Rules for measuring blood pressure in children
It is preferable to measure blood pressure at home with an automatic or semi-automatic tonometer, the use of which will greatly facilitate the procedure and eliminate the influence of the human factor. It is important to select the correct cuff as measuring with an adult cuff will give incorrect results. The dimensions of the cuff depend on the age of the child and are: for infants - 3.5x7 cm; from 1 to 2 years – 4.5×9 cm; from 2 to 4 years – 5.5×11 cm; from 4 to 7 years – 6.5×13 cm; from 7 to 10 years – 8.5×15 cm; from 10 and older - an adult cuff is suitable.
It is best to measure blood pressure in the morning, 15-20 minutes after waking up or resting. The child should take a comfortable position (lying or sitting), be calm and relaxed. The hand on which the measurement will be taken should be at heart level and free of clothing. Next, a cuff is attached to the arm 2-3 centimeters above the elbow, and depending on the type of device, measurements begin. If this is an automatic tonometer, then just press the power button and air will automatically be pumped into the cuff and after a few seconds the result will appear on the device display. In a semi-automatic tonometer, air is pumped and released using a bulb. For a more reliable result, you should measure the pressure 3 times with an interval of 2-4 minutes and calculate the average value.
LIST OF ABBREVIATIONS
AH - arterial hypertension BP - blood pressure BP av - mean hemodynamic pressure DBP - diastopic blood pressure IV - time index PI - area index CV - coefficient of variation PBP - pulse arterial pressure SBP - systolic blood pressure SI - 24-hour ABPM index - 24-hour blood pressure monitoring pressure CO – standard deviation Av – average value HR – heart rate ECG – electrocardiogram.
The origins of hypertension in adults, according to many authors, are in childhood, but the nature and time of development of arterial hypertension in children are not well known. In addition, the proportion of children with low blood pressure has recently increased. In this regard, an urgent task in pediatrics is to improve the quality of early diagnosis of hyper- and hypotensive conditions.
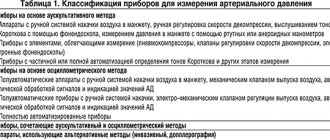
In order to adequately assess blood pressure levels, it must be correctly measured and compared with standard values. N.S. Korotkov’s method, proposed in 1905 by our compatriot, has historically proven its clinical significance for diagnosing and predicting the course of arterial hypertension. However, accumulated experience shows that one-time measurements do not always reflect true blood pressure, do not take into account the “white coat hypertension” effect, and do not provide an idea of the circadian rhythm of blood pressure.
The possibility of continuous 24-hour recording of blood pressure in patients has long attracted doctors of various specialties. The invasive intra-arterial method (Oxford system through a catheter in the brachial artery), despite its high accuracy and continuity of measurement, is not widely used due to the high risk of complications.
Noninvasive intermittent but repeated blood pressure measurements using the Korotkoff auscultatory method, the oscillometric method, or a combination of both have been used for about 30 years.
The oscillometric method used in most blood pressure monitors has been known for a long time: one of the first devices for recording arterial oscillograms was designed by L.I. Uskov in 1904. However, widespread practical use of this method in medicine became possible in the 80s thanks to progress in computer technology. Numerous semi-automatic and automatic devices for one-time blood pressure measurements and monitors for daily blood pressure monitoring have appeared.
Self-measurement of blood pressure by patients has become widespread. Numerous studies have confirmed that blood pressure measured by nurses, the patient himself or an automatic device is lower than that measured by a doctor. Comparison of 24-hour blood pressure monitoring data with random measurements showed that about 40% of patients receive excessive antihypertensive treatment.
According to many authors, in approximately a third of adolescents with arterial hypertension identified during random blood pressure measurements, elevated blood pressure was also recorded during ABPM.
If in adults ABPM has been used for a long time and seriously for diagnosing hypertension and monitoring antihypertensive therapy, then in children this is a relatively new direction.
