Pharmacological properties of the drug Simvastatin
A lipid-lowering agent synthesized from the fermentation product of Aspergillus terreus . After oral administration, simvastatin, which is an inactive lactone, undergoes hydrolysis into the corresponding β-hydroxyl form - the main metabolite and inhibitor of HMG-CoA reductase, an enzyme that is a catalyst in the early stages of cholesterol biosynthesis. Simvastatin reduces the content of total cholesterol in the blood plasma, as well as the level of LDL, VLDL and triglycerides; in addition, it slightly increases HDL levels, thus reducing the LDL/HDL ratio and total cholesterol/HDL. The active form of simvastatin is a specific inhibitor of HMG-CoA reductase, an enzyme that catalyzes the formation of mevalonic acid from HMG-CoA. Since the formation of mevalonate from HMG-CoA occurs at an early stage of cholesterol biosynthesis, treatment with simvastatin is not accompanied by the accumulation of potentially toxic sterols in the body. Moreover, HMG-CoA, in turn, is quickly converted into acetyl-CoA, a substance that is actively involved in many biosynthetic processes in the body. Simvastatin undergoes extensive primary extraction in the liver followed by excretion into the bile. The concentration of the active form of simvastatin in the systemic circulation is less than 5% of the orally administered dose; 95% of simvastatin is bound to plasma proteins. Simvastatin significantly reduces the concentration of total cholesterol and LDL in the case of heterozygous familial and non-familial hypercholesterolemia, as well as in mixed types of hyperlipidemia, when increased cholesterol levels are the main disorder. A positive therapeutic effect is observed after 2 weeks of treatment, reaching a maximum at 4–6 weeks, and persists with further administration of simvastatin. If you stop taking it, the concentration of total cholesterol in the blood returns to its original level. Slows down the progression of coronary atherosclerosis and reduces both the incidence of new lesions and the likelihood of developing total vascular occlusions.
Simvastatin in clinical practice: known facts, pleiotropic properties and new prospects
Cardiovascular diseases hold leading positions in the lists of causes of mortality and disability in most countries of the world. Thus, according to the World Health Organization, almost every third death worldwide occurs from diseases of the cardiovascular system, the foundation for which is created by atherosclerosis. A sharp reduction in the development of atherosclerosis is facilitated by special programs for its prevention and treatment developed in many countries around the world, an integral part of which is the use of lipid-lowering drugs.
The development and progression of atherosclerosis and its complications depend primarily on the level of cholesterol (C) in the blood serum, which led to a targeted search and development of drugs that affect the content and metabolism of lipids. Among different groups of medications that have a lipid-lowering effect, HMG-CoA reductase inhibitors (statins) turned out to be the most effective drugs that consistently reduce blood cholesterol levels. At the same time, there is a lot of evidence that the effect of statins is more than just a decrease in blood lipid levels. It has been shown that treatment with HMG-CoA reductase inhibitors is accompanied by an improvement in the clinical course of coronary heart disease (CHD), a reduction in recurrent myocardial infarction (MI), fatal and non-fatal, and a reduction in overall and coronary mortality (Cholesterol Treatment Trialists Collaborators, 2005).
A significant reduction in the incidence of MI during treatment with statins has been proven in a number of major randomized clinical trials: CARE (Cholesterol and Recurrent Events trial), 4S (Scandinavian Simvastatin Survival Study), PLAC-I (Pravastatin Limitation of Atherosclerosis in the Coronary Arteries), REGRESS (Regression Growth Evaluation Statin Study) and others. On this basis, drugs from the statin group were included in schemes for primary and secondary prevention of coronary artery disease. One of the safest and most studied statins is simvastatin (Zocor). In fact, it was the studies with simvastatin (HPS - Heart Protection Study, 4S) that were among the first to prove not only their lipid-lowering effect, but also their effect on endpoints. For example, the randomized, double-blind, placebo-controlled study 4S (Scandinavian Simvastatin Survival Study) examined the effect of long-term simvastatin therapy on the risk of coronary events in 4444 patients with coronary artery disease (previous myocardial infarction and/or angina) and moderate hypercholesterolemia (total cholesterol 5, 5–8 mmol/l) [1]. The 4S study was the most revealing regarding treatment and secondary prevention in patients with coronary artery disease when prescribed statins. In addition, it has been demonstrated that reducing total cholesterol and low-density lipoprotein (LDL) cholesterol can improve the prognosis of diabetic patients with coronary artery disease, more significantly than in patients without diabetes.
The randomized, placebo-controlled SCAT (Simvastatin/enalapril Coronary Atherosclerosis Trial) study examined the effects of long-term lipid-lowering therapy with simvastatin (10–40 mg/day, mean dose 28.5 ± 13 mg/day) on coronary atherosclerosis. According to angiography, in 460 patients with coronary artery disease with at least three visually confirmed atherosclerotic lesions of the coronary arteries, total cholesterol was 4.1–6.2 mmol/l, high-density lipoprotein cholesterol (HDL) was less than 2.2 mmol/ l, left ventricular ejection fraction (LV) - more than 35%. There was a significant decrease in LDL cholesterol levels by 30.5%. Repeated coronary angiography after 4 years showed a slowdown in angiographically confirmed coronary atherosclerotic narrowing in the simvastatin group by its effect on the mean diameter, minimum diameter and maximum percentage of diameter of stenoses, regardless of the main risk factors for coronary artery disease. Despite the fact that a significant reduction in mortality and the incidence of myocardial infarction in the simvastatin group was not detected during this study, nevertheless, a decrease in the need for coronary artery bypass grafting was noted [2].
