Without ultrasound data, it is almost impossible to diagnose some diseases. This category includes pathologies of the spleen. Ultrasound of the spleen is a non-invasive and accessible diagnostic method.
CONSULTATION WITH DOCTORS ON THE RESULTS OF ULTRASOUND AND ANALYSIS - 500 rubles!
CLICK TO SIGN UP
With the help of ultrasound diagnostics, it is possible to determine with a high degree of reliability the size of an organ, local and diffuse structures, as well as confirm or refute the presence of neoplasms in it. This diagnostic method is safe and is used for both adults and children.
Indications for ultrasound diagnostics
The content of the article
The spleen (splen) is the largest lymphoid parenchymal organ. It has a peculiar shape of a flat hemisphere. The spleen is located in the upper left part of the abdominal cavity, behind the stomach.
Despite the fact that the organ is not considered vital, it performs the most important functions, which, by the way, are still not fully understood:
- Lymphopoiesis
- the production of antibodies and circulating blood lymphocytes - a kind of filter for bacteria, foreign particles and protozoa. - Destruction of damaged red blood cells and platelets
. The spleen, through the destruction of blood elements, participates in the formation of bile and iron metabolism. - Platelet accumulation
. The organ stores a third of all platelets. - Production of lymphocytes and monocytes
. - Hormonal regulation of bone marrow function
.
The procedure is carried out both for individual indications, in which case the doctor examines this particular organ, and for standard diagnostics of the abdominal cavity. The circulatory system of the spleen is interconnected with the vessels of other organs, and its tissues react to any abdominal pathology, so the organ must be examined during an ultrasound of the abdominal cavity.
Ultrasound of the spleen is prescribed for the following disorders:
- All groups of blood diseases.
- Increased size of the spleen.
- Oncological diseases or suspicion of their presence. Determination of the location and degree of localization of metastases.
- Improper development of the organ. Congenital anomalies (absence of an organ, “wandering” spleen, several spleens, etc.).
- Abdominal injuries.
- Numerous infectious diseases, including sexually transmitted infections (syphilis, malaria, sepsis, typhus, etc.).
- Liver diseases (cirrhosis, hepatitis, etc.). Determination of foci of purulent processes.
- Monitoring the results of prescribed treatment.
Abdominal injuries, falls from heights, and traffic accidents are especially important indications for examining the spleen, since rupture of the organ, accompanied by blood loss, can be fatal.
Causes of splenic infarction
The main cause of the occurrence of a focus of necrosis in the spleen is partial or complete occlusion (blockage) of the splenic artery or its branches. One of the following conditions can lead to the formation of this lesion:
- malignant blood diseases (lymphogranulomatosis, leukemia, lymphoma);
- changes in the physicochemical properties of blood caused by various factors (acquired and congenital pathologies of the coagulation system, hemolytic and sickle cell anemia, erythropoietin therapy, long-term use of oral contraceptives, impaired protein metabolism);
- heart diseases (arrhythmias, myocardial infarction, congenital and acquired valvular defects, septic endocarditis);
- inflammatory and systemic vascular diseases (endoarteritis, atherosclerosis, vasculitis);
- traumatic injuries to the ribs or abdominal organs, which can cause air or fat embolism of the linear vessels;
- parasitic and infectious diseases (malaria, typhoid, sepsis);
- pathology of the spleen (cyst, increased mobility of the organ).
What diseases of the spleen can be detected by ultrasound?
Ultrasound examination of the spleen can detect a number of diseases at the initial stage of pathology development. This explains the value of this survey.
Such pathological changes include:
- Cysts.
- Malignant, benign tumors.
- Abscess (purulent inflammation, life-threatening)
- Necrosis (death) of tissue.
- Mechanical damage that can lead to organ rupture or hematoma (hemorrhage, bruise).
- Inflammation.
- Sepsis (blood poisoning).
- Mononucleosis.
Despite the fairly short list of pathologies, most of them can be fatal if left untreated.
