All articles
Using suppositories for pain relief and treatment of hemorrhoids
26.09.2017
Suppositories for hemorrhoids are an effective treatment for the disease. The combination of various active ingredients allows you to eliminate the symptoms of the disease.
Today there are many effective ways to treat hemorrhoids. Symptoms can often be relieved with over-the-counter medications and lifestyle changes. One of the most popular remedies are suppositories, or rectal suppositories “for hemorrhoids”. Such candles have different effects and are used for specific purposes. Doctors do not recommend using several remedies to treat hemorrhoids at the same time. Also, you should not use medications containing glucocorticosteroids uncontrollably for longer than 5–7 days. Be sure to tell your doctor if your symptoms worsen while using them, such as increased itching.
Advantages and disadvantages of candles
Rectal suppositories are intended for insertion into the rectum. They contain an active substance and various auxiliary components. The candles soften and melt at the temperature of the human body, ensuring the supply of the active substance, and at room temperature they retain their shape.
Maintaining candles does not require outside help or special medical education, is a non-invasive treatment method, does not cause nausea and vomiting, and in most cases does not cause discomfort. Thanks to these advantages, rectal suppositories have gained popularity and are considered an effective remedy for hemorrhoids.
Like any other dosage form, suppositories also have disadvantages. Firstly, they require storage at low temperatures, often in a refrigerator. Secondly, using candles is not always convenient. Thirdly, some components of suppositories cannot be stored for a long time, so it is not recommended to buy suppositories for hemorrhoids for future use. Remember, candles cannot be used if they are cracked or damaged, or if their color or smell has changed.
Laxatives
The drugs are used for external and internal hemorrhoids. Due to the active components, there is an improvement in intestinal motility, fecal transit, liquefaction of solid formations, and prevention of constipation.
The list includes:
- Guttalax - has a local effect, does not affect the processes of food digestion or absorption. It is prescribed for patients with constipation, dysbacteriosis, or after surgery. Prohibited for use in case of intestinal obstruction, appendicitis.
- Senade – stimulates the process of defecation, is not addictive. Used for constipation, rectal ruptures. Contraindicated for peritonitis, intestinal obstruction, cystitis, strangulated hernia or hemorrhoidal node.
Medicines are prescribed by a doctor strictly according to indications.
Effects of rectal suppositories
Anesthesia
Reduce pain due to analgesic components (novocaine, lidocaine, etc.). Anesthetic suppositories for hemorrhoids are prescribed for acute pain.
Reduce blood clot formation
Achieved through anticoagulants, which block blood clotting mechanisms. After taking such suppositories, blood stops clotting normally, so patients with a tendency to bleed are advised to first consult a doctor.
Anti-inflammatory effect
You can relieve inflammation with the help of non-steroidal anti-inflammatory drugs (aspirin, diclofenac), as well as hormonal drugs (drugs containing glucocorticosteroids). Natural substances (sea buckthorn oil, propolis) are also widely used.
Stop bleeding
In this case, drugs that are opposite in action to anticoagulants are used. That is, they activate the blood clotting process, stop bleeding, but can lead to the formation of blood clots if used uncontrolled.
Strengthening veins
Achieved by increasing their tone, strengthening the wall, and increasing elasticity.
In order to increase the effectiveness of suppositories for hemorrhoids and ensure ease of use, they sometimes include several active ingredients.
For example, suppositories with analgesic, anti-inflammatory and hemostatic effects are popular.
Modern methods of treating hemorrhoids
Etiology
Hemorrhoids (from the Greek haimorrois) literally mean “bleeding.” This disease, known since time immemorial, is still explained ambiguously and sometimes contradictorily, which fully reflects the level of our knowledge about it. Most researchers recognize that the sources of bleeding are cavernous formations, which under normal conditions are formed during intrauterine development.
The first group of hemorrhoidal formations, the defeat of which leads to the formation of external hemorrhoids, is located at the exit from the anal canal, in the subcutaneous tissue.
The second group of cavernous formations, located in the submucosal layer of the rectum, above the dentate line, is the source of the development of internal hemorrhoids.