Suitable tonometers for measuring
It is not necessary to buy a separate blood pressure monitor for a child; it is enough to purchase a children’s cuff. When purchasing a tonometer, pay attention to its functionality. For a large family, it is worth choosing a tonometer with measurement memory for two users with recording of measurement time. This will help track the slightest deviations in pressure from the norm. For hypertensive patients, morning hypertension monitoring functions and a high blood pressure indicator will not be superfluous.
Tonometer Omron M1 Eco Approximate price: 1,700 rubles
- semi-automatic tonometer;
- memory for 42 results + date and time registration;
- indicators of arrhythmia and high blood pressure;
- calculation of the average blood pressure value from the last three results;
- large display.
Tonometer Omron M10-IT Approximate price: 8,900 rubles
- automatic tonometer;
- memory for 2 users for 84 measurements + guest mode;
- indicators of movement, arrhythmia, high blood pressure;
- the presence of a function for calculating the average blood pressure value from three measurements;
- It is possible to connect to a computer.
DESCRIPTION OF THE METHOD
METHOD FORMULA: a method is proposed for assessing the circadian rhythm of blood pressure in children in natural conditions using wearable blood pressure monitors in order to improve the quality of diagnosis of hypertensive and hypotensive conditions in pediatrics.
The novelty of the proposed method lies in the fact that for the first time, standards for the parameters of daily blood pressure monitoring are proposed for children of various ages, highlighting the 5th, 90th, 95th percentile of blood pressure for adolescents 13–15 years old. For the first time, for calculating ABPM parameters, values of the 95th percentile of blood pressure are proposed individually for each child, taking into account gender, age and height.
ANNEX 1
24-hour BP monitoring diary
Child's full name _________________________________________________
Date of birth _________________ Age (years) ____________________
Weight ___________ Height __________ Body mass index (kg/m2) __________
FULL NAME. mother of the child _____________________________________________________
Address: ________________________________________________________
Telephone: ______________________________________________________
Study start date ________ Study start time ________
Cuff: on the right hand on the left hand.
Prescriptions (drug, dose) – _____________________________________
| Time | Kind of activity | Complaints | |||||||||
| (hour) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Notes |
| 06–07 | |||||||||||
| 07–08 | |||||||||||
| 08–09 | |||||||||||
| 09–10 | |||||||||||
| 10–11 | |||||||||||
| 11–12 | |||||||||||
| 12–13 | |||||||||||
| 13–14 | |||||||||||
| 14–15 | |||||||||||
| 15–16 | |||||||||||
| 16–17 | |||||||||||
| 17–18 | |||||||||||
| 18–19 | |||||||||||
| 19–20 | |||||||||||
| 20–21 | |||||||||||
| 21–22 | |||||||||||
| 22–23 | |||||||||||
| 23–24 | |||||||||||
| 00–01 | |||||||||||
| 01–02 | |||||||||||
| 02–03 | |||||||||||
| 03–04 | |||||||||||
| 04–05 | |||||||||||
| 05–06 | |||||||||||
where, types of activities: 1 – sleep, 2 – eating, 3 – taking medications, 4 – lying down, 5 – emotional stress, 6 – physical activity; complaints: 7 – headaches, 8 – dizziness, 9 – palpitations, 10 – fatigue
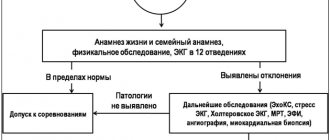
INDICATIONS AND CONTRAINDICATIONS FOR THE USE OF THE METHOD
The main indications for ABPM are:
1. Arterial hypertension.
2. Arterial hypotension.
3. Syncope.
4. Short-term, difficult to register during random measurements, fluctuations in blood pressure.
5. White coat hypertension.
6. Hypertension refractory to drug therapy.
There are no absolute contraindications to the use of the ABPM method in pediatrics. Possible complications include:
1. Swelling of the forearm and hand.
2. Petechial hemorrhages.
3. Contact dermatitis.
In order to prevent the occurrence of petechial hemorrhages, ABPM should not be administered to children with thrombocytopenia, thrombocytopathy and other disorders of vascular-platelet hemostasis during an exacerbation. To prevent the development of edema of the distal part of the limb and contact dermatitis, the cuff should be placed not on the bare shoulder, but on the sleeve of a thin shirt.