Currently, HMG-CoA reductase inhibitors continue to be intensively studied. The growing interest in statins is explained by insufficient knowledge of their additional properties - the so-called pleiotropic effects.
Main pleiotropic effects of statins
- Effect on oxidized lipoproteins.
- Improvement of endothelial function.
- Decreased cell adhesion.
- Anti-inflammatory effect.
- Inhibition of proliferation and migration of smooth muscle cells.
- Stabilization of atherosclerotic plaque.
- Decreased platelet aggregation.
- Improvement of the fibrinolytic system.
- Effect on other organs and systems (prevention of osteoporosis, bone fractures; reduction of bile saturation with cholesterol, dissolution of cholesterol stones, antitumor effect, prevention of Alzheimer's disease and vascular dementia).
According to recent data, statins have a beneficial effect on the migration and functional state of macrophages, as well as on the migration and proliferation of smooth muscle cells in the vascular wall, thereby improving its biochemical and histochemical characteristics. In particular, by inactivating macrophages, statins reduce the production of metalloproteases and proinflammatory cytokines in them, which loosen the “cover” of the atherosclerotic plaque, destabilizing it. As a result, the risk of plaque rupture and intravascular thrombus formation is reduced. Inhibition of migration and proliferation of smooth muscle cells leads to a decrease in the potential volume of atheroma. The mechanism of anticoagulant action of statins is quite complex. These drugs reduce the level of plasma fibrinogen, normalize the lipid composition of blood cell membranes, inhibit ADP-dependent platelet aggregation, inhibit thromboxane production and reduce the concentration of tissue plasminogen activator-1 [3].
Taking into account the fact that to date a huge number of original articles and literature reviews have been published on the lipid-lowering properties of simvastatin (Zocor), as well as on its effect on morbidity and mortality from cardiovascular diseases, in this article we would like to focus the attention of readers on new data on the pleiotropic effects of simvastatin, as well as studies that in the future may expand the indications for its use.
Pleiotropic properties of simvastatin
Effect on oxidized lipoproteins. Oxidized lipoproteins appear to play a key role in the uptake of lipoprotein cholesterol by macrophages and in other processes, including the cytotoxic effect on endothelial cells. Statins reduce the sensitivity of lipoproteins to oxidation both in vitro and in vivo. Studies have shown that simvastatin therapy significantly reduces markers of oxidative stress in patients with hypercholesterolemia and diabetes mellitus [4].
Improvement of endothelial function. Endothelial dysfunction is a preclinical feature of early atherosclerosis. With endothelial dysfunction, diffusion of lipids and inflammatory cells (in particular, monocytes, T-lymphocytes) into the endothelium and subendothelial areas of blood vessels is observed [5]. Secretion of cytokines and growth factors stimulates migration into the intima, proliferation of smooth muscle cells and accumulation of matrix collagen, monocytes and other white blood cells, forming atheroma. Subsequent progression of atheroma, even non-occlusive one, can lead to a violation of its integrity, which leads to thrombosis, the development of acute coronary syndrome and MI [6]. Therefore, non-invasive determination of endothelial dysfunction is important for diagnosing and monitoring early atherosclerotic changes in the vascular endothelium. Statins have a corrective effect on endothelial dysfunction indirectly through the normalization of the blood lipid spectrum and through a direct effect on the endothelium (regardless of changes in the blood lipid spectrum) [7]. Wilson SH et al. experimentally established that simvastatin has a beneficial effect on endothelial function without hypolipidemic effects. This manifests itself in the form of a preserved response in increasing myocardial perfusion and the coherence of the microcirculatory response with increasing myocardial oxygen demand [8]. In a study by O'Driscoll G. et al. Treatment with simvastatin has been shown to improve endothelial dysfunction after 30 days [9].
Decreased cell adhesion. The interaction between blood leukocytes and vascular endothelium is an important component of the pathogenesis of atherosclerosis. Experiments have established an increase in the adhesion of leukocytes to endothelial cells when oxidized LDL is introduced into the blood, which is likely the result of the expression of adhesion molecules (ICAM-1, VCAM-1, P-selectin) on the surface of endothelial cells. During therapy with simvastatin, cell adhesion significantly decreased [10].
