Causes of hemorrhoids
Inflammation of the anorectal area after childbirth occurs not only as a result of excessive muscle tension and stretching of the hemorrhoidal veins during labor. In many ways, the development of postpartum hemorrhoids depends on the lifestyle of the pregnant woman. Factors that provoke rectal prolapse after childbirth include:
- Sedentary work, insufficient level of physical activity;
- Obesity, overweight;
- Poor nutrition;
- Family history (hereditary predisposition);
- Chronic constipation;
- Frequent stress.
Why is there a problem?
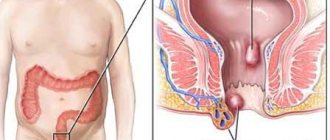
Hemorrhoids in a nursing mother are a common problem. Often the disease develops during pregnancy, especially in its last stages. This is due to the growth of the uterus, which puts pressure on the walls of the rectum. Before the baby is born, symptoms may be absent or mild. The pathology worsens during the birth process, when intra-abdominal pressure increases significantly. The consequence of this process is the formation of nodes and anal fissures, which entails many unpleasant symptoms of the disease.
Another common cause of hemorrhoids in nursing mothers is constipation. Abnormal bowel movements occur due to many reasons. This is diet, stress, an increase in the hormone progesterone. As a result, the digestion process is disrupted, constipation appears, leading to hemorrhoids.
In addition, the following conditions may be factors that provoke the disease:
- low physical activity;
- taking hormonal medications prescribed by a doctor;
- stress, chronic fatigue;
- long labor (more than 12 hours).
Hemorrhoids during breastfeeding can appear as an exacerbation of an existing disease before pregnancy and childbirth. To prevent complications of the disease, you should promptly recognize the symptoms of hemorrhoids and take the necessary measures to treat it.
How do hemorrhoids manifest after childbirth?
Usually the disease occurs in an acute form and is accompanied by the following pathological symptoms and disorders:
- Feeling of heaviness, burning, discomfort and itching in the anus;
- Painful sensations in the anorectal area during bowel movements. Gradually, the pain syndrome intensifies, and the patient begins to experience pain not only during bowel movements, but also when walking.
- The appearance of bleeding during or after bowel movements. The blood may be scarlet or dark in color. Blood clots may appear. Sufficiently heavy and constant bleeding can cause anemia, which negatively affects the patient’s health.
- Enlargement and prolapse of hemorrhoids. Initially, prolapse occurs directly during straining and defecation. In this case, as the pressure decreases, the nodes self-reduce. As hemorrhoids progress, prolapse of the nodes may occur during normal activities (lifting weights, sneezing, etc.).
- The formation of cracks in the anus, which provoke the development of inflammatory processes.
The chronic course of hemorrhoids can lead to strangulation, thrombosis and bleeding of the veins of the hemorrhoids, paraproctitis (infectious inflammation of the rectal tissue) and other complications. To avoid this, when you notice the first signs of hemorrhoids, you must consult a doctor who will prescribe appropriate treatment.
Features of the chronic stage
Getting rid of chronic pathology is much more difficult; sometimes a specialist may resort to surgery. This inflammation is characterized by exacerbation and remission. An exacerbation phase may occur in a woman in the following cases:
- stressful situations (this often happens to young mothers);
- constipation (some women are afraid of defecation due to its painful sensations with this disease);
- poor nutrition;
- sedentary time (during childbirth, genital ruptures are possible, which is why patients are forced to spend most of their time in a supine position).
Treatment depends on the stage of the pathology. So, at the first stage the patient practically does not feel any discomfort. Exacerbations begin, and the patient may complain of a feeling of itching in the anus, bloody discharge that comes out along with the feces. It is at this stage that effective drug treatment must be prescribed in order to avoid surgery.
At the second stage, unpleasant phenomena begin to progress. The patient experiences pain in a sitting position, as well as sharp painful sensations during bowel movements. In the final stages, periodic bleeding occurs, even not associated with bowel movements. Treatment in this case consists of complex drug treatment and surgery, since other methods are sometimes ineffective.