MATERIAL AND TECHNICAL SUPPORT OF THE METHOD
1. Devices for daily monitoring of blood pressure and pulse:
1.1. Ambulatory monitor for measuring blood pressure Meditech ABPM-02 (Meditekh, Hungary), registered with the Ministry of Health of the Russian Federation under No. 95/192.
1.2. 24-hour blood pressure and ECG monitoring system MEDSET with SCANLIGHT-recorder and CARDIOLIGHT-recorder recorders, SCANLIGHT-CARDIOLIGHT PC-Software programs, patient cable, SCANLIGHT cuff and Medset Battary Changer-Set device, (company “MEDSET Medizintechnik GmbH”, Germany) registered in the Ministry of Health of the Russian Federation for No. 97/323.
1.3. 24-hour ECG and blood pressure monitoring system “Cardiotechnika-4000 AD” (INKART company, St. Petersburg, Russia), registered by the Ministry of Health of the Russian Federation under No. 95/311-51.
2. Personal computer with printer.
Characteristics of monitors and methods for studying the circadian rhythm of blood pressure in children
Currently, for daily monitoring of blood pressure in children, monitors are used that use various methods of measuring blood pressure: auscultatory, oscillometric, with a combination of these methods, as well as synchronization with an ECG. More accurate, but also much more expensive, are devices with a combination of auscultatory and oscillometric methods, as well as those using synchronization with an ECG: when each air fluctuation in the cuff is correlated with the ECG.
In auscultation monitors, a miniature microphone placed above the brachial artery records Korotkoff sounds. In this case, it is necessary to accurately position the microphone, which is often difficult for children. The sensor is very sensitive to external noise and the slightest displacements. The patient or his parents will not be able to accurately position the microphone on their own, so it is not advisable to remove the cuff and sensor. In addition, the hyperkinetic type of blood circulation predominates in children, in which the “endless tone” phenomenon is often observed, making it difficult to determine diastolic blood pressure by auscultation.
Currently, the most widespread in terms of price/accuracy are monitors with oscillometric blood pressure measurement.
The ABPM-02 devices (AVRM-02, AVRM-02/M and AVRM-02/0) and SCANLIGHT-II use the oscillometric method of measuring blood pressure. The sensor is the entire cuff, therefore the method is insensitive to noise, to displacements of the cuff, which can even be removed between measurements independently by the patient or parents and put on again without compromising the accuracy of the measurements.
The device automatically pumps air into the cuff with a built-in compressor to a pressure of 20–30 mmHg. above systolic blood pressure and then slowly, stepwise, reduces the pressure below diastolic. Arterial pulse waves are transmitted through the cuff and recorded by a capacitive or piezoelectric pressure sensor.
The new blood pressure recording algorithm used in the AVRM-02/M and AVRM-02/0 devices has a new, higher degree of resistance to external mechanical interference, arising, for example, due to involuntary movements of the hand. The essence of the algorithm is step-by-step decompression and registration of several fluctuations at each level of pressure in the cuff. If registration of oscillations at any level is unsuccessful, the device returns to it and repeats the measurement.
As the pressure in the cuff decreases, the first recorded fluctuation is estimated as systolic blood pressure. The maximum oscillation corresponds to the average hemodynamic blood pressure. The last recorded oscillation is considered as diastolic blood pressure. Blood pressure values are related by the formula:
BPsr = DBP + 1/3 (SBP - DBP)
Programming monitors (measurement plan)
The measurement plan provides for the establishment of day and night periods: as a rule, 06.00–24.00 – day, 00.00–06.00 – night. Frequency of measurements during the day: 1 time per 15 minutes, at night: 1 time per 30 minutes. (less frequent measurements will not give an idea of the high variability of blood pressure in children, and more frequent measurements during the day do not increase the accuracy of the study, and at night can cause sleep disturbance).