Anti-inflammatory effect. Epidemiological studies indicate a significant relationship between the inflammatory marker C-reactive protein (CRP) and the risk of cardiovascular events in patients with documented CAD. Thus, PM Ridker et al. proved that an elevated level of CRP increases the risk of cardiovascular events by 4 times, and the combination of elevated CRP and LDL increases the risk of cardiovascular events by 6 times. The identified relationship is explained by the fact that with an increased level of CRP, there is a significant acceleration of the passage of monocytes into and under the vascular endothelium, and consequently, a self-potentiating pathological circle of inflammation occurs in the vascular wall. Studies examining the effect of simvastatin on CRP levels in blood plasma revealed a dose-dependent effect. Thus, at a dose of 20 mg/day there was a moderate but significant decrease in CRP levels by 16%, while at a dose of 40 mg/day a decrease in CRP levels by 32% was observed in patients with hyperlipidemia. In patients with acute coronary syndrome with initially normal LDL cholesterol values, when comparing the anti-inflammatory effects of two dosages of simvastatin 10 and 40 mg/day, it turned out that only the maximum dose of the studied drug led to a significant decrease in CRP [5].
Inhibition of proliferation and migration of smooth muscle cells. It has been shown that the proliferation of smooth muscle cells requires isoprene derivatives formed during the metabolism of mevalonic acid [8]. Experimental work has revealed the inhibitory effect of simvastatin on the proliferation of smooth muscle cells and their migration. It was experimentally established that in rats simvastatin induces apoptosis of cardiomyocytes and smooth muscle cells; reduces the synthesis of interleukin-6 in vitro in a culture of human vascular smooth muscle cells [11]. Accordingly, long-term treatment with simvastatin improves the dilating function of vascular smooth muscle cells in hyperlipidemia and leads to a decrease in vascular wall stiffness in patients with arterial hypertension and hyperlipidemia.
Stabilization of atherosclerotic plaque. Atherosclerotic plaque rupture typically occurs in areas where macrophages accumulate and secrete metalloproteinases that weaken the thin fibrous cap. It was experimentally established that simvastatin reduces the in vitro secretion of metalloproteinase-9 by human and mouse macrophages due to its blocking effect on the metabolism of mevalonic acid [12]. Recent in vivo studies have demonstrated that in patients with coronary artery disease and hypercholesterolemia, simvastatin inhibits the expression of metalloproteinase-9 [13]. Thus, the ability of simvastatin to suppress macrophage activity suggests a stabilizing effect on atherosclerotic plaque independent of the lipid-lowering effect.
Long-term treatment with simvastatin in patients with hypercholesterolemia led to a significant reduction in the area of atherosclerotic lesions and intima-media thickness with an increase in the lumen of the vessel, according to magnetic resonance imaging [14].
Effect on platelet aggregation. Hypercholesterolemia is accompanied by an increase in platelet aggregation, which depends on the influence of factors such as lipid peroxidation, increased production of thromboxane, damage to the platelet membrane and the release of calcium into the cytoplasm. Treatment of patients with coronary artery disease and hypercholesterolemia with simvastatin resulted in a decrease in ADP-induced platelet aggregation, thromboxane B2 production, and calcium levels in the platelet cytoplasm [15].
In addition to inhibiting platelet aggregation, statins can reduce the production of tissue thromboplastin in the atherosclerotic plaque, reduce viscosity and increase fibrinolytic activity of the blood. It has been noted that simvastatin therapy leads to a decrease in the production of tissue thromboplastin in cultured human macrophages [16].
Influence on the mechanisms of fibrinolysis. Tissue plasminogen activator and plasminogen activator inhibitor-1 are predictors of subsequent cardiovascular events. Simvastatin reduces the expression of plasminogen activator inhibitor-1 and increases tissue plasminogen activator levels at sites of vascular injury, which reduces fibrin formation and prevents thrombus development [17]. In addition, simvastatin therapy led to a decrease in von Willebrand factor [18]. Fibrinogen is an independent and powerful predictor of vascular events. A number of studies have reported no significant changes in fibrinogen during treatment with simvastatin. Other clinical studies have demonstrated that simvastatin (10–20 mg/day) significantly reduced fibrinogen concentrations in patients with primary hypercholesterolemia, which is important in preventing the development of thrombotic complications. It was noted that in patients with coronary artery disease, even as a result of short-term therapy with simvastatin (20 mg) for four weeks, fibrinogen concentrations significantly decreased and the clinical course of angina improved [19]. Thus, the addition of statins to existing treatment improved survival in patients at high risk of vascular death. A special feature of the study was the identification of the beneficial effects of simvastatin not only in patients with coronary artery disease (a contingent of previous studies), but also with other vascular diseases, as well as in patients with diabetes mellitus. The large sample size of the study provided convincing evidence of the benefit of simvastatin in older adults and women. In addition, the benefits of simvastatin were observed regardless of concomitant therapy (Aspirin, beta-blockers, angiotensin-converting enzyme inhibitors).
Antitumor potential of simvastatin
Korean scientists obtained interesting data on two experimental mouse models: the first - with colitis-associated colon cancer and the second - a xenograft model of colon cancer. The effect of simvastatin on isolated tumor cells led to dose-dependent cell death, which increased with increasing exposure time to the drug. Simvastatin increased the activity of the caspase-3 enzyme and suppressed the expression of tumor markers Bcl-2, Bcl-xL, cIAP-1 and cFLIP. When analyzing the effect of the drug on tumor growth in mice, a significant slowdown in tumor growth was revealed in mice with colitis-associated colon cancer. In mice with a xenograft model of colon cancer treated with simvastatin, the tumor sizes were significantly smaller, the zones of tumor necrosis were larger, as well as the severity of signs of apoptosis. Thus, the authors believe that simvastatin has convincingly demonstrated its antitumor potential as both a preventive and therapeutic agent [20].