There are anastomoses between the external and internal cavernous formations, the functional purpose of which is not entirely clear, if only because with an increase in intra-abdominal pressure, as a rule, external rather than internal nodes thrombose. Along with the external and internal sphincter, the cavernous plexuses are part of the obturator apparatus of the rectum. Their ability to increase in volume due to filling with blood allows for an ideal sealing of the intestine. Indirect evidence of this assumption is the ordered arrangement of hemorrhoidal formations around the circumference of the intestine; it corresponds to 3, 7 and 11 o'clock. Unfortunately, this delicate mechanism is very vulnerable and there are many reasons for this. The immediate cause of hemorrhoids is a violation of the blood supply to the cavernous veins, which can be caused by increased arterial blood flow, but more often by a slowdown in venous outflow. The dilated vein forms a “bag of blood”, which is called a hemorrhoid. In recent years, much attention has been paid to studying the condition of the ligamentous apparatus of the submucosal layer of the rectum, the violation of which leads to the prolapse of internal hemorrhoids. Therefore, from the point of view of modern pathophysiology, both variants of the development of the disease should be considered not only as equivalent, but, possibly, as complementary.
Prevalence . Data on the prevalence of hemorrhoids are very contradictory; for example, in Russia this figure ranges from 130–145 cases per 1000 adults [1]. Statistical data provided by foreign researchers is only about 4.4% [2, 3]. The inconsistency of the indicators is most likely due to the difference between morbidity and negotiability, which is indirectly confirmed by data from examinations of US residents, which stated that 80% of people who had hemorrhoids did not complain [4].
Classification of hemorrhoids . The classification was proposed by the State Scientific Center of Coloproctology [1]. It includes the symptoms of the disease, its clinical manifestations and anatomical changes. According to the course of the disease, chronic and acute types of hemorrhoids are distinguished. In shape - internal, external, combined. The chronic course of internal hemorrhoids is divided into 4 stages. It should be emphasized that the clinical symptoms of the disease correspond to the morphological changes occurring in the longitudinal muscle, which fixes cavernous formations in the submucosal layer of the rectum.
In the first stage: bleeding and discomfort are clinically noted, hemorrhoids do not fall out of the anal canal, the vascular pattern of the mucous membrane is enhanced, anatomically - changes in the longitudinal muscle are insignificant.
In the second - bleeding, prolapse of nodes, itching, mucous discharge; prolapsed nodes are automatically reset into the anal canal; histologically in the fibromuscular framework there is unexpressed dystrophy, the number of elastic fibers predominates.
In the third - bleeding, prolapse of nodes, anal itching, mucous discharge. Prolapsed hemorrhoids require manual assistance to reposition them into the anal canal; At the same time, morphological changes in muscle tissue indicate a loss of elasticity, which proves the predominance of dystrophy processes.
In the fourth - bleeding, itching, discomfort, incontinence of the anal sphincter, severe pain; constant prolapse and inability to manually reduce hemorrhoids into the anal canal; which corresponds to complete degeneration of the fibromuscular framework that holds the nodes in the anal canal.
Complications of hemorrhoids . The most common complication of hemorrhoids is thrombosis of hemorrhoids. As a rule, the lesion occurs in the external nodes and quite often thrombosis is the first manifestation of the disease. Precipitating moments for the development of thrombosis most often include pregnancy, childbirth, long air travel, lifting heavy weights, and acute stool disorders. If patients seek help in the first 2 days from the onset of the disease, an enlarged bluish (at an early stage) hemorrhoid, covered with skin and partially mucous, is easily visually detected. More often, the appearance of a node is accompanied by pain, especially intense if two or more nodes are affected. If the size of the node is significant (usually more than 2 cm) with pronounced tension in the mucosal tissue, an area of necrosis appears on it; after rejection of the latter, bleeding develops, sometimes parts of the blood clot may partially come off and the size of the prolapsed formation may decrease significantly. The skin part of the node becomes swollen and hyperemic. Clinically, as a rule, in this case, the patient notes a decrease in pain. Digital examination should begin with examination of the wall of the anal canal opposite to the thrombosed node, which makes the examination more gentle. A digital examination can reveal signs of thrombosis of the internal hemorrhoid. Examination of the anal canal using instruments is carried out only by proctologists.