To clarify sleep time, you should recommend that your child press the “event” button on the monitor when he goes to bed and when he wakes up. According to our observations, the beginning of the night period is approximately 1 hour after, and the day time period is 1 hour before the “event”. You can focus on the heart rate graph: when you fall asleep, there is a sharp decrease in heart rate, and when you wake up, it increases. Using the heart rate chart, you can indirectly control the depth of sleep: if a significant increase in heart rate was observed at night, it means that your sleep was restless. When statistically processing data, shifting the daily period by ±1 hour does not affect the average values. Editing the duration of day and night intervals is also possible after entering data from the monitor into the computer.
When programming monitors, it is necessary to select the appropriate cuff size, turn off the warning sound, and turn off the display so that the results of routine measurements are not displayed - to reduce the increased attention of children to the device and prevent anxiety from the high blood pressure values obtained.
Method of installing the monitor on the patient
The monitor is placed in a case and secured to the patient using two tapes: one goes over the shoulder, the other is located at the waist. Some instructions recommend removing the monitor from the patient at night and, connecting it with a longer tube to the cuff, laying it next to it. However, children sleep more restlessly than adults and often the tube gets wrapped around the child and becomes bent, disrupting the measurement process. In our opinion, during the study the child should not remove the monitor at night.
The cuff is selected in accordance with the circumference of the child's shoulder, measured at the middle of the distance between the olecranon and humeral processes (Table 1). The use of cuffs on the forearm or finger is not adequate and cannot yet be recommended for widespread use in pediatric practice.
Table 1. Selection of a cuff depending on the size of the child’s shoulder
| Shoulder circumference (cm) | Dimensions of rubber balloon cuff (cm) | Dimensions of the cuff cover (cm) |
| Less than 24 | 6x28.5 | 9 x 41 |
| 24 – 32 | 12.5x22.5 | 16 x52 |
| More than 32 | 14.5 x 32 | 16x70 |
To prevent unpleasant sensations associated with the duration of measurements (sweating, rubbing, etc.), it is allowed to place the cuff over a thin shirt or T-shirt with sleeves. This does not affect the accuracy of measurements. The cuff is secured so that the tube connection or “arteria” mark is approximately above the brachial artery. The outlet tube should be directed upward so that the patient can put other clothing over the cuff, if necessary.
After installing the monitor, it is necessary to explain to the child the rules of behavior at the time of measurement and demonstrate one measurement. The child learns that the measurement has begun by the compression of the shoulder due to the increase in pressure in the cuff. At this moment, it is necessary to avoid sudden movements: stop if the child is walking or running, lower the arm with the cuff along the body, relax the arm muscles as much as possible, and do not move the fingers. If the child was sitting or lying down, you should leave the arm in the position in which it was (preferably, the cuff should be at the level of the heart).
As a rule, planned measurements are accompanied by a smooth injection of air into the cuff and a stepwise decrease in pressure. Sometimes, if the measurements are unsuccessful, the monitor, after reducing the pressure, pumps air into the cuff again. It is necessary to explain to the child that until the air is quickly and completely released from the cuff, one must remain calm.
The monitors are equipped with an “extraordinary measurement” button, which can be recommended to the child to press if an attack of headache, pain in the heart, dizziness, etc. occurs. At this moment, an extraordinary measurement of blood pressure and heart rate will occur, recording it in memory and displaying the results on the display for taking emergency measures, if necessary.
You should explain to the child that he should not think about the monitor, listen to its work, or worry about night measurements. At the same time, the child must exercise certain caution: avoid intense physical activity and sudden movements. The monitors are equipped with protection systems: in the event of a sudden increase in pressure, the emergency valve will release air. In addition, there is a button to interrupt the measurement. As a rule, children, especially adolescents, are very responsible about blood pressure monitoring. According to our data, the percentage of measurements available for calculations usually exceeds 95%. Nighttime blood pressure monitoring usually does not bother children.