And already in 2009, in the journal Cancer chemotherapy and pharmacology Lee G. et al. published data from a phase II multicenter study in which simvastatin (40 mg/day every day) was included in anticancer treatment regimens along with irinotecan, fluorouracil, and calcium folinate (Leucovorin) in patients with metastatic colon cancer.
Simvastatin and mortality from sepsis
At the 29th International Congress of Internal Medicine, data from a small Paraguayan double-blind study were released, which included 65 patients with severe sepsis (54% men, mean age 53.5 years), 70% of whom were hospitalized in a state of septic shock [29th International Congress of Internal Medicine. Buenos Aires Sheraton Hotel & Convention Center Buenos Aires, Argentina September 16–20, 2008]. The patients were divided into two groups, comparable in severity of the condition and concomitant diseases, in which, in addition to the therapy, simvastatin was prescribed at a dose of 80 mg/day or placebo. Mortality in the simvastatin group was 50%, which was significantly lower than in the placebo group (80%; RR 0.54; p = 0.04). The authors attribute these differences in outcomes to the anti-inflammatory and antithrombotic properties of simvastatin.
This is how statins, using the example of one of the most well-studied and safe representatives of this class - simvastatin (Zocor), are conquering new “therapeutic niches” for their use in clinical practice, which, apparently, in the near future will change our attitude towards them as purely cardiological drugs, which we will primarily owe to the pleiotropic effects of statins.
D. A. Napalkov , Candidate of Medical Sciences A. V. Zhilenko MMA named after. I. M. Sechenova , Moscow
Literature
- Scandinavian Simvastatin Survival Study Group: Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) // Lancet. 1994; 344(8934):1383–1389.
- Burton JR, Teo KK, Buller CE et al. Effects of long term cholesterol lowering on coronary atherosclerosis in patient risk factor subgroups: the Simvastatin/enalapril Coronary Atherosclerosis Trial (SCAT) // Can J Cardiol. 2003; 19: 487–491.
- Libby P., Aikawa M. Mechanism of plaque stabilization with statins // Am J Card. 2003; 20:4A–8B.
- Marcetou ME, Zacharis EA, Nokitovich D. et al. Early effects of simvastatin versus atorvastatin on oxidative stress and proinflammatory cytokines in hyperlipidemic subjects // Angiology. 2006; 57: 211–218.
- Susekov A.V. HMG-CoA reductase inhibitors in the secondary prevention of atherosclerosis: 30 years later // Consilium medicum. 2005; No. 11, p. 896–903.
- Gratsiansky N.A. Atorvastatin: test results with low initial low-density lipoprotein cholesterol // Consilium_medicum. 2005; No. 11, p. 903–912.
- Simons L. A, Sullivan D., Simons J. et al. Effects of atorvastatin, monotherapy and simvastatin plus cholestyramine on arterial endothelial function in patients with severe primary hypercholesterolaemia // Atherosclerosis. 1998; 137:197–203.
- Aronov D. M. Simvastatin. New data and perspectives. M.: Triad X, 2002, 80 p.
- O'Droscoll G., Green D., Tylor R. Simvastatin an HMG-CoA reductase inhibitors, improves endothelial function within 1 month // Circulation. 1997; 95:1126–1131.
- Sardo MA, Castaldo M, Cinquegrani M et al. Effects of simvastatin treatment on sI_CAM_1 and sE_selectin levels in hypercholesterolemic subjects // Atherosclerosis. 2001; 155: 143–147.
- Shevchenko O. P., Shevchenko A. O. Statins are HMG-CoA reductase inhibitors. M.: Reafarm, 2003, 112 p.
- Eberlein M., Heusinger-Ribeiro J., Goppelt-Struebe M. Rho-dependent inhibition of the induction of connective tissue growth factor (CTGF) by HMG CoA reductase inhibitors (statins) // Br. J. Pharmacol. 2001. Vol. 133. P. 1172–1180.
- Briel M, Schwartz GG, Thompson PL et al. Effects of early treatment with statins on short-term clinical outcomes in acute coronary syndromes: a meta-analysis of randomized controlled trials // JAMA. 2006; 295:2046–2056.
- Grines CL The role of statins in reversing atherosclerosis: what the latest regression studies show // J Interv Cardiol. 2006; 19:3–9.
- Nomura S., Shouzu A., Omoto S. et al. Losartan and simvastatin inhibit platelet activation in hypertensive patients // J Thromb Thrombolysis. 2004; 18: 177–185.
- Kunieda Y., Nakagawa K., Nishimura H. et al. HMG CoA reductase inhibitor suppresses the expression of tissue factor and plasminogen activator inhibitor-1 induced by angiotensin II in cultured rat aortic endothelial cells // Thromb Res. 2003; 110:227–234.
- Krysiak R., Okopie B., Herman Z. Effects of HMG-CoA reductase inhibitors on coagulation and fibrinolysis processes // Drugs. 2003; 63:1821–1854.
