreme severity of muscular dystonia is observed in children with cerebral palsy, which is a cause of disability.
There is no specific treatment for dystonia. Doctors use a complex of therapeutic measures, including drug and physical therapy, massages, osteopathy, and the help of a psychologist. Mild and moderate dystonia responds well to restorative treatment if it is started in a timely manner and carried out regularly.
The most important thing in the treatment of dystonia: the earliest possible diagnosis and initiation of therapy. The best results are observed if the diagnosis is made in the first months of life.
Very often, in babies under the age of one year, an attentive mother determines that the muscles in the arms and legs are too tense, or, conversely, the muscles are too relaxed. When examined by a neurologist, a violation of muscle tone is determined.
Many questions immediately arise: what is it, how is it determined, for what reason does it arise, why it is dangerous for the baby and how it can be corrected.
Muscle tone (Latin tonus from the Greek tonos - tension, tension), a state of slight physiological contraction of a muscle at rest, ensuring its readiness for work. (G. G. Shanko). In other words, tone is muscle tension, which is necessary to maintain body posture and ensure its movements.
Before birth in utero, the baby is in the fetal position, when the arms and legs are bent and pressed to the body. physiological hypertonicity remains during the first three months of life . By 3 months, the tone of the flexor and extensor muscles is leveled out and a state occurs that we characterize as normotonia. At the same time, the baby’s arms and legs unbend much more easily, and the fingers of the hands are rarely clenched into a fist.
Changes in muscle tone may appear as
- muscular hypertension or muscle hypertonicity,
- muscular dystonia,
- muscle hypotonia or muscle hypotonia.
Do you have questions for your pediatric neurologist? Call: +375 (29) 333-88-77 from 9.00 to 18.00 seven days a week
If the baby’s arms and legs are tightly pressed to the body, it is difficult to straighten them, the baby cries, throws his head back - this is due to excessive muscle tension. The number of impulses that comes from the central nervous system to the muscles is significantly increased.
Muscular hypertension syndrome is characterized by an increase in resistance to passive movements, limitation of spontaneous and voluntary motor activity, increased tendon reflexes, expansion of their zone, and foot clonus.
The severity of muscle hypertonia syndrome can vary from a slight increase in resistance to passive movements to complete stiffness. If muscle hypertonicity is not pronounced and is not combined with pathological tonic reflexes and other neurological disorders, its effect on the child’s development can manifest itself in a slight delay in motor skills. It also happens that motor development progresses according to age and the child begins to sit, stand up and walk in time, but at the same time the child’s feet rest on the toes, which leads to gait disturbance. Walking on your toes for a long time can lead to shortening of the Achilles tendons, which can only be corrected by surgical treatment.
Muscle hypotonia syndrome is characterized by a decrease in resistance to passive movements and an increase in their volume. Spontaneous and voluntary motor activity is limited. Tendon reflexes may be normal, increased, decreased, or absent, depending on the level of damage to the nervous system. Hypotension can transform into normotension, dystonia, hypertension, or remain a leading symptom throughout the first year of life.
The syndrome of movement disorders in children of the first year of life can manifest itself as muscular dystonia - a condition when muscle hypotension alternates with hypertension, that is, muscle tone is constantly changing. Muscular dystonia is also said to occur when some muscles in a child are too relaxed, while others, on the contrary, are too tense.
Severe muscular dystonia syndrome can lead to delayed motor development or movement disorders (for example, gait disturbance). Transient muscular dystonia syndrome does not have a significant effect on the age-related motor development of the child.
Disorders of muscle tone are often caused by problems in the functioning of the central nervous system - the brain or spinal cord, and are most often a consequence of hypoxia and ischemia. Hypoxia is a condition in which the baby’s body and central nervous system lack oxygen. Ischemia is a disruption of the blood supply to tissues, leading to hypoxia.
Impaired muscle tone occurs in serious severe diseases of the nervous system, such as various forms of myopathies, spinal muscular atrophy, myasthenia gravis, and can also be a consequence of inflammatory, vascular and traumatic diseases of the nervous system, always observed in cerebral palsy.
Detection of muscle tone disorders requires observation by a pediatric neurologist .
Observation by a pediatric neurologist at home Call: +375 (29) 333-88-77 from 9.00 to 18.00 seven days a week
If necessary, the specialist will prescribe additional research methods :
- Neurosonography
- Doppler examination of cerebral blood flow
- Consultation with an ophthalmologist.
Treatment of muscle tone disorders
- Therapeutic massage and gymnastics.
- Physiotherapeutic, including thermal and electrical procedures.
- Water procedures, relaxing or tonic baths, swimming.
- Fitball exercises.
- Drug treatment: drugs from the group of nootropics, vascular, sedatives, neurometabolic, vitamin drugs.
In most cases, in children with mild disturbances of muscle tone, it is possible to restore the functioning of the central nervous system and achieve normotonia.
Ivanova M.I. neurologist of the first category.
Preventative examinations of newborns by a neurologist
An experienced neurologist will be able to promptly diagnose a disease or developmental disorder of a child, prescribe additional diagnostic procedures: functional and ultrasound studies, conduct complex treatment, and involve the required specialists in the treatment process: physical therapy doctor, physiotherapist, psychologist, speech therapist, osteopath and others.