For diagnostic purposes, it is important that the child, when conducting 24-hour blood pressure monitoring, is in his normal rhythm of life, and in case of intense physical, emotional or mental stress, he (or his parents) makes an appropriate entry in the diary (Appendix 1). When assessing the effectiveness of therapy, the child during ABPM should be in approximately the same conditions before and during treatment.
Evaluation of monitoring data
A wide selection of modern computer programs provides great opportunities for editing and evaluating monitoring results. This data can be presented in graphical form (graphs, histograms) or as a statistical report. It should be emphasized that data editing according to the patient diary is an important preparatory procedure to eliminate possible measurement artifacts.
The graphical form is most convenient for visual assessment of the daily profile and blood pressure variability. To smooth out random fluctuations in blood pressure, graphs of average values, Fourier transforms, polynomial analysis (polynomial of degree 5–6), and cosinor analysis are used. ABPM data can be transposed into Excel (Windows) and analyzed by this program.
When analyzing data obtained from daily monitoring of blood pressure, the most informative are the following groups of parameters: average blood pressure values, time indices of hypertension and hypotension, indices of the area under the blood pressure curve, indicators of blood pressure variability. For all parameters, values are calculated both for 24 hours and for individual periods of time (day, night or arbitrary intervals).
Average blood pressure values (systolic, diastolic, average hemodynamic, pulse) give the main idea of the patient’s blood pressure level and more accurately reflect the true level of hypertension than single measurements.
Until recently, normal limits for daily blood pressure monitoring in the pediatric population, based on a sufficient number of studies, were not established in Russia. Abroad, this problem is receiving more attention. In 1997, MSSoergel et al determined the appropriate mean BP values in children and adolescents based on 24-hour monitoring in a multicenter study including 1141 children. Considering that BP values correlate better with body length than with age, the 50 and 95 percentiles of BP were given taking into account the child’s height (Table 2).
Table 2. Values of the 50th and 95th percentile of blood pressure according to 24-hour monitoring in children and adolescents depending on height (MSSoergel et al., 1997)
| Height (CM)/ n | Percentile BP Day | Percentile BP Day | Percentile BP Night | |||
| 50 | 95 | 50 | 95 | 50 | 95 | |
| boys | ||||||
| 120(33) | 105/65 | 113/72 | 112/73 | 123/85 | 95/55 | 104/63 |
| 130(62) | 105/65 | 117/75 | 113/73 | 125/85 | 96/55 | 107/65 |
| 140(102) | 107/65 | 121/77 | 114/73 | 127/85 | 97/55 | 110/67 |
| 150(105) | 109/66 | 124/78 | 115/73 | 129/85 | 99/56 | 113/67 |
| 160(115) | 112/66 | 126/78 | 118/73 | 132/85 | 102/56 | 116/67 |
| 170(83) | 115/67 | 128/77 | 121 /73 | 135/85 | 104/56 | 119/67 |
| 180(69) | 120/67 | 130/77 | 124/73 | 137/85 | 107/55 | 122/67 |
| girls | ||||||
| 120(40) | 103/65 | 113/73 | 111 /72 | 120/84 | 96/55 | 107/66 |
| 130(58) | 105/66 | 117/75 | 112/72 | 124/84 | 97/55 | 109/66 |
| 140(70) | 108/66 | 120/76 | 114/72 | 127/84 | 98/55 | 111/66 |
| 150(111) | 110/66 | 122/76 | 115/73 | 129/84 | 99/55 | 112/66 |
| 160(56) | 111/66 | 124/76 | 116/73 | 131/84 | 100/55 | 113/66 |
| 170(105) | 112/66 | 124/76 | 118/74 | 131/84 | 101/55 | 113/66 |
| 180(25) | 113/66 | 124/76 | 120/74 | 131/84 | 103/55 | 114/66 |
Based on a survey of 240 adolescents aged 13–15 years, we obtained normative values for ABPM indicators. Blood pressure values corresponding to the 5th, 90th and 95th percentile are highlighted. The data is presented in Table 3.