- Bickel C., Rupprecht H. J., Blankenberg S. et al. Relation of markers of inflammation (C-reactive protein, fibrinogen, von Willebrand factor, and leukocyte count) and statin therapy to long-term mortality in patients with angiographically proven coronary artery disease // Am J Cardiol. 2002; 89:901–908.
- Broncel M., Marczyk I., Chojnowska-Jezierska J. et al. The comparison of simvastatin and atorvastatin effects on hemostatic parameters in patients with hyperlipidemia type II // Pol Merkuriusz Lek. 2005; 18: 380–384.
- Cho SJ, Kim JS, Kim JM et al. Simvastatin induces apoptosis in human colon cancer cells and in tumor xenografts and attenuates colitis-associated colon cancer in mice // Int J Cancer. 2008; 123(4):951–957.
Indications for use of the drug Simvastatin
For coronary artery disease, it is prescribed to reduce mortality, reduce the risk of coronary death and non-fatal myocardial infarction, and the risk of undergoing myocardial revascularization procedures (coronary artery bypass grafting and percutaneous transluminal coronary angioplasty); slowing the progression of coronary atherosclerosis, including preventing the development of total vascular occlusions and the occurrence of new lesions. For hyperlipidemia, it is prescribed to reduce elevated levels of total cholesterol, LDL cholesterol, apolipoprotein B and triglycerides in patients with primary hypercholesterolemia, heterozygous familial hypercholesterolemia or combined (mixed) hyperlipidemia in cases where diet and other non-drug methods are ineffective. Indicated in combination with diet and other non-drug methods to reduce elevated levels of cholesterol and apolipoprotein B in patients with homozygous familial hypercholesterolemia and hypertriglyceridemia in cases where these methods are ineffective.
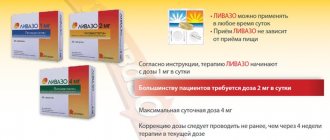
Use of the drug Simvastatin
Before starting to take simvastatin, the patient should be prescribed a standard cholesterol-lowering diet, which must be followed during drug treatment. For hyperlipidemia, the initial dose is usually 10 mg/day taken once in the evening. In patients with mild to moderate hypercholesterolemia, the initial dose may be reduced to 5 mg. If necessary, dose selection should be carried out at intervals of at least 4 weeks up to 40 mg/day in 1 dose in the evening. If the LDL level decreases below 75 mg/dL (1.94 mmol/L) or total plasma cholesterol below 140 mg/dL (3.6 mmol/L), the dose of simvastatin should be reduced. The dose of simvastatin for patients with homozygous familial hypercholesterolemia is 40 mg/day in the evening or 80 mg/day, divided into 3 doses (20, 20 and 40 mg at night). Simvastatin should be used as an adjunct to other lipid-lowering treatments (eg, LDL apheresis) in these patients if these treatments are not available. For ischemic heart disease, the initial dose is 20 mg/day in 1 dose in the evening. If dose adjustment is necessary, it should be selected as described above. Simvastatin is effective both as monotherapy and in combination with bile acid sequestrants. When patients are simultaneously taking cyclosporine, fibrates or nicotinic acid, the maximum dose of simvastatin should not exceed 10 mg/day. Since simvastatin is practically not excreted in the urine, there is no need to reduce the dose in patients with moderate chronic renal failure. In persons with severe renal impairment (creatinine clearance less than 30 ml/min), doses above 10 mg/day should be used with great caution.
Simvastatin Zentiva, 20 mg, film-coated tablets, 28 pcs.
Before and during treatment, the patient must follow a cholesterol-lowering diet.
At the beginning of therapy with Simvastatin Zentiva, a transient increase in the activity of liver enzymes is possible.
Before starting therapy and thereafter, liver function tests should be performed regularly (monitor liver transaminase activity every 6 weeks for the first 3 months, then every 8 weeks for the remainder of the first year, and then every six months), and should also be performed when increasing doses. liver function test. When increasing the dose to 80 mg, a test must be performed every 3 months. Simvastatin Zentiva, like other HMG-CoA reductase inhibitors, should not be used if there is an increased risk of rhabdomyolysis and renal failure (against the background of severe acute infection, arterial hypotension, trauma, severe metabolic disorders, before major surgery).
In patients with low thyroid function (hypothyroidism) or certain kidney diseases (nephrotic syndrome), when the concentration of cholesterol in the blood increases, the underlying disease should be treated first.
Simvastatin Zentiva should be administered with caution to patients who abuse alcohol and/or have a history of liver disease.
Drinking grapefruit juice (more than 1 l/day) may increase the severity of side effects associated with the use of Simvastatin Zentiva, so their simultaneous use should be avoided.
Simvastatin Zentiva is not indicated in cases where there is hypertriglyceridemia of types I, IV and V.
Treatment with Simvastatin Zentiva may cause myopathy leading to rhabdomyolysis and renal failure.