It is important to identify existing diseases in time, in the first months of life, in order to prevent delays in the child’s development or limitation of his capabilities.
The sooner treatment is prescribed, the more optimistic the prognosis will be. Timely, comprehensive therapy will save the child from age-related complications and many psychological problems, ensure his full development and create conditions for achievements in life.
Benefits of going to the clinic
Self-treatment of increased muscle tone may be ineffective or lead to complications, so you need to contact a clinic with a team of specialists. The doctor will prescribe examinations, conduct an examination and identify the exact cause of the pathology. Experts will also help determine whether the complaints are related to increased muscle tone or whether the problem of poor health lies elsewhere.
After the diagnosis is made, an individual treatment complex is selected that suits the specific patient. In case of physiological disorders and poor lifestyle, physiotherapeutic methods and regulation of periods of activity and rest are chosen for treatment. In case of internal or infectious disorders, drug therapy is added and a whole range of rehabilitation measures is developed.
A specialist can also provide advice on preventative measures if you notice that your lifestyle may be contributing to the development of muscle hypertonicity.
We suggest you order the Almag treatment device inexpensively.
Consultation with a neurologist is most effective at home
In order to examine the child and assess muscle tone, the child must be calm and should not cry at the time of examination or before the examination (crying can greatly affect tone). Children with altered tone react more sharply to changes in the environment, unfamiliar smells or sounds. Any fear or agitation of the baby can distort the results of the examination.
Therefore, in order for an examination by a neurologist to be as effective as possible, we recommend calling a neurologist to the newborn’s home.
Routine observation of newborns by a neurologist
Routine examinations by a neurologist are especially important for infants. During this period, the doctor can identify early manifestations of congenital diseases, such as hydrocephalus, cerebral palsy, malformations of the brain and spinal cord, and timely detect acquired diseases.
To prevent and timely identify possible disorders of the peripheral nervous system, brain and spinal cord, children in the first years of life need to be regularly examined by a pediatric neurologist.
A neurologist should examine a newborn baby:
- In the first 30 days after birth. If there are risk factors, several consecutive examinations are carried out during this period.
- Every 3 months during the first year of life.
- Every 6 months until the child reaches the age of three.
- Annual examinations up to 6 years of age.
- Preventive examinations during the period of adaptation to social life (7-11 years) and active puberty (11-14 years).
Diagnostic methods
Increased muscle tone in adults has the following symptoms: discomfort when performing habitual movements, which results in muscle stiffness during mobility. Muscle density increases, and there is a constant feeling of tension, tightness or stiffness of movement.
In a child, symptoms of hypertonicity are manifested by clenched fists, legs, and arms pressed to the chest. Also, in a baby, signs of impaired tone are the fetal position, which lasts longer than 2 weeks, the fact that the baby holds his head straight, and resistance is felt during gymnastics.
The following methods are used to make a diagnosis:
- Examination by a neurologist, therapist, endocrinologist, possibly a psychiatrist;
- Assessment of childbirth in the mother, as well as clarification of the characteristics of intrauterine development;
- General and biochemical blood test;
- Determining the absence of epilepsy and paralysis, as well as taking medications that can provoke an increase in muscle tone;
- EMG;
- CT or MRI;
- Ultrasound of the brain and neck;
- X-ray of the spine;
- Study of cerebrospinal fluid, levels of electrolytes and CPK in the blood.
It is mandatory to establish the root causes of the development of the pathological condition, after which an individual rehabilitation program is drawn up.
When you need to urgently call a neurologist at home
In newborns and children of the first year of life
- In a calm state, when crying or excited, the baby’s hands or chin begin to tremble.
- The baby's sleep is disturbed: there are difficulties falling asleep, shallow and restless sleep with frequent awakenings.
- When the fontanelle bulges.
- If the fontanel is painful, crying when touched)
- With frequent and profuse regurgitation, even with small amounts of food.
- When any convulsions occur.
- If the child has a forced position of the legs: with the toes tucked, or the feet are extended as if the child is “standing on tiptoes.”
- With monotonous crying, refusal to feed, sluggish sucking.
In children older than one year
- For severe or frequent headaches.
- For neck pain.
- If the child complains of shooting or piercing pain in the back when moving.
- For muscle twitching or tics.
- If your child experiences fainting.
- With constant absent-mindedness.
- With forgetfulness, sudden changes in mood.
- If the child experiences unmotivated crying or aggression.
- If speech, reading, or writing impairment is obvious.
- With a sharp decrease or impairment of vision, taste, hearing, and smell.
- With low learning ability, progressive educational retardation.
- With “bad behavior”, uncontrollability.
- With increased fatigue.
- If you see a lack or a sharp deterioration in contacts with other children.
- For bedwetting of urine or feces (for children over 5 years old, if it occurs more than 2 times a week).
- If a change in gait is obvious, refusal to stand on a leg.
- In case of sleep disturbance, if there is difficulty falling asleep.
In case of head injuries, loss of consciousness, severe convulsions, or the child’s condition is unclear, CALL AN AMBULANCE IMMEDIATELY.