Diabetes mellitus type 2.
It is a chronic disease of the endocrine system, which develops due to a lack of insulin and dysfunction of pancreatic cells. It manifests itself as excessive urination, increased thirst, itchy skin, increased appetite, fever, and muscle weakness. The diagnosis should be confirmed by laboratory tests, namely through a blood test for glucose concentration and the level of glycosylated hemoglobin. Treatment mainly uses a low-carbon diet, increased physical activity and hypoglycemic drugs.
Information about the disease.
In fact, “diabetes mellitus” from Greek means loss of sugar. Thus, the term reflects the main symptom of the disease (lack of sugar) - glucose is not retained in the body and is excreted in the urine. Type 2 diabetes mellitus (non-insulin-dependent) develops against the background of tissue insensitivity to the action of insulin, as well as a subsequent decrease in cell function. Diabetes mellitus type 2 (DM2) is different from diabetes mellitus type 1 (DM1). In diabetes 1, the lack of insulin is primary; in diabetes 2, the lack of the hormone is a consequence of a prolonged lack of insulin. Statistics are very diverse and depend on ethnic characteristics and living standards. In Russia, the prevalence is about 7%, and covers 90% of all forms of diabetes. The group most susceptible to the disease is people over 40-45 years of age.
FAQ
I was diagnosed with type 2 diabetes, but I don’t notice anything bad about my health. Is diabetes really that dangerous?
Type 2 diabetes mellitus most often begins like this - “not noticeably” and is detected only when the patient donates blood for a test for a completely different reason. This “silence” of the disease is very insidious. Before the patient learns of the diagnosis, there may already be chronic complications of the disease in the form of damage to the eyes, kidneys, and legs. These complications are very dangerous and difficult to treat. Plus, with diabetes mellitus, atherosclerosis begins to progress very quickly, which is fraught with stroke, heart attack, and ischemia of the lower extremities. Therefore, diabetes mellitus is a dangerous disease.
Is it possible to completely recover from diabetes?
Today, unfortunately, there is no such possibility. We diagnose diabetes mellitus once in a lifetime and keep it forever. You can ideally compensate for diabetes and then your blood sugar will not differ from people without diabetes, therefore, you will not risk developing complications of the disease. Usually doctors write this in the diagnosis: “Diabetes mellitus (type 1 or 2), compensated.
Should I follow a diet for diabetes if my blood sugar has returned to normal during treatment?
Diet therapy for diabetes mellitus cannot be canceled under any circumstances. Diet is the first component of treatment for this complex disease. Even if it seems to you that “one piece of cake” will not hurt, and even if you do not see high blood sugar on the glucometer after errors in nutrition, this is not a reason to cancel the diet. Failure to comply with dietary measures leads to gradually increasing sugar levels, which are then quite difficult to return to normal.
Is it possible to exercise if you have diabetes?
It’s not possible, but it’s absolutely necessary! Rational physical activity is useful not only for general well-being and maintaining muscle tone, but also playing sports reduces blood sugar, improves blood flow in the muscles, which means more oxygen enters the body's cells and ischemia does not occur, which so often accompanies diabetes.
What blood glucose levels should you aim for when treating diabetes?
For this disease, it is very desirable to have blood sugar in the range of normal values, which are determined for all people. These are fasting blood sugar figures of 3.3-5.5 mmol/l (in capillary blood) and 4.8-6.1 mmol/l (in venous plasma) and up to 7.8 mmol/l 2 hours after meals. Reducing blood sugar and keeping it within the physiological norm will reduce the risk of developing chronic complications of the disease to a minimum. There are situations when the endocrinologist advises not to reduce blood sugar to normal. This occurs in cases where the risk of a decrease in glycemia below normal is more dangerous than a moderate increase in blood sugar. Various neurological and psychiatric diseases, coronary heart disease, and old age usually require less strict control of diabetes. Of course, this should not mean that you can have a sugar level of 12-20 mmol/l. Everything should be reasonable.
If diabetes mellitus is a lifelong disease and goes “unnoticed”, without changing overall well-being, is it worth treating and monitoring it so strictly?
Of course, it is necessary to treat diabetes mellitus and this is very important. For the time being (this period can be quite long) there are no specific complications of the disease, even with persistent hyperglycemia, but then they can appear “all at once” and this will quickly affect the quality and life expectancy of a patient with diabetes.
What complications should you be wary of with diabetes?