Predisposing factors for the development of myopathy include old age (over 65 years), female gender, uncontrolled hypothyroidism and impaired renal function. The risk of this pathology increases when using one or more of the following drugs with Simvastatin Zentiva: fibrates (gemfibrozil), cyclosporine, nefazodone, macrolides (erythromycin, clarithromycin, telithromycin), azole antifungals (ketoconazole, voriconazole, itraconazole, posaconazole ) and HIV protease inhibitors (ritonavir, nelfinavir), slow calcium channel blockers (verapamil, diltiazem, amlodipine), amiodarone, dronedarone, fusidic acid. The risk of developing myopathy also increases in patients with severe renal failure (creatinine clearance <30 ml/min).
All patients starting therapy with Simvastatin Zentiva, as well as patients who need to increase the dose of the drug, should be informed of the possibility of myopathy and the need to immediately seek medical attention if unexplained pain, muscle soreness, lethargy or muscle weakness occurs, especially if accompanied by malaise or fever. Drug therapy should be discontinued immediately if myopathy is diagnosed or suspected.
In order to diagnose the development of myopathy, it is recommended to regularly measure CPK activity.
When treated with Simvastatin Zentiva, an increase in serum CPK activity is possible, which should be taken into account in the differential diagnosis of chest pain. The criterion for discontinuation of the drug is an increase in CPK activity in the blood serum by more than 10 times relative to the ULN. In patients with myalgia, myasthenia gravis and/or a marked increase in CPK activity, treatment with the drug is discontinued.
Data from current studies do not contain information regarding the adverse effects of simvastatin on the lens of the eye.
The drug is effective both as monotherapy and in combination with bile acid sequestrants.
For patients with severe renal failure, treatment is carried out under the monitoring of renal function.
The duration of use of the drug is determined individually by the attending physician.
Drugs of the statin class can cause an increase in blood glucose concentrations. In some patients at high risk of developing diabetes mellitus, such changes may lead to its manifestation, which is an indication for antidiabetic therapy. However, the reduction in the risk of vascular diseases while taking statins exceeds the risk of developing diabetes, so this factor should not serve as a basis for discontinuing statin treatment. Patients at risk (fasting blood glucose concentration 5.6-6.9 mmol/l, BMI >30 kg/m2, hypertriglyceridemia, history of arterial hypertension) should be under medical supervision and regularly monitor biochemical parameters.
Side effects of the drug Simvastatin
abdominal pain, constipation, flatulence, nausea, vomiting, diarrhea, pancreatitis, hepatitis, asthenia, headache, myopathy, dizziness, convulsions, myalgia, rhabdomyolysis, paresthesia, peripheral neuropathy, skin rash, itching, alopecia, anemia, hypersensitivity syndrome to simvastatin (angioedema, lupus-like syndrome, rheumatoid polymyalgia, vasculitis, thrombocytopenia, eosinophilia, increased ESR, arthritis, arthralgia, urticaria, photosensitivity, fever, flushing, shortness of breath and malaise), increased activity of alkaline phosphatase transaminases and γ-glutamyltransferase in blood plasma.
Special instructions for the use of the drug Simvastatin
Simvastatin and other HMG-CoA reductase inhibitors sometimes cause myopathy, which is manifested by myalgia or muscle weakness associated with a significant increase in creatine kinase levels. Rhabdomyolysis is rare. Simvastatin therapy should be discontinued if myopathy is diagnosed or suspected. Before prescribing simvastatin and periodically during treatment, for 1 year or up to a year after the last dose increase, liver function should be monitored in all patients. Patients whose dose was increased to 80 mg should be re-examined after 3 months. Particular attention should be paid to patients with elevated levels of transaminases in the blood plasma. They need to immediately re-test these indicators, and repeat the tests more often during treatment. If there is a tendency to increase the level of plasma transaminases, especially if it consistently exceeds the upper limit of normal by more than 3 times, treatment should be stopped. Prescribe with caution to persons who abuse alcohol, as well as with a history of liver disease. Liver disease in the acute period or an unexplained increase in plasma transaminases are contraindications to treatment with simvastatin. The safety and effectiveness of simvastatin in children has not been established.
SIMVASTATIN
special instructions
Myopathy/Rhabdomyolysis
Simvastatin, like other GM-CoA reductase inhibitors, can cause myopathy, which manifests itself as muscle pain, soreness or weakness and is accompanied by an increase in CPK activity (more than 10 times the upper limit of normal (ULN)). Myopathy may manifest itself in the form of rhabdomyolysis, sometimes accompanied by secondary acute renal failure due to myoglobinuria. In rare cases, death has occurred. The risk of developing myopathy increases due to an increase in the concentration in the blood plasma of substances that have an inhibitory effect on HMG-CoA reductase. Risk factors for developing myopathy include older age (>65 years), female gender, uncontrolled hypothyroidism, and impaired renal function.
As with treatment with other HMG-CoA reductase inhibitors, the risk of developing myopathy/rhabdomyolysis depends on the dose. In clinical studies (median follow-up of 4 years), the incidence of myopathy at doses of 20, 40 and 80 mg per day was 0.03%, 0.08% and 0.61%, respectively. In these studies, patients were closely monitored, and a number of drugs that may interact with simvastatin were not used.
In a clinical study in which patients with a history of myocardial infarction took simvastatin at a dose of 80 mg per day (mean follow-up 6.7 years), the incidence of myopathy was approximately 1.0%, and in patients taking the drug at a dose of 20 mg per day day - 0.02%. Approximately half of the cases of myopathy were reported during the first year of treatment. The incidence of myopathy during each subsequent year of treatment was approximately 0.1%.