More rare complications include the formation of a hematoma with a sharp increase in pressure and damage to the wall of the venous vessel. If an internal hemorrhoid prolapses, it may become strangulated. If necrosis of the internal node occurs, massive bleeding is possible, so the patient should be shown to a proctologist. In the event of strangulation of several prolapsed nodes or the occurrence of stool disorders, a purulent process may occur in the perirectal tissue.
Differential diagnosis
Clinical manifestations of hemorrhoids do not differ in the specificity of symptoms. In case of acute hemorrhoids or its complications, these are acute paraproctitis, anal fissure, cryptitis, rectal prolapse. In the case of chronic hemorrhoids, the development of a tumor of the rectum or anal canal should first be excluded. The group of patients who have been suffering from hemorrhoids for a long time, who have come to us due to increased bleeding or unstable stools, is of particular concern in terms of oncological diseases. In case of any treatment of a patient with hemorrhoids to a therapist or general practitioner, it is necessary to refer him for a consultation with a proctologist.
Conservative treatment
The choice of treatment method is usually determined by the stage of the disease or the nature of the complications that have developed.
A special diet for patients with hemorrhoids is not required, except in certain cases. For thrombosis of hemorrhoids, a protein-vegetable diet with a high fiber content and the exclusion of fried and spicy foods, spices, and alcohol is recommended. In patients with concomitant diseases of the colon (irritable bowel syndrome, diverticular disease or nonspecific colitis), the diet should be aimed at normalizing stool. In case of thrombosis of hemorrhoids, accompanied by constipation, patients should be prescribed microenemas to cleanse the intestines. Patients leading a sedentary lifestyle, without exacerbation, should be recommended to play sports, with the exception of weightlifting and cycling. Patients should pay special attention to performing hygienic measures. During the acute period of the disease, it should be recommended to take a cool shower 2-3 times a day and always after stool, and it is necessary to wash not only the skin of the perineum and anus, but also the anal canal itself. In cases where water procedures are not available, the use of special wet sanitary napkins should be recommended.
Systemic drugs . In the conservative treatment of hemorrhoids, one of the leading roles belongs to drugs containing bioflavonoids (diosmin and hesperidin). The use of the latter in the treatment of hemorrhoids is traditional, but with the creation of modern biotechnologies it was possible to obtain Detralex, a micronized drug, which made it more bioavailable and increased the effectiveness of treatment by about 30%. Bioflavonoids have several properties: first of all, they are able to increase venous tone, enhance lymphatic drainage, reduce vascular fragility and improve microcirculation. First of all, the listed qualities make it necessary to use Detralex in the event of thrombosis of hemorrhoids. The drug is prescribed 2 tablets 3 times a day for the first four days, then 1 tablet 4 times for up to 7 days. In addition, Detralex is able to reduce and prevent the development of hemorrhoidal bleeding and exacerbation of hemorrhoids. For preventive purposes, it is recommended to take the drug for up to 6 months, 2 tablets per day. The use of micronized bioflavonoids (the source of which are natural sources, for example, red grape seeds) is possible even during pregnancy, although not for a long time (up to 7 days). The drug is well tolerated and rarely causes allergic reactions. To date, the drug “Phlebodia 600” has been successfully used, which has a prolonged effect, which allows it to be taken once a day. In patients with thrombosis of hemorrhoids, accompanied by severe pain, it is possible to use non-steroidal anti-inflammatory drugs and analgesics, but it is extremely difficult to assess the effectiveness of their effects, so the question of their use should be decided individually in each specific case.