Classification
So, what is splenic infarction? This is an area of necrosis that forms in the organ, the development of which is caused by impaired blood flow in the system of lienal (splenic) vessels. Depending on the type of these disorders, two types of heart attack are distinguished:
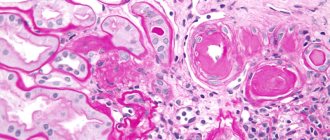
- Ischemic. Occurs as a result of blockage of the splenic artery or one of its branches (thrombosis, embolus) or disruption of blood flow caused by severe vascular spasm. As a result, blood stops flowing to the tissues of the spleen, which is accompanied by hypoxia and ischemia, and subsequently the formation of a focus of necrosis. With this form of the disease, the spleen or parts of it (macropreparation) become pale yellow. If you examine organ tissue under a microscope (microscopic specimen), you can identify foci of inflammatory infiltration.
- Hemorrhagic. When a branch of the linear artery is blocked, blood is discharged into the collateral vessels, which leads to an increase in pressure in them. As a result, the vessel ruptures and blood flows into the parenchyma of the organ. The histological description indicates that the organ has a bright red color due to the shedding of blood; clearly defined foci of necrosis and infiltrates are identified in it.
The disease predominantly affects older people (over 60 years old), equally women and men.
Depending on the extent of the pathological process, the presence or absence of complications, a heart attack takes the following forms:
- extensive;
- finely focal;
- multiple;
- unit;
- uncomplicated;
- septic.
Preparation
Ultrasound of the spleen is performed in the morning, on an empty stomach. The most accurate result of the study is possible subject to high-quality preparation for the procedure:
- The last meal should be at least 7-8 hours before the examination. An exception is for patients with diabetes: they are allowed to have a light snack in the morning (ideally tea with crackers).
- 2 days before the procedure, it is necessary to adjust the diet - exclude foods that contribute to gas formation (beans, raw vegetables, black bread, carbonated drinks, dairy products, etc.). This is necessary to prevent fermentation in the intestines: air prevents inspection of the spleen and distorts the result.
- It is recommended to take sorbents and enzyme preparations that stimulate digestion (smecta, festal, mezim, etc.).
- If a person has increased gas formation, then he is additionally advised to take activated charcoal on the eve of the procedure. The dosage is calculated individually at the rate of 1 tablet per 10 kg of body weight.
- Smoking and drinking alcohol are prohibited at least 24 hours before the procedure, as this can cause stomach spasms, which in turn will distort the results.
Preparing for an ultrasound of a child is somewhat more complicated, since he needs to be prepared not only physically, but psychologically. Although this procedure is completely painless and safe, the child may experience overwhelming anxiety and fear. It is possible to reduce the examination procedure to a kind of game.
There are also difficulties in the area of nutrition. Children do not always tolerate hunger well, especially for infants and children under 3 years of age. A pause in feeding a baby must be made 3 hours before the ultrasound, in children 2-3 years old - 4 hours, over 3 years old - at least 6 hours. Do not drink for 1 hour.
How is the procedure performed?
The duration of an ultrasound examination of the spleen does not exceed 15 minutes. The patient can receive the results of the examination immediately after the procedure. The examination is carried out as follows:
- The patient lies on the couch with his back and exposes his stomach.
- The doctor applies a special gel to the abdomen, which improves the glide of the sensor and the penetration of ultrasonic waves deep into the tissue.
- A specialist performs an examination. The sensor is located along the midline of the abdomen, shifted to the left by 10 cm, and then parallel sections are made. Afterwards, the doctor changes the direction of movement from the costal arch to the lower pole of the spleen.
- The received data is decrypted.
With congenital anomalies of the spleen, even if this is a conditional norm of development, difficulties may arise in performing the procedure. The solution to the problem is to conduct an ultrasound of the spleen through the intercostal space. To do this, the patient needs to take a certain position: lie on his right side, raise his left hand behind his head, then take a deep breath and hold his breath - in this state the doctor examines the condition of the organ.
If no suspected pathologies have been identified, the ultrasound continues with the patient in the prone position.
How is the examination carried out?
Tomography is performed in the diagnostic room. The patient needs to wear clothes without metal inserts. You need to lie down on a retractable table. When performing contrast-enhanced MRI, the drug is first administered intravenously.