Values between the 90th and 95th percentiles should be considered “high normal BP.” Isolating the concept of “high normal blood pressure,” on the one hand, allows us to avoid overdiagnosis of hypertension and does not cause mental trauma to the child and his parents, on the other hand, it involves identifying a group at risk for the possibility of developing hypertension, requiring preventive measures and dynamic monitoring. Blood pressure values above the 95th percentile were taken as arterial hypertension. Blood pressure values below the 5th percentile were taken as arterial hypotension.
The time index (TI) of hypertension or “proportion of elevated blood pressure” allows you to estimate the time of blood pressure increase during the day. This indicator is calculated by the percentage of measurements exceeding normal blood pressure readings over a 24-hour period or separately for each time of day. For the maximum permissible value of blood pressure in children during the daytime, we took the values of the 95th percentile for the corresponding gender, age and height, calculated according to our own nomograms (Appendix 2). The maximum permissible value of blood pressure at night was taken to be 10% less than during the day.
Table 3. Indicators of 24-hour blood pressure monitoring in adolescents aged 13–15 years
| Time | Options | Percentiles | Maximum | Minimum | Average | s | ||
| 5 | 90 | 95 | ||||||
| Girls (average age 14.3 years) | ||||||||
| Day | GARDEN | 87 | 123 | 126 | 165 | 63 | 105,8 | 12,8 |
| (24 hours) | DBP | 45 | 76 | 78 | 100 | 35 | 60 | 11,1 |
| Day | GARDEN | 96 | 128 | 131 | 165 | 79 | 112 | 12,3 |
| (8.00–22.00) | DBP | 53 | 79 | 82 | 100 | 36 | 63 | 10,3 |
| Night | GARDEN | 79 | 113 | 116 | 136 | 63 | 96,8 | 10,3 |
| (00.00–06.00) | DBP | 47 | 64 | 66 | 74 | 35 | 54 | 7,3 |
| Boys (average age 14.1 years) | ||||||||
| Day | GARDEN | 94 | 131 | 134 | 166 | 80 | 113,2 | 13,3 |
| (24 hours) | DBP | 49 | 78 | 80 | 107 | 38 | 63,4 | 10,6 |
| Day | GARDEN | 98 | 134 | 136 | 166 | 85 | 117,8 | 13,2 |
| (8.00–22.00) | DBP | 55 | 80 | 83 | 107 | 41 | 67,5 | 9,5 |
| Night | GARDEN | 86 | 115 | 117 | 144 | 80 | 101,4 | 11,4 |
| (00.00–06.00) | DBP | 48 | 67 | 69 | 74 | 38 | 57,2 | 8,1 |
A time index greater than 25% for SBP is clearly considered pathological. In this case, a diagnosis of hypertension is made. With stable hypertension, the AI of hypertension approaches 100% and loses its informative value. In this case, the area index or pressure load is determined. The area index is calculated as the area of the figure limited by the curve of high blood pressure and the level of normal blood pressure (in mmHg*hour/day). The area index reflects the hypertensive load acting on the patient’s body, that is, for how long in 24 hours (or per day, night) and on average by what amount the blood pressure exceeded the upper permissible limit.
When calculating the “hypotension index,” the percentage of time when blood pressure was below the 5th percentile for age and gender is calculated.
The normative values of PV and PI obtained in our study during 24-hour blood pressure monitoring are presented in Table 4.
Table 4. Time index and area index standards for adolescents aged 13–15 years
| Options | Day | Night | ||||
| GARDEN | DBP | BP avg. | GARDEN | DBP | BP avg. | |
| Girls | ||||||
| IV (%) Less | 20 | 15 | 15 | 15 | 10 | 10 |
| PI less than mmHg*hour | 25 | 20 | 15 | 10 | 10 | 10 |
| Boys | ||||||
| IV (%) Less | 25 | 15 | 10 | 10 | 10 | 10 |
| PI less than mmHg*hour | 15 | 15 | 10 | 10 | 10 | 10 |