Local therapy . Local treatment is prescribed to relieve inflammation and analgesia. Among the drugs of the first group, we can recommend Posterisan Forte ointment (or suppositories of a similar name). The drug contains a suspension of E. coli culture and hydrocortisone. E. coli metabolites can enhance local immune responses, accompanied by the release of cytokines, especially intraleukin-1. In addition, a suspension of bacterial culture causes the formation of specific immunoglobulin A, which forms a delicate film on the intestinal mucosa, acting as a local protective barrier. Hydrocortisone, which is the second component of the drug, helps to quickly suppress inflammation and accelerates the processes of tissue regeneration induced by a suspension of Escherichia coli culture. The drug is administered rectally 2 times a day; in case of severe inflammatory process, for example, in patients with nonspecific colitis, the frequency of administration can be increased taking into account the frequency of stool. The maximum duration of treatment does not exceed three weeks. If it is necessary to continue therapy, it is possible to use Posterizan suppositories or ointments containing exclusively a suspension of bacterial culture.
Among the drugs that have a complex effect, we recommend Relief Advance suppositories. The composition includes 10% benzocaine, which has a rapid analgesic effect, in addition, shark liver oil containing fat-soluble vitamins, free fatty acids, squalene and alkylglycerol, which are powerful reparants, which allows them to be recommended even for use in the postoperative period in patients who underwent surgery for hemorrhoids. The frequency of administration is 3–5 times a day. The drug is highly effective, well tolerated and rarely produces adverse reactions.
Surgical treatment of hemorrhoids
External hemorrhoids . In addition to conservative treatment of thrombosed hemorrhoids in the first 24–48 hours, until inflammatory changes in the skin part of the node occur, surgical intervention is possible. It is usually performed under local anesthesia and involves removing the hematoma or thrombotic masses, although there is an opinion that it is necessary to remove the entire node along with the affected vein [5]. This tactic is justified in the presence of one (less often two) large nodes or in severe pain. Unfortunately, such operations can not be performed often, because the majority of patients consult a doctor already in the presence of severe inflammation, which sharply intensifies the pain syndrome that existed until that moment. Surgical removal of large external nodes is justified in case of difficulties arising with hygiene, persistent anal itching or after previous thrombosis, although in recent years many patients have turned to a proctologist for aesthetic reasons.
Internal hemorrhoids . Currently, there is a fairly large selection of minimally invasive treatments, used mainly for isolated internal hemorrhoids of stages I–II. True, sometimes the indications for their use can be expanded, mainly in elderly and senile people with severe concomitant diseases. Minimally invasive interventions include: infrared photocoagulation, latex ring ligation and, finally, transanal ligation under Doppler control. The first two of these methods have long been used in clinical practice, and their strengths and weaknesses are well known, so we will dwell in more detail on the last method.
Ligation of hemorrhoidal arteries under Doppler control . The essence of the method is based on the fact that Doppler examination reveals the distal branches of the superior hemorrhoidal artery, supplying blood to the internal hemorrhoids. The necessary equipment is an electronic unit and an anoscope with a Doppler sensor. The method can be used for stages I–III of the disease. The procedure can be carried out in a hospital within one day. The procedure lasts 20–40 minutes, does not require general anesthesia, restrictions on physical activity for about two weeks. Temporary disability is not required for patients. There are no problems with stool in the early postoperative period.
Operation Longo . Prolapse of the mucous membrane of the anal canal with internal hemorrhoidal plexuses, caused by damage to the muscular and ligamentous apparatus of the latter, is accompanied by a disruption of their blood supply and a change in the anatomical relationships between the external and internal nodes. This prerequisite served as the basis for the creation of the Longo operation, which involves tightening the prolapsed mucosa, restoring the anatomical position of the hemorrhoidal plexuses and normalizing their blood flow. The Longo method has been used in clinical practice since 1993, in our country for the last 5 years. The intervention is performed with a disposable set of instruments. The operation is indicated for stages II–IV of hemorrhoids. In our opinion, the advantages of this procedure are most convincing for circular prolapse of nodes. The operation can be performed under conduction or local anesthesia.
Advantages of the method; the duration of the operation is 10–20 minutes, the hospitalization period does not exceed one day, the pain syndrome is well relieved without the use of narcotic analgesics, there is no need for dressings, the patient can return to work in 5–10 days.