Features of traditional treatment of inflammation of the anorectal area after childbirth
The tactics and treatment regimen for hemorrhoids in women who have given birth differ from treatment in other people. Depending on the needs of the body, the shape and stage of hemorrhoids, as well as the severity of clinical manifestations, treatment of rectal prolapse after childbirth can be carried out using the following methods:
- Physiotherapy. Postpartum hemorrhoids are treated with a set of special exercises that help strengthen muscle tissue. Moderate exercise and walking outside during pregnancy will help prevent hemorrhoids after childbirth.
- Proper nutrition. Following a special diet will ensure the necessary metabolism and restore normal bowel movements. It is necessary to include foods enriched with fiber in your diet. Since constipation can make hemorrhoids worse, normalizing the frequency of bowel movements is very important.
- Treatment using medications (tablets, suppositories, creams, ointments). Their action is aimed at restoring tissue structures and relieving pain.
- Surgical treatment of inflammation of the anorectal region (excision of external hemorrhoids, sclerosis of internal nodes).
Also, women who have given birth and suffer from postpartum hemorrhoids should avoid wearing tight underwear and clothing.
Features of therapy
At the initial stages of the development of postpartum inflammation, conservative methods are used, which may include the following:
- use of candles. Rectal suppositories are the most common means by which both acute and chronic pathologies can be eliminated. Modern suppositories contain extracts of medicinal herbs, as well as painkillers.
- Ointments. If the inflammation is external in nature, special ointments are used that act directly on the source of the pathology. Modern drugs promote rapid healing of perineal cracks.
- Homeopathic remedies. Since many medications are often contraindicated for a woman after childbirth, since their components can pass into milk, homeopathic therapy is most often prescribed. We are talking about candles that contain such harmless ingredients as tea tree oil, calendula extract, chamomile and other herbs. Before starting to use such products, a woman should definitely consult a proctologist, since some such products can cause an allergic reaction.
- Drugs with a laxative effect. This ailment is very often accompanied by constipation, which interferes with a quick recovery. To facilitate the act of defecation, medications containing lactulose may be prescribed. This substance does not cause diarrhea, but helps normalize stool.
- Microclysters made from a decoction of herbs with healing properties also have a good effect.
If there is no desired effect, the proctologist advises the patient to prepare for surgery. With conservative therapy, a large number of medications are prescribed, which can harm the nursing mother. In this case, excision of the nodes is performed under general anesthesia. The ligation technique is considered the most modern type of therapy. During this operation, latex clamps are applied to the base of the knot. After this, the dying hemorrhoidal node disappears on its own.
Diet for hemorrhoids
Women diagnosed with postpartum hemorrhoids should exclude smoked foods, spices, flour and sweet products, as well as peppery and fatty foods from their diet during therapy. White bread should be replaced with other types of bread.
After hemorrhoids are cured, it is important to maintain a balanced and nutritious diet. In this case, you need to eat foods that improve digestion and enhance intestinal motility (fermented milk porridge, dishes rich in plant fiber, buckwheat and rice cereals, vegetable oils). This will ensure regular bowel movements.
The peculiarity of dietary nutrition for postpartum hemorrhoids is that the quality of breast milk should not deteriorate. Therefore, nursing mothers are recommended to eat apples, bananas, dried fruits and other fruits rich in saturated microelements and fiber. You also need fish and lean meat.
You should also control the amount of fluid consumed (at least 1.5 liters per day). It is recommended to abstain from tonic and carbonated drinks.
Treatment of constipation in nursing mothers
Not all pharmaceutical products are suitable for nursing mothers. To choose medications, it is best to consult a doctor. The specialist may prescribe microenemas, rectal suppositories or oral medications.
But most medications can only be used for a short time. Other methods will help normalize stool during breastfeeding.
The doctor's first recommendation for treating constipation during breastfeeding is a balanced diet. Laxatives are prescribed when measures to correct the diet are ineffective or there is a high risk of complications, in cases where constipation requires emergency help.
There is one most important principle of treatment: the development of a morning reflex to bowel movement. It is important to try to maintain a daily routine, setting aside enough time to go to the toilet in the morning immediately after waking up and having breakfast. This can be difficult for a new mother, especially on days when the baby is restless. But you should pay attention to your needs even in this case.
Compliance with the drinking regime is of great importance. During lactation, large amounts of fluid are required, so it is important to drink at least 1.5-2 liters of water per day.