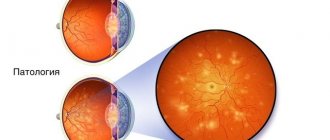
Diabetes mellitus has acute and chronic complications. As the name implies, acute complications develop quickly, “acutely”. The most common acute conditions in diabetes are hypoglycemia (a sharp decrease in blood sugar below normal) and diabetic ketoacidosis (a significant increase in blood sugar, against which acetone appears in the blood and urine). Both of these complications can lead to significant damage to body systems and death in a short period of time. Chronic complications are slow-onset damage to blood vessels and other tissues of the body against the background of chronic hyperglycemia. Eye damage – diabetic retinopathy can lead to complete blindness. Kidney damage leads the patient to a hemodialysis bed. Damage to nervous tissue leads to disruption of higher nervous activity and to the development of “neuropathic ulcers.” These slowly developing complications do not lead to immediate death, but they disable patients.
Now there are a lot of pills for the treatment of diabetes. How do you know which medications are best?
Only a doctor can understand which treatment will be best for each specific patient after examining the patient and conducting a clarifying examination. Eight classes of drugs exist to treat the disease, and more and more drugs are being developed. Pharmacotherapy of diabetes mellitus is perhaps the most “spoiled” branch of medicine. All drugs have their own indications and contraindications, and this is quite individual. The choice of drug is the doctor’s task.
If insulin is prescribed for diabetes mellitus, then “this is forever”? How to live “on injections”?
There are different types of diabetes, and accordingly there are different treatments. Insulin therapy is mandatory and vital for patients with type 1 diabetes. Without insulin, these patients quickly die. In type 2 diabetes, a temporary or permanent need for insulin treatment may also arise. With a sharp increase in blood sugar, with prolonged decompensation of diabetes mellitus, when the body's reserve capabilities are almost exhausted, insulin administration is required. After normalization of blood sugar, insulin (only for type 2 diabetes mellitus!) can be discontinued and return to tablet therapy. It should be remembered that type 2 diabetes mellitus may require constant administration of insulin. And this is not because there is a dependence on insulin (as patients who received insulin in a hospital often say), but because there is an insulin requirement, because your pancreas is no longer able to produce enough insulin.
My relatives have diabetes. What can I do to avoid getting sick?
Diabetes mellitus is a disease with a genetic predisposition and you can often see that one family suffers from this disease more often. The risk of getting sick certainly exists, but we can try to reduce this risk. If, unfortunately, we cannot change the genetic predisposition, then it is quite possible to exclude provoking factors for the development of the disease. A balanced diet and physical activity, reducing alcohol consumption, losing body weight (if it is in excess) are measures to prevent diabetes. Everyone knows this set of measures and it is called a “healthy lifestyle,” but in terms of preventing diabetes, there is nothing better.
Causes of type 2 diabetes mellitus.
The disease develops due to a combination of hereditary predisposition and external factors affecting the body throughout life. By adulthood, negative exogenous influences reduce the sensitivity of cells to insulin, as a result of which they cease to receive sufficient amounts of glucose. The main causes of type 2 diabetes:
- • Obesity. Fat tissue reduces the ability of cells to properly perceive insulin. Excess weight is one of the key risk factors for developing the disease. Obesity is present in 80-90% of patients;
- • Poor nutrition. The main cause of obesity is overeating. An increased calorie intake leads to the development of type 2 diabetes. In addition, excessive consumption of large amounts of sugar provokes surges in insulin secretion, which also provokes the development of the disease;
- • Physical inactivity. Lack of physical activity has a bad effect on the functioning of most organs of the body, and also helps to slow down metabolic processes. Physical inactivity is accompanied by low consumption of glucose by muscles, so it accumulates in the blood;
- • Endocrine diseases. Often, the disease occurs against the background of disruption of the endocrine system. Cases have been reported against the background of pancreatic tumors, pancreatitis, hypo- or hyperfunction of the thyroid gland;
- • Infectious diseases. In people with hereditary pathology, the initial appearance of diabetes mellitus can be triggered by an infectious disease - herpes, influenza and hepatitis.
Classification
Etiological classification of glycemic disorders (WHO, 1999)
Diabetes mellitus type 1 (caused by the destruction of beta cells, usually leading to absolute insulin deficiency): autoimmune, idiopathic.
Type 2 diabetes mellitus (may range from a predominance of insulin resistance with relative insulin deficiency to a predominance of defects in insulin secretion with or without insulin resistance).
Gestational diabetes mellitus.
Other specific types:
– genetic defects that cause dysfunction of beta cells;
– genetic defects that cause disruption of insulin action;
– diseases of the exocrine pancreas;
– endocrinopathy;
– induced by pharmacological and chemical agents;
– infections;
– rare forms of immune-mediated diabetes;
– other genetic syndromes sometimes associated with diabetes
Genetic defects in beta cell function:
| Genetic defects causing disruption of insulin action:
|
Diseases of the exocrine pancreas:
| Endocrinopathies:
|
Diabetes mellitus induced by pharmacological and chemical agents:
| Other genetic syndromes sometimes associated with diabetes:
|
Infections:
| Uncommon forms of immune-mediated diabetes
|
Mechanism of disease development.