To prevent movement during diagnostics, doctors need to secure the limbs using special belts. The duration of the manipulation is about 40 minutes. The machine may make loud noises during the scanning process, so it is often recommended to use earplugs.
Interpretation of ultrasound of the spleen: normal indicators
Normal ultrasound findings of the spleen look like this:
- Echogenicity: average.
- The size of the splenic vein is no more than 0.5 cm (in diameter).
- Possible presence of a vascular network in the area of the organ's hilum.
- Shape: sickle-shaped.
- Location: in the abdominal cavity, in the left upper quadrant (between the diaphragm and the stomach).
- Localization of the stomach: at the center of the spleen (or slightly lower).
- Location of the tail of the pancreas: at the middle of the hilum of the organ.
- Localization of the left kidney: just below the spleen in the middle.
- Size: with an oblique cut - within 12 cm, with a transverse cut - up to 8 cm, thickness - about 4 cm.
- Weight: 150-250 g.
- The structure of the parenchyma is homogeneous, the contour is continuous.
Spleen size in children
In children, the normal size of the spleen depends not only on age, but also on height, therefore individual fluctuations in indicators in children are acceptable within 10% of the age norm. The sizes of the organ for children of different ages are presented in the table.
| Age | Length (mm) | Thickness (mm) |
| Newborn | 45 | 20 |
| 1 year | 52 | 25 |
| 3 years | 65 | 30 |
| 5 years | 75 | 35 |
| 7 years | 90 | 40 |
| 10 years | 105 | 50 |
| 14 years | 130 | 55 |
If the indicators go beyond the normal range, the following pathologies may be suspected:
- hematological syndrome.
- anemia.
- leukemia.
- Congenital heart defect.
- typhoid fever.
- tuberculosis.
Often, an enlarged spleen in children indicates liver problems.
Pathological indicators of the spleen: list of changes by disease
| Deciphering the pathology | Indications of the study |
| Leukemic infiltration | Increased size of the spleen. Pointed edge. Excessive contour convexity. Increased parenchyma density. Inflammation of the lymph nodes at the organ's gates. Strengthening the echo structure. |
| Abscess | Transformation of the echostructure (mixed or hypoechoic). The appearance of a cyst (on ultrasound it looks like an oval formation with uneven contours). |
| Hematoma | Mixed or anechoic echostructure. Uneven boundaries of the spleen contour. |
| Gap | The appearance of fluid in the abdominal cavity or under the diaphragm. Irregular, uneven contour of the organ. |
| Heart attack | A thickened or thinned area on the spleen tissue has been identified. |
Some diseases cannot be seen directly after an ultrasound examination of the spleen, but the doctor is able to determine them by the area of the largest oblique section. To find it, you need to multiply the largest linear dimension by the smallest. The norm for this indicator is 15.5-23.5 cm2.
Alternative Research
In medicine, there are many methods for examining the spleen:
- Ultrasound.
- Computed and magnetic resonance imaging.
- Radionuclide scanning.
- Puncture.
Ultrasound of the spleen has many advantages over other methods.
- Painless – the study does not require invasive procedures. Then, like a biopsy (tissue sampling for further analysis), although it is carried out with anesthesia, the procedure is still unpleasant.
- Short duration - obtaining the necessary information about the condition of the organ and making a preliminary diagnosis takes only 15 minutes.
- It has no contraindications, which allows the procedure to be performed many times. And this is very convenient for monitoring the course of the disease and adjusting treatment.
- Affordable cost – ultrasound has the lowest price among all methods.
CT or MRI of the spleen
A CT scan is often performed if emergency diagnosis is necessary for serious injuries and damage. Manipulation allows you to accurately determine the relative position of internal organs and identify changes. Computed tomography can detect malignant and benign formations, infections and inflammations.
MRI is used primarily to assess changes in soft tissues. This method allows you to most accurately determine the real state of tissues and organs and see any deviations. In each specific case, the examination method is chosen by the doctor, taking into account the patient’s existing problems.