Physical activity improves microcirculation, stimulates intestinal motility, strengthens the muscles of the peritoneum and pelvic floor. You should consult a doctor so that he can suggest light exercises based on your health condition.
Herbal medicine should be selected with care by a nursing mother. There are a number of medicinal herbs approved for use. Herbal decoctions and infusions should be taken according to the recommendations of a specialist.
Laxatives should be prescribed by a doctor. There are not many products allowed for nursing mothers. It is important to avoid taking stimulant laxatives, which are addictive. It is allowed to take bulk laxatives, osmotic agents, and topical medications. There are categories of laxatives that are approved for long-term use and have a beneficial effect on the digestive system of a young mother.
Hemorrhoids after childbirth: basics and specifics of osteopathic treatment
During breastfeeding, most surgical and conservative methods designed to treat hemorrhoids are contraindicated.
The most effective treatment in such a situation is osteopathy. To combat hemorrhoids, an osteopath uses special manual techniques to redistribute the load on the organs and normalize blood flow. Thanks to this effect, osteopathy fights the very cause of hemorrhoids, and not its clinical manifestations.
Osteopathy is an absolutely safe method that allows you to cure hemorrhoids without side effects. It is also advisable to use this method of manual intervention during pregnancy in order to prevent inflammatory processes in the anorectal area after childbirth. The duration of the course of osteopathic therapy is selected by the doctor individually, taking into account the severity of the pathological condition and the patient’s health status.
Osteopathic methods of combating postpartum hemorrhoids
To achieve maximum and lasting results, treatment of rectal prolapse after childbirth is carried out using visceral and structural osteopathy methods. The osteopath pays special attention to the condition of the spine, pelvic bones and coccyx. Slight displacement of the vertebrae can cause pinching of the spinal nerves. This leads to intestinal atony and impaired frequency of bowel movements, which in turn provokes the formation of hemorrhoids, the appearance of congestion in the pelvis and increased pressure in the hemorrhoidal veins. This is why osteopathic work with the spine and bones is so important in the fight against hemorrhoids.
When eliminating congestive processes, an important role is played by diagnosing the pelvic muscles and relieving their spasms, improving lymph flow and blood circulation, restoring the elasticity of the ligaments, as well as working with internal organs.
The effect of manual intervention is noticeable after several sessions. Hemorrhoids stop developing, alarming symptoms disappear, the nodes become smaller and stop bothering the patient.
Surgery and minimally invasive procedures
In the third and fourth stages of hemorrhoids, surgery and minimally invasive procedures are used, since medications are ineffective. When breastfeeding, gentle procedures are carried out that relieve the woman of hemorrhoids and at the same time do not harm the baby.
One of the most popular treatment methods is called cryotherapy. Hemorrhoidal neoplasms are treated with liquid nitrogen. Necrosis of soft tissue occurs under the influence of low temperatures. After a few days, the tumors disappear.
An effective way to treat pathology is latex ligation using rings. During the procedure, a surgical instrument, a ligator, is used. A latex ring is placed at the base of the hemorrhoid. Blood does not enter the node, necrosis occurs, the node dies and disappears.
The procedures are carried out in the private proctology center “Proctologist 81”.
Prevention of postpartum hemorrhoids
In order to prevent recurrent bowel prolapse after childbirth, generally accepted hygiene rules should be followed. After defecation, it is better to use soft toilet paper. If possible, wash with warm water after each bowel movement. You should also follow a proper diet to prevent constipation.
Effective means of preventing the disease include physical therapy exercises. Performing safe and simple physical exercises will help speed up the restoration of vascular tone in the pelvic organs and reduce the time of treatment for postpartum hemorrhoids.
Diagnostics
The diagnosis is made by a coloproctologist. If necessary, your doctor may refer you to other specialists for consultation. For the most successful treatment, seek medical help at the first symptoms. This will also help eliminate the risk of developing other diseases with similar symptoms.
Postpartum hemorrhoids are identified based on:
- patient complaints;
- inspection;
- finger examination;
- laboratory methods: blood test, urine test;
- instrumental diagnostics: sigmoidoscopy, irrigoscopy, colonoscopy, anoscopy.