The basis of the disease is a violation of carbohydrate metabolism due to increased cell resistance to insulin. The ability of tissues to accept and utilize glucose decreases, and a state of hyperglycemia (increased plasma sugar levels) develops. In addition, alternative ways of obtaining energy from amino acids and fatty acids are activated. To compensate for the glucose balance, the body begins to remove it through the kidneys (in the urine). A high concentration of sugar in body fluids causes an increase in osmotic pressure, causing copious and frequent urination. During this process, more fluid and salts are removed from the body, leading to dehydration and electrolyte imbalance. All this provokes the main symptoms of the disease - thirst, dry skin, weakness and arrhythmia.
Classification of the disease:
- • Lightweight. Treatment requires dietary adjustments, as well as a small dosage of a hypoglycemic drug. Low risk of complications;
- • Medium shape. To stabilize the disorders, constant intake of hypoglycemic agents is necessary. There is a possibility of initial stages of vascular complications;
- • Severe form. Patients require a course of tableted hypoglycemic drugs and insulin. Serious diabetic complications arise - angiopathy of small and large vessels, neuropathy, encephalopathy.
Symptoms of the disease.
Type 2 diabetes develops quite slowly. At the initial stage, the symptoms are practically invisible. The first symptom that appears is increased thirst. The mouth feels dry, and patients drink about 3-5 liters per day. With this volume, the amount of urine and frequency of urination increases. Due to the increased sugar content in the urine and frequent urination, itching and redness of the groin area occurs. Over time, itching occurs in the abdomen, armpits, knees and elbows. Since glucose does not reach the tissues in full, appetite increases (after 1-2 hours after eating, the patient feels hungry). Despite the high caloric content of the diet, the patient does not gain weight, since glucose is not absorbed, but is lost in urine.
Additional symptoms include increased fatigue, chronic feeling of tiredness, daytime sleepiness, weakness. The skin becomes drier, rashes and fungal formations appear. Bruises easily appear on the body, and wounds and abrasions take a very long time to heal. Women experience genital candidiasis, and men experience urethral infections. Some patients report tingling in their fingers and numbness in their feet. After eating, a feeling of nausea and even vomiting is also noticeable. Headaches and dizziness are common.
T2DM
Type 2 diabetes mellitus (T2DM) most often affects people over 40 years of age. This form of diabetes is characterized by relative insulin deficiency. For a long time, the disease may not manifest itself at all; symptoms appear gradually, so people often seek help late. Over time, the patient may need insulin therapy. Type 2 diabetes mellitus is treated mainly on an outpatient basis.
The risk of developing T2DM is higher in the following groups of people:
- age over 45 years;
- overweight (body mass index more than 25 kg/m²);
- high blood pressure (arterial hypertension, above 140/90 mm Hg);
- genetic predisposition (close relatives suffer from T2DM);
- low physical activity;
- elevated blood triglyceride levels (≥ 2.82 mmol/L) and decreased HDL cholesterol levels ≤0.9 mmol/L.
For people who are at risk, doctors recommend doing a blood test at least once a year and monitoring their glucose levels.
Symptoms of T2DM
Type 2 diabetes mellitus does not have specific symptoms that can clearly identify the disease, but the appearance of several symptoms of the disease at the same time may be a sign of the development of T2DM. Check if you have three or more symptoms from the list below, this is a reason to see a doctor:
- you feel dry in your mouth and constantly thirsty;
- you have excessive urination, including at night;
- your skin and mucous membranes are itchy;
- you quickly get tired and feel weak;
- your wounds and skin damage are healing slowly;
- pustules appear on the skin;
- you have lost a lot of weight and suddenly for no apparent reason.
What to do if you suspect you have T2DM?
If you feel unwell and experience symptoms of diabetes, the first thing you should do is consult a doctor. An examination performed by a therapist or general practitioner will help identify T2DM. To register at the clinic, you will need a passport and compulsory medical insurance policy. The doctor will decide on the need for further examination based on the results of the examination.
The following tests help identify T2DM:
- general blood analysis;
- general urine analysis;
- biochemical blood test with blood glucose testing;
- biochemical blood test to assess lipid metabolism disorders;
- determination of the level of glycated hemoglobin in the blood;
- oral glucose tolerance test.
All of the above tests can be done at the clinic at the site of attachment. The results will be ready 1-2 days after submission. The diagnosis may be as follows:
- diabetes mellitus has not been confirmed, but there are factors for its development;
- prediabetes was detected;
- type 2 diabetes mellitus was diagnosed.