Bipolar coagulation of hemorrhoids using the LigaSure device . A modern alternative to classical hemorrhoidectomy is the method of bipolar coagulation of hemorrhoids, which is successfully used in stages III–IV of the disease. The method is based on the principle of bipolar coagulation using a modernized generator equipped with a feedback unit that allows tissue differentiation. In this case, the usual burn of the tissue does not occur, but welding occurs due to the polymerization of its own collagen and instead of the usual scab, the wound is covered with a collagen film. The intervention can be performed under spinal or epidural anesthesia. The intervention technique is simple. The reliability of polymerization guaranteed by the method makes it possible to coagulate vessels up to 7 mm in diameter. The duration of the operation is about 20 minutes. The duration of postoperative treatment is determined by the size of the wound defects of the anal canal. Pain syndrome in the postoperative period is less pronounced than during traditional surgery.
Literature
- Vorobyov G.I., Shelygin Yu.A., Blagodarny L.A. Hemorrhoids. M.: Publishing house "Mitra-Press", 2002. 192 p.
- Johanson JF, Sonnenberg A. The prevalence of hemmhoroids and chronic constipation // Gastroenterology. 1990, 98; 380–386.
- Bayer I., Myslovaty B., Picovsky BM Rubber Band ligation of hemorrhoids: covenient and economic treatment // J. Clin. Gastroentrol. 1966; 23:50–52.
- Haas PA, Haas GP, Schmaltz S., Fox TA Jr. The prevalence of hemorrhoids // Dis. Colon Rectum. 1983; 29: 435–439.
- Corman MI Colon and Rectum surgery, 3rd ed.Philadelphia, Pa: JB Lippincott. 1993: 54–115.
K. E. Mayat , Candidate of Medical Sciences European Medical Center , Moscow
Features of application
When using suppositories, it is necessary to take into account their features and follow some rules:
- Carefully study the instructions for use and pay attention to storage conditions.
- Do not hold the candle in your hands for a long time, as it may begin to melt.
- If suppositories are used once a day, it is best to use them at night. If twice, then in the morning and in the evening.
- It is necessary to insert the suppository with clean hands while lying on your side, after bowel movements and performing hygiene procedures.
You can find out which suppositories for hemorrhoids are best for the patient, as well as how to take them correctly and for how long, after consultation with a specialist.
A comprehensive plan is drawn up individually for each patient, taking into account his age, gender, presence and absence of concomitant pathology and individual characteristics of the body.
Share:
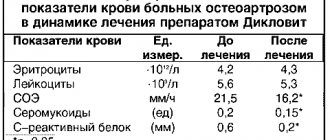
NSAIDs
Medicines are intended to relieve pain and inflammatory processes. When used strictly according to the regimen, they can cause blood thinning, bleeding, and erosions of the gastrointestinal mucosa.
Therapy is carried out:
- Diclofenac – for pinched nodes, thrombosis, complicated forms of pathology, swelling, inflammation;
- Nizom – for pain syndrome, during postoperative recovery;
- Ibuklin - for swelling, pain as a means of rehabilitation.
When treating NSAIDs, you cannot independently change the regimen, increase or decrease the dosage.
How to relieve pain with folk remedies?
At home, the easiest way to get rid of hemorrhoids is with compresses, lotions or sitz baths.
Compresses
To relieve swelling, inflammation, and pain, use ice packs (ice packs on the painful area for 10 minutes every hour). Grate fresh aloe leaves, squeeze out the juice, moisten with a sterile cloth and apply to the inflamed nodes. Grate raw potatoes, wrap the pulp in gauze and place on the sore spot for 10 minutes.
Lotions
Lotions can relieve pain using herbal infusions: chamomile, calendula, nettle, plantain, brachypodium. The herbs reduce inflammation, improve blood circulation around the anus and relieve anal spasms. This helps improve the patient's condition.
Baths
For minor pain, cool sitz baths with the addition of herbal infusions: centanum leaves, aloe vera, nettle, oak bark, celery, algae, calendula.