In patients taking simvastatin at a dose of 80 mg per day, the risk of developing myopathy is higher than when using other statins that cause a comparable decrease in LDL cholesterol concentrations. Therefore, simvastatin at a dose of 80 mg per day should be prescribed only
patients with a high risk of cardiovascular complications, in whom drug therapy at lower doses did not achieve a therapeutic effect, and the expected benefit of treatment outweighs the possible risk. If a patient taking simvastatin 80 mg requires treatment with another drug that may interact with simvastatin, the dose of simvastatin should be reduced or another statin that has less potential for drug interaction should be prescribed (see sections Contraindications and Dosage and Administration ).
All patients who begin therapy with Simvastatin, as well as patients who need to increase their dose, should be warned about the possibility of myopathy and informed about the need to immediately contact a doctor if any unexplained pain, muscle soreness or muscle weakness occurs. Therapy with Simvastatin should be discontinued immediately if myopathy is diagnosed or even suspected.
The presence of the above symptoms and/or a more than 10-fold increase in CPK activity compared to ULN indicates the presence of myopathy. In most cases, after immediate cessation of simvastatin, the symptoms of myopathy resolve and CPK activity decreases. In patients starting to take simvastatin or increasing the dose of the drug, periodic determination of CPK activity is advisable, but there is no guarantee that such monitoring can prevent the development of myopathy.
Many of the patients who experienced rhabdomyolysis during simvastatin therapy had a complicated medical history, including impaired renal function, usually due to diabetes mellitus. Such patients require more careful monitoring.
Simvastatin therapy should be temporarily discontinued in patients several days before major surgery and during the postoperative period.
The risk of developing myopathy/rhabdomyolysis increases when simvastatin is used simultaneously with the following drugs:
Contraindicated drugs
- Potent
CYP3A4 inhibitors:
Concomitant therapy with potent CYP3A4 inhibitors at therapeutic doses (eg,
itraconazole, ketoconazole, posaconazole, erythromycin, clarithromycin, HIV protease inhibitors, boceprevir, telaprevir, or nefazodone)
is contraindicated. If treatment with itraconazole, ketoconazole, posaconazole, erythromycin, clarithromycin or telithromycin cannot be avoided, simvastatin therapy should be interrupted for the duration of their use (see section “Contraindications” and “Interaction with other drugs”). - Gemfibrozil, cyclosporine or danazol:
simultaneous use of these drugs with simvastatin is contraindicated (see section “Contraindications and interactions with other drugs”).
Other drugs
- Other fibrates: in patients taking fibrates other than gemfibrozil
(see section "Contraindications")
or fenofibrate, the dose of simvastatin should not exceed 10 mg per day.
With the simultaneous use of simvastatin and fenofibrate, the risk of developing myopathy does not exceed the sum of the risks when treating each drug separately. Fenofibrate should be used with caution in combination with simvastatin, as both drugs can cause myopathy. The addition of fibrates to simvastitin usually leads to a small additional decrease in the concentration of LDL cholesterol, but allows for a more pronounced decrease in the concentration of TG and an increase in the concentration of HDL cholesterol. In small, short clinical studies in which both drugs were used under close supervision, combination therapy with fibrates and simvastatin was not associated with the development of myopathy (see section "Interactions with other drugs").
Amiodarone: In patients taking amiodarone, the dose of simvastatin should not exceed 20 mg per day.
(see section “Interaction with other drugs”).
Blockers of "slow" calcium channels
- Verapamil or diltiazem: In patients taking verapamil or diltiazem, the dose of simvastatin should not exceed 20 mg per day.
(see section “Interaction with other drugs”).
- Amlodipine: In patients taking amlodipine, the dose of simvastatin should not exceed 40 mg per day
(see section “Interaction with other drugs”).
Moderate inhibitors of the
CYP3A4 isoenzyme:
with simultaneous use of drugs with moderate inhibitory activity against the CYP3A4 isoenzyme and simvastatin, especially at higher doses, the risk of developing myopathy may increase.
Fusidic acid:
in patients taking fusidic acid and simvastatin simultaneously, the risk of developing myopathy may increase (see section "Interaction with other drugs"). Patients should be closely monitored when fusidic acid is used concomitantly with simvastatin. A break in treatment with simvastatin is possible.