Serious complications.
The development of type 2 diabetes mellitus may be accompanied by the development of chronic and acute complications. The most dangerous complications can lead to death - hyperglycemic coma, hypoglycemic coma, lactic acid coma. Chronic complications develop gradually and include diabetic microangiopathies and macroangiopathies - manifested by thrombosis and vascular atherosclerosis. Disturbances in the functioning of internal organs, joint pain and mental disorders (depression, emotional instability) are often noticeable.
How to diagnose type 2 diabetes?
The problem of identifying diabetes mellitus is manifested in the absence of obvious symptoms in the initial stages of the disease. Patients with a hereditary predisposition to the disease, or over 40 years of age with suspected diabetes, are recommended to undergo a blood plasma test for sugar levels. Laboratory tests will be the most informative and will detect not only the initial stage of diabetes mellitus, but also the state of prediabetes - decreased susceptibility to glucose. The examination is carried out by an endocrinologist.
To the Endocrinologist
Diagnosis begins with asking the patient about his well-being, symptoms of the disease are identified, and existing risk factors are analyzed. Once results from the laboratory are received, the diagnosis can be confirmed. There are several specific tests to detect type 2 diabetes:
- • Fasting glucose. The material is collected after 8-12 hours of fasting. Glucose levels above 7 mmol/l (venous blood) are a criterion for the disease;
- • Glucose test. To diagnose diabetes at an early stage, glucose concentrations are examined after eating a meal high in carbohydrates. With this test, a reading above 11.1 mmol/l is diabetes, a reading of 7.8-11.0 mmol/l is prediabetes;
- • Glycated hemoglobin. The analysis allows you to estimate the average glucose concentration in the body over the past 3 months. An indicator of 6.5% or more indicates diabetes, 6-6.4% indicates prediabetes.
Diff. diagnosis involves distinguishing between type 1 diabetes and type 2 diabetes. The clinical differences between these diseases are the slow increase in symptoms and the older age of the patients (although recently there have been cases of the disease in people aged 20-25 years).
Test results
Only a doctor can interpret test results, since he evaluates them in conjunction with other symptoms, weight, heredity, and condition. So in pregnant women, blood sugar levels may increase and the doctor decides whether adjustments are required or not. If a diagnosis of diabetes has been avoided, many may find themselves with prediabetes, impaired glucose tolerance and metabolic syndrome.
One of the clear ways to correct your diet and physical activity level is to use a Contour Plus glucometer with test strips included. A small drop of blood - an accurate measurement method will allow you to see the results of your efforts on the display and instill new healthy lifestyle habits. This can help avoid many problems in the future.
Prevention and treatment of type 2 diabetes
Endocrinology uses a systematic approach to therapy. In the initial stages of the disease, the greatest attention is paid to consultations and changes in the patient’s lifestyle (attempts to control sugar). If such treatment does not help, then a decision is made to use drug treatment. The complex of treatment procedures includes:
- • Diet. The main principle of the diet is to reduce foods high in carbohydrates and fats. The most dangerous are products with refined sugar (confectionery, candy, chocolate, lemonade). The diet should consist of vegetables, milk, meat, eggs and grains. The diet should be fractional (5-6 times a day), portions should be small;
- • Physical exercise. If the patient does not yet have severe complications, then sports activities are indicated for him. The duration and intensity of training is selected individually. Patients are usually recommended to exercise walking, swimming and walking;
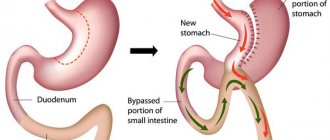
- • Drug treatment. Several groups of drugs are used. To reduce insulin resistance of cells, the absorption of glucose in the gastrointestinal tract and its production in the liver, the use of biguanides and thiazolidinediones is allowed. If the use of these drugs is not enough, drugs that enhance insulin activity are prescribed.
Timely diagnosis, an experienced endocrinologist and correctly prescribed treatment (including diet) are the key to successful treatment of the disease. Our multidisciplinary Sante Clinic employs experienced endocrinologists (PhD) who will help you maintain your health with diabetes mellitus type 1 and 2. Without queues, long waits “by appointment” and postponed appointments - we are waiting for you at Sante Clinic!
To the Endocrinologist
Recommendations
Even in the absence of an established diagnosis of diabetes, it is recommended to monitor blood sugar once a year - this is the simplest and most accessible method of early diagnosis of the disease. There is no specific prevention of diabetes, so it is recommended to maintain a healthy lifestyle: rational exercise and proper nutrition.
In the case when this diagnosis is confirmed, constant contact between the patient and the doctor is necessary. Only under this condition is it possible to prevent the destructive effects of diabetes on the body.