Nicotinic acid (> 1 g/day):
with simultaneous use of simvastatin and nicotinic acid in lipid-lowering doses (> 1 g/day), cases of myopathy/rhabdomyolysis have been described. In an ongoing double-blind, randomized clinical trial conducted in China, the UK and Scandinavia, an interim safety analysis by an independent committee showed that the incidence of myopathy in approximately 4700 patients (UK/Scandinavia) treated with simvastatin 40 mg or ezetimibe /simvastatin 10/40 mg in combination with laropiprant/ nicotinic acid sustained release at a dose of 40 mg/2 g, was comparable to the overall incidence of myopathy in all clinical studies of simvastatin 40 mg (0.08%). However, in approximately 3900 Chinese patients in the same group, the incidence of myopathy was higher than expected (approximately 0.9%). In the control group (placebo + simvastatin 40 mg or ezetimibe/simvastatin 10/40 mg), the risk of developing myopathy in 8600 patients of Chinese, British and Scandinavian nationalities was not increased. Given the higher incidence of myopathy in patients of Chinese nationality, caution should be exercised when taking simvastatin (especially in doses > 40 mg) in combination with nicotinic acid or drugs containing nicotinic acid in lipid-lowering doses (> 1 g/day) in representatives of this group. nationality. Since the risk of developing myopathy depends on the dose, it is not recommended for Chinese patients to prescribe simvastatin at a dose of 80 mg in combination with nicotinic acid or drugs containing nicotinic acid in lipid-lowering doses (> 1 g / day). There is no data on an increase in the risk of developing myopathy during concomitant treatment in other representatives of the Mongoloid race (see section “Interaction with other drugs”).
Effect on the liver
Some adult patients taking simvastatin experienced sustained elevations in liver enzyme activity (more than 3 times the ULN). When the drug was discontinued or interrupted, the activity of liver transaminases usually gradually returned to the original level. Increased activity of liver transaminases was not associated with jaundice or other clinical symptoms. No hypersensitivity reactions were identified. Some of the above patients had abnormal liver function tests before starting treatment with simvastatin and/or abused alcohol.
Before starting treatment, and then in accordance with clinical indications, liver function tests are recommended in all patients. For patients in whom the dose of simvastatin is planned to be increased to 80 mg per day, additional liver function tests should be performed before moving to the indicated dosage, then after 3 months after starting its use, and then regularly repeat (for example, once every six months) for first year of treatment. Particular attention should be paid to patients with increased activity of serum transaminases. These patients need to repeat the study in the near future and subsequently carry it out regularly until the activity of serum transaminases normalizes. In cases where the activity of “liver” transaminases increases, especially when the ULN is persistently exceeded by 3 times, the drug should be discontinued. The cause of increased alanine aminotransferase (ALT) activity may be muscle damage, so increased ALT and CPK activity may indicate the development of myopathy (see section “Special instructions, Myopathy/Rhabdomyolysis”).
There have been rare post-marketing reports of fatal and non-fatal cases of liver failure in patients taking statins, including simvastatin. If serious liver damage with clinical symptoms and/or hyperbilirubinemia or jaundice develops during treatment with simvastatin, therapy should be interrupted immediately. If no other cause for the development of this pathology has been identified, re-prescribing simvastatin is contraindicated.
In patients who abuse alcohol and/or patients with impaired liver function, the drug should be used with extreme caution. Active liver disease or unexplained elevations in aminotransferase activity are contraindications to simvastatin.
During treatment with simvastatin, as with treatment with other lipid-lowering drugs, a moderate (less than 3 times the ULN) increase in the activity of serum transaminases was observed. These changes appeared soon after the start of treatment, were often transient, were not accompanied by any symptoms and did not require interruption of treatment.
Ophthalmological examination
Data from modern long-term clinical studies do not contain information regarding the adverse effects of simvastatin on the human lens.
Use in children and adolescents aged 10-17 years
The safety and effectiveness of simvastatin in children and adolescents aged 10-17 years with heterozygous familial hypercholesterolemia were assessed in controlled clinical studies involving boys 10-17 years old and girls 10-17 years old at least 1 year after menarche. Pediatric patients treated with simvastatin had a similar side effect profile to patients treated with placebo. The use of simvastatin at a dose of > 40 mg per day has not been studied in pediatric and adolescent patients.
In this study, there was no significant effect of simvastatin on the growth and puberty of boys and girls, or any effect on the length of the menstrual cycle in girls. Girls should be advised about appropriate methods of contraception during treatment with simvastatin (see section “Contraindications”, “Use during pregnancy and breastfeeding”). The use of simvastatin has not been studied in children under 10 years of age or in girls 10–17 years of age before menarche.
Use in elderly patients
In patients over the age of 65 years, the effectiveness of simvastatin, assessed by the level of reduction in the concentration of total cholesterol and LDL cholesterol, is the same as in the population as a whole; no significant increase in the frequency of clinical or laboratory side effects was observed. However, in a clinical study of simvastatin 80 mg daily, patients over 65 years of age had an increased risk of developing myopathy compared with patients under 65 years of age.
Drug interactions Simvastatin
The risk of developing myopathy increases with concomitant treatment with drugs that cause the development of myopathy when administered alone (gemfibrozil and other fibrates), as well as nicotinic acid in hypolipidemic doses (more than 1 g/day). Simvastatin and other HMG-CoA reductase inhibitors are metabolized by the cytochrome P450 isoform 3A4, so drugs that, at therapeutic doses, have an inhibitory effect on this metabolic pathway may significantly increase plasma levels of HMG-CoA reductase inhibitors and thus increase the risk of developing myopathy. These include cyclosporine, mibefradil (a calcium antagonist of the tetralol class), itraconazole, ketoconazole and other azole antifungals, macrolide antibiotics (erythromycin, clarithromycin), and the antidepressant nefazodone. Simvastatin may enhance the effect of coumarin anticoagulants.